Patient’s death case at GMCH Chandigarh: No medical negligence, says hospital panel

Chandigarh: Investigating the allegations of medical negligence in the case of a 63-year-old woman who had suffered a cardiac arrest due to a pending MRI test and its related treatments, which was believed to have potentially saved her life, the committee has found no substantial evidence against the doctor or the Government Medical College and Hospital (GMCH), Sector 32.
According to the preliminary report submitted by the panel, the doctor was not deemed negligent since there was insufficient evidence implicating him or the hospital in any misconduct that could have resulted in medical negligence and the patient’s demise.
This comes in response to the allegations made by the deceased’s family members, accusing the doctor of providing inadequate healthcare services and delaying treatment to the patient. They alleged that rather than sending the COVID samples to a private institution, GMCH should have taken charge of conducting the tests and administering the appropriate treatment to the patient.
Denying the claims, Hospital director-principal Dr Jasbinder Kaur informed HT, “The medical negligence committee has concluded that there is no substantial evidence which proves that the treating doctor has any monetary consideration for getting laboratory test from a private lab. Further, as per statements given by the doctors and careful examination of the complaint, along with documentary evidence placed on record, the committee thinks that the patient was managed properly as per protocol,”
According to The Daily, the case involved a 63-year-old woman from Baltana, Mohali, who was admitted to the hospital on May 8, 2021, during the peak time of the COVID-19 pandemic. She was experiencing pain in the upper limbs.
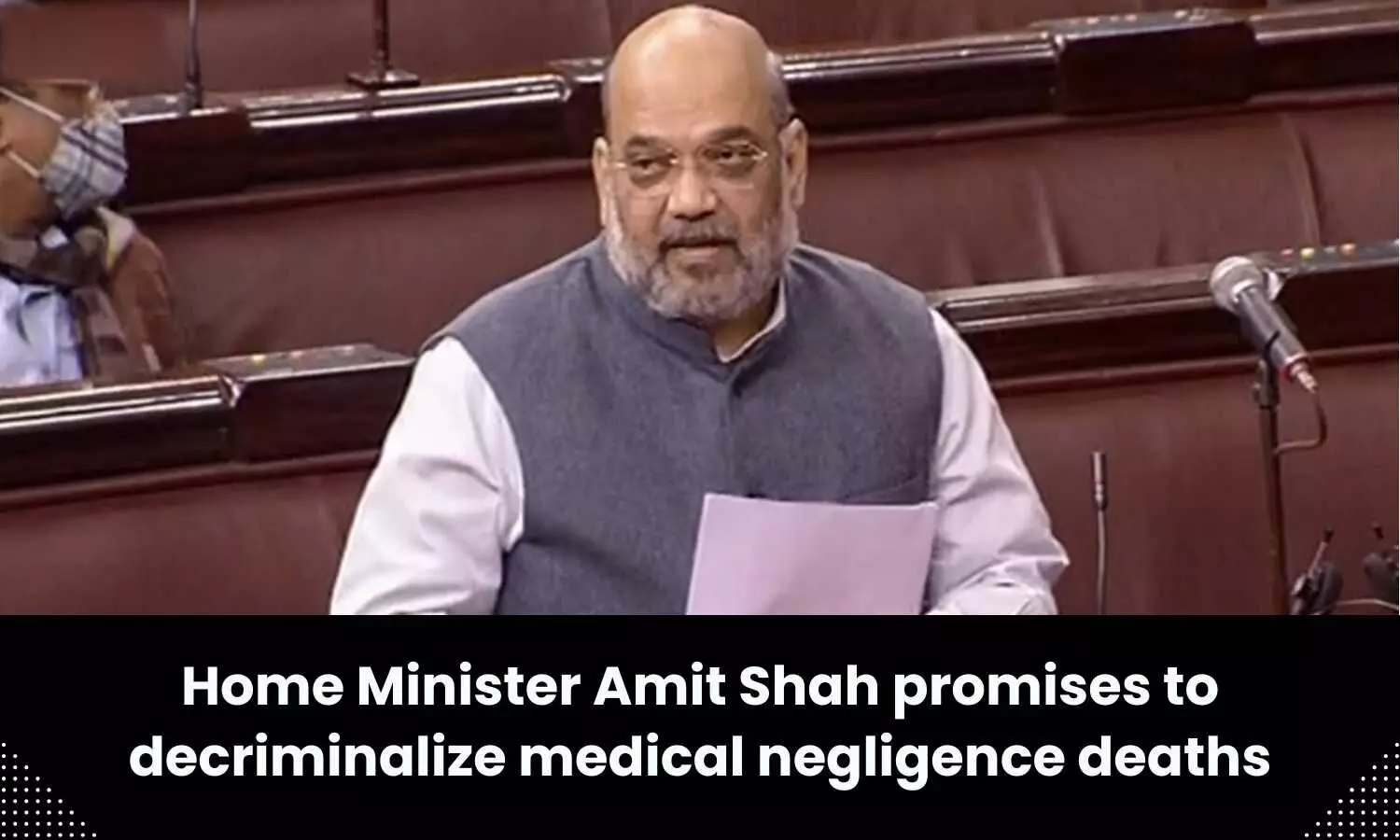
The medical examination revealed that she was diabetic and had no blood flow in the arteries, causing extreme pain in the right upper limb. The doctors planned an embolectomy (removal of a blood clot) to relieve the thrombus and resume blood flow.
Due to the strict protocol during the peak of the COVID-19 pandemic, all surgery/ICU/MRI patients were required to undergo RTPCR testing. However, due to the high volume of tests, it took more than 24 hours to test patients within GMCH. The RTCPR test was done through a private laboratory after discussing with the patient’s attendants to prioritise patient care.
The medical negligence committee in the report stated that the test samples were sent to a GMCH lab and a private hospital. The private hospital’s report was negative for Covid. Although the report was available before the MRI, the test could not be done as the patient was developing breathlessness.
On May 11, the patient was moved to a ventilator after severe chest pain and falling unconscious. Despite efforts, including CPR, the patient suffered a cardiac arrest and was subsequently moved to the ICU. Another cardiac arrest occurred on May 13, and despite all measures, the patient could not be revived.
The GMCH officials decided to engage the police in the matter, consequently submitting the report to the Chandigarh SSP for necessary measures to be taken.
Powered by WPeMatico