Tripura: The Director of Medical Education (DME Tripura) has invited applications for Online Stray Vacancy Round of Tripura State NEET UG 2024 counselling for Tripura state quota/Domicile seats and All India other than Tripura candidates.
All the eligible candidates who have not registered in earlier Rounds of Tripura State NEET UG 2024 Counselling can register themselves in Stray Vacancy Round of Tripura State NEET UG 2024 Counselling.
All the registered candidates (Round-I, Round-2, Round-3 & freshly registered candidates of Stray Vacancy Round) who intend to apply for Stray Vacancy Round of Tripura State NEET UG 2024 Counselling MUST APPLY ONLINE by submitting the online application form of Stray Vacancy Round through the counselling website.
If any candidate (registered in Round-1/Round-2/Round-3/ Stray Vacancy Round) fails to submit the online application form for Stray Vacancy Round of Tripura State NEET UG 2024 Counselling, then his/her candidature for the Stray Vacancy Round counselling will not be considered.
Schedule for Stray Vacancy Round of Tripura State NEET UG 2024 Online Counselling
|
Event
|
Date & Time
|
- Online Registration
- Online Payment of registration fee.
- Offline
payment of security deposit and submission of security deposit details ONLINE and
physical submission to the
DME office.
|
28-10-2024 (12 Noon) to 30-10-2024
(up to 12 Noon)
|
|
Publication of Merit list
|
31-10-2024
|
|
Choice Filling by the candidates
|
31-10-2024 (4 PM onwards) to
02-11-2024 (up to 10 AM
|
|
Allotment Result
|
02-11-2024
|
|
Submission
of Allotment letter to the office of DME
|
03-11-2024
|
|
Nomination to be collected from DME office by a
candidate allotted a seat
|
03-11-2024 (3 PM onwards) 05-11-2024 (12 noon)
|
|
Physical
verification of original documents
and other admission formalities and admission in the allotted admitting Institutions
|
03-11-2024 (3 PM onwards) 05-11-2024 (5 PM)
|
|
Counselling Link
|
|
Counselling Related Information
|
Candidates are instructed not to wait for the last hours regarding any event of the schedule of Registration/choice filling/submission of relevant documents at DME/admission.
; seat matrix is furnished as per information of vacant seats received from respective Institute up to 25-10-2024. A) Seat Matrix for MBBS
Seat Matrix for MBBS
Name of
Medical College |
Total |
UR |
EWS |
ST |
OBC |
SC |
| Agartala Government Medical College, Agartala, Tripura |
2 |
— |
2 |
|
— |
_ |
| Tripura Medical College & Dr. BRAM Teaching Hospital, |
1 |
…….. |
— |
1 |
—- |
— |
Tripura Santiniketan Medical College,Agartala,
Tripura,Madhuban, Ranir Khamar, Amtali, |
36 seats at Prescribed tuition fee rate of Tripura Santiniketan
Medical College |
8 |
—– |
18 |
|
09+01(WESM |
| All India other than Tripura State Domicile candidates |
All India other than Tripura StateTripura State Domicile
candidates in Tripura Medical College & Dr. BRAM Teaching Hospital, |
1 |
— |
— |
— |
…… |
1 |
All India other than Tripura State Domicile
candidates in Tripura Santiniketan Medical College, Agartala, Tripura,
Madhuban, RanirKhamar, Amtali,Agartala, Tripura |
67 |
32 |
—– |
5 |
20 |
10 |
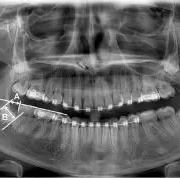
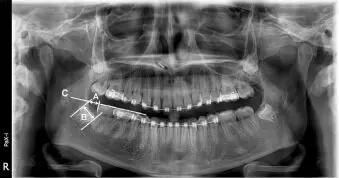
Seat Matrix for BDS
|
Name of
Dental College
|
Total
|
UR
|
ST
|
SC
|
|
Agartala Government Dental
College, Agartala, Tripura
|
02
|
02
|
—
|
—
|
|
Regional Institute of Medical
Sciences, Imphal, Manipur
|
01
|
—
|
01-
|
—
|
Seat Matrix for BHMS
Name of
the College |
Total |
UR |
ST |
SC |
| Midnapore Homoeo Medical College, Midnaporc, West Bengal |
1 |
— |
1 |
— |
Seat Matrix for BASLP
Name of
the College |
Total |
UR |
ST |
SC |
| Regional Institute of Medical Sciences, Imphal, Manipur |
1 |
|
0
1 |
|
A) NON-REFUNDABLE REGISTRATION FEES FOR ONLINE NEET UG 2024 COUNSELLING
The Registration fees for fresh candidates (not registered in earlier Rounds), who wants to register in the NEET UG 2024 counselling, will be as follows according to their category.
Online Submission of Application Form with Registration Fee by
the Candidate |
Registration
Fees for Counselling |
| Category |
General/OBC-NCL-(State
Domicile) |
Rs.
2500/- |
General-EWS (State Domicile)/OBC-NCL-(Non
Domicile) |
Rs.
2000/- |
| SC/ST/PwD/Other |
Rs.
1800/- |
*Registration fees for the candidates under OBC-NCL (Non creamy Layer) category registering for State quota/Domicile seats will be as per registration fees for General candidate.
*Registration fees for the candidates under OBC-NCL (Non creamy Layer) category registering for All India other than Tripura seats will be as per registration fees for General-EWS candidate.
B) MANDATORY SECURITY DEPOSIT
The Mandatory Security deposit has to be paid by the candidates-
i) Freshly registered candidates of Stray Vacancy Round (who have not registered in earlier Rounds).
ii) The candidates who have not paid their mandatory security deposit in Round-1 3.
iii) The candidates who have already paid rnandatory security deposit for Government College seats only (Rs.10.000 or Rs. 5.000) and now want to apply for Tripura Medical College (TMC) or Tripura Santiniketan Medical college(TSMC) Seats by paying Rs.1 lakh as Security deposit
| Details of Mandatory Security Deposit |
| For Government College Seats |
For
SC/ST category candidate Rs. 5000/- (Rupees five thousand) only. For other category candidate Rs.
10,000/- (Rupees ten thousand) only. |
For 1) Non-Government College Seats 2) Both Non-Government &
Government College Seats. 3) Non- Government College seats (Tuition fee rate
of Government Medical college at Tripura Santiniketan Medical College) |
For
all category candidates Rs. 100000/-(Rupees One Lakh) Only. |
The mandatory security deposit shall have to be submitted through Bank Demand Draft/Bank Deposit/Online transaction. The demand draft shall have to be payable in favour of “Directorate of Medical Education, Government of Tripura- from any nationalized bank Preferably SBI.
Account
details of DME |
| ACCOUNT NO OF DME |
34706666148 |
| BANK NAME |
STATE
BANK OF INDIA |
| IFSC code |
SBLN0000002 |
| ADDRESS OF THE BANK |
H.G
BASAK ROAD, AGARTALA |
All the candidates who are submitting the security deposit for first time during the Stray Vacancy Round or chan2edimodified the already submitted amount of security deposit of earlier rounds (Round-2/Round-3). are requested to mandatorily submit the original demand draft/counterfoil of original bank deposit/scanned copy of online transaction receipt mentioning the transaction number/ID to the office of the Director of Medical Education, Bidurkarta Chowmohani, Agartata PHYSICALLY on or before 30-10-2024 (up to 12 Noon). The format for submission of security deposit details is given in ANNEXURE-1.
Eligibility and qualification: The eligibility and qualification to get a seat shall be in accordance with information bulletin of Tripura State NEET UG 2024 Counselling published by DME and information bulletin published by NTA/Guidelines of MCC/NMC/MCl/MoHFW/Ministry of AYUSH/ guidelines of Institutions.
Following categories of Candidates are not eligible for Stray Vacancy Round:-
a) Candidates who have not registered for Stray Vacancy Round.
b) Candidate joined/holding any seat from either State or MCC Counselling at the time of Stray Vacancy Round.
c) Candidates allotted a seat in Round 3 of Tripura State NEET UG 2024 Counselling.
The candidates are reminded that-
The scanned copy of original demand draft/counterfoil of original bank deposit/online transaction ,receipt mentioning the transaction number/ID in respect of mandatory security deposit shall have to be provided wherever applicable during uploading of the security deposit details.
2) The fresh candidates are also reminded to go through the information bulletin and earlier notifications issued by the Director of Medical education, Govt. of Tripura in respect to the earlier Rounds of Tripura NEET UG 2024 Counselling to keep abreast of the counselling.
3) All the aspirant eligible candidates are instructed to follow the DME website regularly for further Notices/Updates/Notification which may be issued from time to time.
- Candidates are instructed to participate in the “Choice filling” as per their choices in the Counselling for allotment of seats as per seat matrix and category according to Merit (Result score and Rank of NEET UG 2024). Candidates are instructed to follow the website of Allotted Institutions for details regarding admission and other details.
- Freshly Registered Candidates shall have to submit Registration fees and mandatory Security deposit as notified earlier which is mandatory for all to participate in Stray Vacancy Round. Documents of Eligibility, NEET UG 2024 score Card, Admit Card, Age Proof Certificate and all others relevant certificates shall have to be uploaded during Online Registration.
The details of appropriate supporting document to be uploaded by the freshly registered candidates of Stray Vacancy Round are as follows:
| Serial No. |
Certificates |
Documents to be
uploaded |
1.
|
Age
Proof |
Birth
Certificate/Class X Admit Card/Class X pass certificate |
2.
|
Clause
Supporting Documents |
1) Clause-1: PRTC of
the candidate/PRTC of the parents.
2) Clause 2: Parents service certificate clearly
mentioning about service in the state of Tripura. 3) Clause 3: Parents
service/deputation certificate issued by the appointing authority.
4) Clause 4: Valid Certificate of WESM issued from Rajya
Sainik Board 5) Clause 5: Service Certificate of the
parents along with candidate’s class 12th admit card /marksheet However, if
any other clause supporting documents is submitted confirming the eligibility
of the candidate is subject to be verified by the Tripura NEET UG 2024
counselling committeee |
| 3 |
Economically
Weaker Section (EWS) |
EWS
certificate issued form the appropriate authority for the Financial year
2023-2024. |
| 4 |
Ward
of Ex-serviceman (WESM) |
Valid
WESM certificate for NEET UG 2024 issued from the Rajya Sainik Baord |
| 5 |
SC/ST/OBC-NCL |
SC/ST/OBC-NCL
Certificate issued by the competent authority. |
| 6 |
Disability
Certificate |
Issued
from a duly constituted and authorized Medical Board in an ONLINE format by
the designated centeres as per NMC norms (Gazette Notification no.
MCI-34(41)/2018Med./170045 dated 04/02/2019) No other PWD certificate, issued
by any other Authority/Hospital will be entertained. |
| 7 |
H.S(+2)
Marksheet |
H.S
(+2) Marksheet (In case of Grades are awarded instead of secured marks
/percentage, then the details of Grade to the corresponding marks/percentage
must be produced by any supporting official document) |
| 8 |
NEET
Score card 2024 |
Latest
NEET Score card 2024 |
| 9 |
NEET
2024 Admit Card |
NEET
2024 Admit Card |
All the candidates who are going to participate in the Stray Vacancy Round are instructed to go through all the earlier notifications/information bulletin/guidelines/steps of counselling/flow chart in connection with Tripura State NEET UG 2024 Counselling throughly.
To view the official Notice, Click here : https://medicaldialogues.in/pdf_upload/educational-notification-regarding-online-stray-vacancy-round-of-tripura-state-neet-ug-2024-counselling-258553.pdf