Johnson & Johnson, through its subsidiary Ethicon, manufactures critical medical devices such as SURGICEL and ETHICON, widely used for wound closure and bleeding control in surgeries. However, in 2019, a neurosurgeon at the University of Kentucky Medical Center identified irregularities in a batch of SURGICEL products, which were later confirmed to be counterfeit.
Upon investigation, J&J traced the counterfeit medical products to M/s Medserve, a business operated by Pritamdas Arora in New Delhi. The counterfeit products were substandard, non-sterile, and contaminated, posing a severe risk to patient safety.
The Delhi High Court, presided over by Justice Amit Bansal, reviewed extensive evidence, including WhatsApp conversations, email correspondences, invoices, and financial transactions, confirming the defendants’ direct involvement in counterfeiting activities.
Justice Bansal emphasized the severity of the counterfeiting, stating;
“Counterfeiting of medical devices is not merely a case of trade mark infringement, it is a grave offence that endangers the lives of people. The defendants’ conduct demonstrates a deliberate effort to mislead the public, jeopardize consumer safety and exploit consumer trust for financial gain.”
The court highlighted that counterfeit medical products lacked essential sterility and quality standards required for surgical use. Further, the defendants falsified expiration dates on expired medical products, increasing the health risks for unsuspecting patients.
“The counterfeit products failed to meet the necessary oxidation levels required for proper absorption in the body. The use of such substandard medical devices during surgery could result in severe complications, including infections, foreign body reactions, and surgical adhesions.”
The court also criticized the impact of counterfeiting on J&J’s reputation, stating;
“The defendants’ deliberate and fraudulent acts have also caused irreparable harm to the plaintiff’s goodwill and market reputation. By selling substandard counterfeit products under the plaintiff’s trade marks, the defendants have misled consumers and associated the plaintiff’s name with the counterfeit goods.”
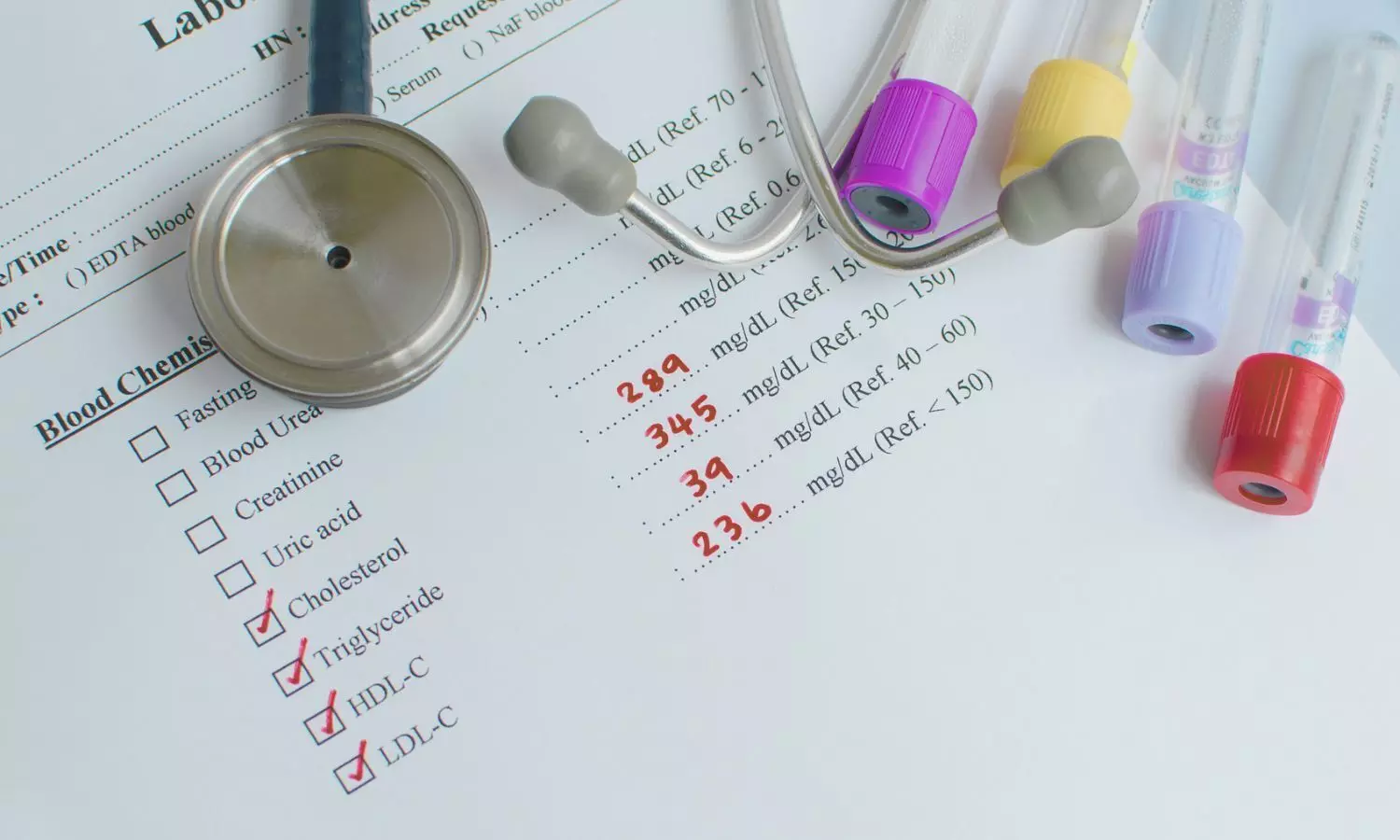
Taking a strict stance against counterfeiting, the court awarded Rs 2.34 crore as compensatory damages based on sales figures of counterfeit products and an additional Rs 1 crore as exemplary damages, citing the defendants’ deliberate and fraudulent actions.
Justice Bansal justified the award, noting;
“I am convinced with the evidence presented and submissions made by the counsel for plaintiff and conclude that a conservative profit margin of 25% can be assumed for awarding actual damages in favor of the plaintiff and against the defendants in the present case.”
“Counterfeit medical products are a direct threat to public health and safety. The defendants’ conduct demonstrates a deliberate effort to mislead consumers and exploit their trust for financial gain.”
The court-appointed Local Commissioner conducted raids on the defendants’ premises, seizing counterfeit ‘SURGICEL’ and ‘ETHICON’ products, along with falsified documentation, counterfeit labels, and substantial financial records.
The investigation revealed that the defendants laundered over Rs 9.39 crore through international transactions, diverting funds to multiple foreign bank accounts.
The court took serious note of the defendants’ refusal to cooperate, observing;
“The evidence presented before the Court, including invoices, bank receipts, and chat extracts, establishes without a doubt that defendant no. 1 has received substantial financial gains in the course of carrying out the infringing and counterfeiting activities.”
Despite multiple summons, the defendants failed to appear before the court, prompting the issuance of non-bailable warrants against Pritamdas Arora, who remained untraceable.
To prevent further consumer deception and safeguard public health, the court granted a permanent injunction restraining the defendants from using J&J’s trademarks, selling counterfeit products, or engaging in any activities that could mislead consumers into believing they were purchasing genuine J&J products.
The court also ordered the destruction of all counterfeit products seized during the proceedings, stating;
“The plaintiff is entitled to compensatory and exemplary damages, and the counterfeit products seized shall be destroyed to prevent further harm to the public.”
To view the original order, click on the link below: