Bicycling? Orthopedic surgeon shares tips to protect your hands, wrists and head
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
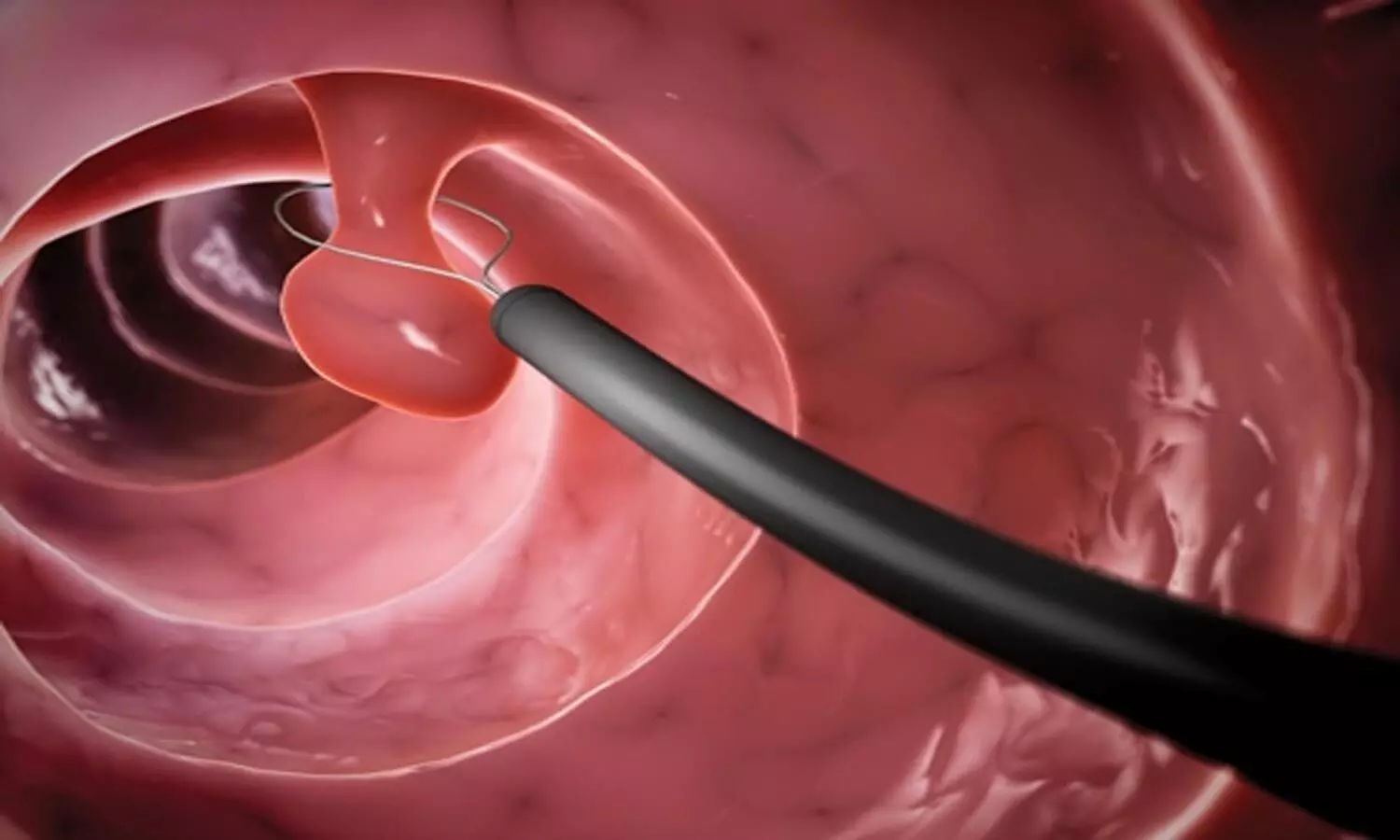
Fasting and bowel preparation before colonoscopy can lead to intravascular volume depletion, but rigorous assessment of its clinical implications is limited. Recent prospective cohort study was conducted to evaluate the relationship between intravascular volume status and hypotension during propofol sedation for elective colonoscopy. The cohort included adult patients undergoing colonoscopy following polyethylene glycol (PEG) bowel preparation. Using a combination of transthoracic echocardiography (TTE) and ClearSight noninvasive monitoring, the study aimed to assess pre-procedural volume status and monitor intraprocedural hemodynamics.
Patient Analysis
Among the 99 patients analyzed, 32% exhibited signs of intravascular volume depletion based on TTE assessments following a passive leg-raising test. The study observed inadequate agreement between TTE and ClearSight measurements of stroke volume at baseline and post-leg raising, casting doubt on the reliability of the noninvasive monitor alone in determining volume status. Notably, significant intraprocedural hypotension, defined as a mean arterial pressure below 60 mm Hg, was more prevalent in patients identified as fluid-responsive compared to those who were normovolemic (48% vs. 21%, respectively).
Demographic Insights
The lack of significant association between demographic variables (age, ASA status, antihypertensive therapy) and fluid responsiveness suggests that other factors may be influencing intravascular depletion. Fasting durations for fluids and food averaged 9 hours and 25 hours, respectively, which aligns with established guidelines, yet the risks associated with fasting and required bowel preparation persist.
Monitoring Implications
The study emphasizes that while individuals undergoing colonoscopy may frequently display signs of fluid responsiveness, their hemodynamic stability remains questionable, especially under sedation’s influence. Propofol’s vasodilatory effects amplify this concern, suggesting a need for vigilant monitoring during procedures. Though current recommendations encourage intravenous fluid administration as a preventive strategy against hypotension, its efficacy continues to be debated.
Conclusions and Future Directions
Overall, the findings underscore a critical gap in understanding the clinical impacts of bowel preparation-induced volume depletion during colonoscopy. The study suggests a need for further investigation into the optimal management of intravascular volume status pre-procedurally and the overall necessity of advanced monitoring approaches in outpatient endoscopic settings to mitigate adverse outcomes.
Key Points
– A prospective cohort study assessed the impact of fasting and bowel preparation on intravascular volume status and hypotension during propofol sedation in elective colonoscopy, revealing that volume depletion may lead to significant hemodynamic instability.
– Transthoracic echocardiography (TTE) indicated that 32% of the 99 patients studied exhibited signs of intravascular volume depletion after a passive leg-raising test; however, there was a notable lack of agreement between TTE and ClearSight noninvasive monitoring regarding stroke volume measurements, raising concerns about the latter’s reliability.
– Patients identified as fluid-responsive experienced a higher incidence of significant intraprocedural hypotension compared to those classified as normovolemic (48% vs. 21%), demonstrating the potential risks associated with inadequate volume status during sedation.
– Demographic factors such as age, ASA status, and antihypertensive medication use did not correlate with fluid responsiveness, indicating the involvement of other unidentified elements in intravascular depletion.
– The study highlighted the necessity of ongoing monitoring during colonoscopies, particularly under propofol sedation, due to the anesthetic’s vasodilatory effects which can exacerbate hypotensive episodes, despite existing guidelines recommending preventive intravenous fluid administration.
– Findings point to an urgent need for enhanced understanding and management strategies for intravascular volume status prior to procedures, advocating for the exploration of advanced monitoring techniques in outpatient endoscopic environments to minimize the risk of adverse events.
Reference –
Allen, M.L., Kluger, M., Schneider, F. et al. Fluid responsiveness and hypotension in patients undergoing propofol-based sedation for colonoscopy following bowel preparation: a prospective cohort study. Can J Anesth/J Can Anesth 72, 529–539 (2025). https://doi.org/10.1007/s12630-025-02939-x
Powered by WPeMatico

Researchers at Tohoku University have discovered that an oral drug called MA-5 can improve both heart and muscle problems in Barth syndrome, a rare genetic disorder affecting 1 in 300,000 births worldwide with no current cure.
Barth syndrome is caused by mutations in the TAZ gene that leave patients-mostly young boys-with weakened hearts, muscle fatigue, and increased rates of infection. Many require heart transplants, and current treatments only manage symptoms without addressing the underlying cause.
The research team, led by Professors Takaaki Abe, and Takafumi Toyohara, and first author Yoshiyasu Tongu, tested MA-5 on cells from four Barth syndrome patients and in fruit fly (Drosophila) models of the disease. Published in The FASEB Journal on June 21, 2025, their findings reveal that MA-5 boosted cellular energy (ATP) production by up to 50% and protected cells from oxidative stress-induced death.
“What excites us most is that MA-5 works by targeting the fundamental problem in Barth syndrome-defective energy production in mitochondria,” explains Abe. “Unlike current treatments that only manage symptoms, MA-5 actually improves the root cause of how cells generate energy.”
MA-5 was chosen as a treatment because it enhances interactions between two crucial mitochondrial proteins-mitofilin and ATP synthase-leading to more efficient energy production. As such, this mechanism directly addresses the cause of cellular dysfunction in Barth syndrome.
In human muscle cells derived from Barth syndrome iPS cell models, MA-5 corrected abnormal mitochondrial structures and reduced cellular stress markers. When tested in Drosophila with Barth syndrome, the drug dramatically improved their climbing ability (capacity for physical exertion) and normalized their elevated heart rates-two key symptoms that mirror how the disease affects humans. Furthermore, MA-5 restored normal mitochondrial structure in the Drosophila muscle tissue.
These promising results suggest that MA-5 addresses the largest challenges faced by patients with Barth syndrome, which would significantly improve their quality of life. Phase I clinical trials in Japan have been completed successfully, and the research team is preparing to start Phase II trials soon.
“We’ve validated MA-5 using patient cells, iPS cell models and a Drosophila model of Barth syndrome,” remarks Abe. “The evidence from all of these studies supports its potential effectiveness in patients with Barth syndrome, which we hope to examine more in the next clinical trial.”
Considering the limited options for treatment currently available, this research provides hope for a better future for patients and their families. Critically, MA-5 can be taken orally, which makes administration significantly easier for pediatric patients. It is the first oral medication for Barth syndrome to progress to the clinical trial stage.
The team’s findings suggest that MA-5 could become the first disease-modifying treatment for Barth syndrome, offering new therapeutic options beyond current symptomatic management.
Reference:
Yoshiyasu Tongu, Tomoko Kasahara, Tetsuro Matsuhashi, Yoshitsugu Oikawa, Ryota Akimoto, Yuhan Luo, Sayaka Sekine, Momoka Suzuki, Hitomi Kashiwagi, Shinichiro Kanno, Mitochondria-Homing Drug Mitochonic Acid 5 Improves Barth Syndrome Myopathy in a Human-Induced Pluripotent Stem Cell Model and Barth Syndrome Drosophila Model, The FASEB Journal, https://doi.org/10.1096/fj.202401856RRR.
Powered by WPeMatico

UK: A 14-year observational study published in BMJ Open has revealed a strong link between blood sugar control and the risk of developing several eye diseases in older adults. The research, conducted by Caitlin Lin and Stephen Jivraj from the UCL Global Business School for Health, examined how diabetes status and blood sugar levels influence the likelihood of being diagnosed with glaucoma, diabetic eye disease, macular degeneration, and cataracts over time.
Using data from the English Longitudinal Study of Ageing (ELSA), the study followed over 5,600 participants aged 50 and above across eight waves of data collection from 2004 to 2019. Researchers analyzed nearly 29,000 observations, using logistic regression models to assess the relationship between baseline blood sugar status and the later development of eye conditions.
Participants were grouped based on their diabetic status and glycated hemoglobin (HbA1c) levels: non-diabetic (HbA1c <6.5%, no diabetes diagnosis), controlled diabetes (diagnosed with diabetes, HbA1c <6.5%), uncontrolled diabetes (diagnosed, HbA1c ≥6.5%), and undiagnosed diabetes (no diagnosis, HbA1c ≥6.5%). Adjustments were made for various factors, including age, gender, physical activity, BMI, and smoking.
The study led to the following findings:
According to the researchers, “Our findings suggest that maintaining good blood sugar control in older age not only helps in diabetes management but may also play a crucial role in preventing vision-related complications.”
The study is notable for its use of a large, nationally representative cohort with detailed biomarker and lifestyle data, offering valuable insights into the long-term effects of metabolic health on eye disease. However, the authors acknowledged limitations, such as reduced sample size over time due to participant attrition and the use of subjective physical activity data without duration metrics.
Overall, the study supports routine screening for eye diseases in older adults, particularly those with diabetes or elevated blood sugar levels. It also reinforces the need for early detection and proper glycemic control to help reduce the burden of preventable vision loss in aging populations.
Reference:
Lin C, Jivraj SAre diabetes and blood sugar control associated with the diagnosis of eye diseases? An English prospective observational study of glaucoma, diabetic eye disease, macular degeneration and cataract diagnosis trajectories in older ageBMJ Open 2025;15:e091816. doi: 10.1136/bmjopen-2024-091816
Powered by WPeMatico

Spending too much time on screens may cause emotional and behavioral problems in children-and those problems can lead to even more screen use, according to research published by the American Psychological Association.
Conducted by an international team of researchers, the study systematically reviewed and meta-analyzed 117 studies, encompassing data from over 292,000 children worldwide. The findings were published in the journal Psychological Bulletin.
“Children are spending more and more time on screens, for everything from entertainment to homework to messaging friends,” said Michael Noetel, PhD, an associate professor in the School of Psychology at Queensland University and one of the authors of the study. “We found that increased screen time can lead to emotional and behavioral problems, and kids with those problems often turn to screens to cope.”
Noetel and his colleagues conducted a meta-analysis to better understand the relationship between screen time and socio-emotional problems, like aggression, anxiety, or low self-confidence. They included any study with participants under 10 years of age that measured screen use and socio-emotional problems, where children were followed-up for at least six months. Screen-based activities included social media, video games, TV watching and online homework.
Most of the studies were conducted in the United States (41 studies), followed by Canada (13), Australia (11), and Germany and the Netherlands (7 each).
The study revealed that the more children engaged with electronic screens the more likely they were to develop socio-emotional problems. This included both internalizing problems, such as anxiety and depression, and externalizing problems, such as aggression and hyperactivity. Conversely, children experiencing socio-emotional problems were found to be more likely to turn to screens as a coping mechanism.
The researchers identified several factors that may moderate these relationships. Compared with younger children (ages 0-5), older children (ages 6-10) were more likely to develop socio-emotional problems with greater screen use. Girls were generally more susceptible to developing socio-emotional problems with greater screen use, while boys were more likely to increase screen use when facing socio-emotional challenges.
The type of screen content and purpose of screen use also played a role, according to Noetel. Gaming was associated with higher risks compared with educational or recreational screen use. Children experiencing socio-emotional problems were also more likely to turn to games to cope.
The findings suggest parents might want to be cautious about what screens they allow and use parental controls to manage time, said Noetel. He also noted that kids who use screens heavily might need emotional support, not just restrictions. Parents could benefit from programs helping them handle both screen use and emotional problems.
“This comprehensive study highlights the need for a nuanced approach to managing children’s screen time,” said lead author Roberta Vasconcellos, PhD, a lecturer at the University of New South Wales who conducted the research while a doctoral student at Australian Catholic University. “By understanding the bidirectional relationship between screen use and socio-emotional problems, parents, educators and policymakers can better support children’s healthy development in an increasingly digital world.”
Because every study in the meta-analysis followed kids over time, the research is a big step closer to cause‑and‑effect (as opposed to correlation) than the usual snapshots done at a single point in time, according to Noetel.
“It’s about as close as we can get to causal evidence without randomly cutting screens for thousands of kids,” he said. “But still, we can’t completely rule out other factors—like parenting style-that could influence both screen use and emotional problems.”
Reference:
Roberta Pires Vasconcellos, Taren Sanders, Chris Lonsdale, Philip Parker, James Conigrave, Samantha Tang, Borja del Pozo Cruz, Electronic Screen Use and Children’s Socioemotional Problems: A Systematic Review and Meta-Analysis of Longitudinal Studies, Psychological Bulletin, DOI: 10.1037/bul0000468
Powered by WPeMatico

China: A recent systematic review and meta-analysis published in Frontiers in Medicine highlights the potential role of the neutrophil-to-lymphocyte ratio (NLR) as a valuable biomarker for asthma diagnosis and severity stratification. Led by Lei Jin and colleagues from the Department of Cardiothoracic Surgery at The First Affiliated Hospital of Xi’an Medical University, the study aimed to clarify the diagnostic relevance of NLR amid previous uncertainties.
The researchers analyzed data from 19 studies, which included over 43,000 patients with asthma and more than 8,000 healthy controls. Using pooled statistical methods, they evaluated NLR values across different asthma severity groups and assessed how well NLR could distinguish asthma patients from healthy individuals through receiver operating characteristic (ROC) curve analysis.
The latest findings from this meta-analysis spotlighted the diagnostic utility of NLR. The results showed that NLR levels were significantly higher in individuals with asthma compared to healthy controls, with an area under the curve (AUC) of 0.92. Furthermore, NLR effectively differentiated between severe and non-severe asthma cases (AUC 0.91), making it a potentially useful tool for severity assessment. However, its ability to differentiate between moderate and severe asthma was limited, indicating the need for additional or complementary biomarkers to capture more nuanced stages of the disease.
The following were the key findings of the study:
Despite these promising insights, the study acknowledged key limitations. Considerable heterogeneity across the included studies may affect the consistency and broader applicability of the results. Additionally, since most studies were retrospective, they could be subject to selection and reporting biases. Moreover, while NLR shows strong potential, it may not sufficiently capture all aspects of disease progression on its own.
The authors concluded that the study supports the neutrophil-to-lymphocyte ratio (NLR) as an accessible and cost-effective biomarker for the identification and severity assessment of asthma. They highlighted the importance of conducting future prospective studies to validate these findings, establish standardized NLR cut-off values, and explore the potential of combining NLR with other clinical indicators to enhance the accuracy and precision of asthma management.
Reference:
Jin, L., Guo, J., Deng, K., & Yao, Y. (2025). Neutrophil-to-lymphocyte ratio as a biomarker for asthma identification and severity stratification: A systematic review and meta-analysis. Frontiers in Medicine, 12, 1620695. https://doi.org/10.3389/fmed.2025.1620695
Powered by WPeMatico

Distal radius fractures (DRFs) are common upper extremity injuries that often result in pain, limited mobility, and impaired proprioception. While conventional rehabilitation typically targets range of motion (ROM) and strength, closed kinetic chain (CKC) exercises may offer additional benefits by enhancing neuromuscular control and proprioception. Menek and Dansuk conducted a study to investigate the effects of CKC exercises on pain, function, proprioception, and ROM in individuals recovering from conservatively treated DRFs.
Forty individuals with conservatively treated DRF were randomly assigned to either the CKC group (n = 20) or the conventional group (CP) (n = 20). Both groups participated in a six-week rehabilitation program after cast removal. Outcome measures included Visual Analog Scale for activity-related pain (VAS-Activity), active ROM (flexion/ extension), Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire, and joint position sense (JPS).
Key findings of the study were:
• Both groups demonstrated significant improvements in all outcomes after six weeks (p < 0.05). However, the CKC group showed greater improvements across all domains.
• Specifically, JPS improved by 6.75° ± 3.21° in the CKC group compared to 4.95° ± 2.88° in the CP (Cohen d = 2.05), exceeding the minimal clinically important difference (MCID) of 5°.
• DASH scores decreased by 37.11 ± 10.27 points in the CKC group and 18.15 ± 9.61 in the CP (Cohen d = 3.46 vs. 1.77), both surpassing the 10-point MCID.
• Wrist extension increased by 44.00° ± 13.01 (CKC) versus 30.10° ± 11.42 (CP) (p < 0.001), and flexion by 52.50° ± 14.81 (CKC) vs. 39.20° ± 14.21 (CP) (p < 0.001).
• VAS-Activity scores improved by 5.35 ± 2.04 (CKC) and 3.40 ± 1.52 (CP) (Cohen d = 2.60 vs. 1.72), both exceeding the 2-point MCID threshold.
The authors concluded – “This study demonstrated that CKC exercises were more effective than conventional physiotherapy in improving JPS, upper extremity function (as measured by the DASH questionnaire), wrist ROM, and activity-related pain (assessed via the VAS) in individuals recovering from DRFs. These findings suggest that CKC exercises enhance proprioceptive input and neuromuscular control, thereby improving JPS and functional performance. Moreover, the increased joint loading and co-contraction during CKC exercises may contribute to reductions in pain and improvements in ROM, supporting their clinical utility. While the integration of CKC exercises into rehabilitation protocols appears to yield measurable improvements in proprioceptive function, pain management, and upper extremity functionality in individuals with DRF, further long-term follow-up studies are essential to validate the sustainability and external validity of these outcomes.”
Further reading:
Investigating the effects of closed kinetic chain exercises on joint position sense, functionality, range of motion, and pain in individuals with distal radius fracture: a randomized controlled trial Menek and Dansuk BMC Sports Science, Medicine and Rehabilitation (2025) 17:137 https://doi.org/10.1186/s13102-025-01195-2
Powered by WPeMatico
