Colloidal Nano Silver Gel effective and safe in treating bacterial vaginosis and vulvovaginal candidiasis: IJOGR

Vaginal infections, often termed “Infectious
Vaginitis,” are common concerns for women across the lifespan, with a
higher prevalence among women of reproductive age. It is the most frequent
reason for women to seek medical attention. Although these infections are not
associated with significant mortality, they are often associated with high
levels of anxiety and have a negative impact on sexual life, self-esteem, and
quality of life. The more prevalent vaginal infections are caused by
disturbances in the natural vaginal microbiome. The normal vagina flora is
characterized by the dominance of lactic acid producing bacteria, especially
Lactobacillus spp., which help to maintain an acidic pH of vaginal fluids
within the range of 3.5-4.5. Along with lactobacilli, a healthy, acidic
premenopausal vagina also contains a heterogeneous mixture of Gardnerella
vaginalis, Escherichia coli, group B streptococcus (GBS), genital Mycoplasma
species, Candida albicans, and other species.
The most commonly documented cause of vaginitis is bacterial
vaginosis (BV). BV is characterized by a dramatic switch of vaginal bacterial
flora from normal predominant Lactobacilli to a polymicrobial flora. Vulvovaginal
candidiasis (VVC) is the second most common vaginal infection, while trichomoniasis,
caused by Trichomonas vaginalis, is the most common non-viral sexually
transmitted infection. True mixed infection rarely occurs in women with
vaginitis, but coinfection occurs much more frequently. Coinfection with
Candida species is observed in about 20%-30% of women with BV. The coinfection
rates of BV pathogens and trichomoniasis are even more prevalent. Other
etiologies of vaginitis include vulvar skin diseases, desquamative inflammatory
vaginitis, and genitourinary syndrome of menopause.
Despite the availability of numerous oral, topical, and
intravaginal medications for the treatment of vaginal infections, their
management remains challenging. Associated side effects, development of
resistance, lack of prevention and destruction of biofilms, and higher
recurrences are the limitations of currently available conventional therapies.
Ineffectiveness due to poor penetration and rapid removal from the vaginal
canal are the major hurdles in achieving infection cure with local
antimicrobial therapies. There is a need to develop newer therapeutic options
for treating vaginal infections that overcomes the limitations of current
therapies.
During the last decades, nanotechnologies-based
formulations, such as nanoparticles, have been explored to overcome the
limitations of current therapies for vaginal infections. These novel
formulations can improve local drug delivery, biodistribution, retention, and
uptake in vulvovaginal tissues. Other important benefits nanotechnology-based
formulations offer are reduced toxicity, enhanced patient compliance, and
improved treatment outcomes.
The study by Dani, Godbole and Mehta evaluated the efficacy
and safety of colloidal nano silver gel (SilverSol® Vagigel) (A patented
technology from American Biotech Labs, USA) in combination with 0.2% lactic
acid in the female subjects for the treatment of vaginal infections.
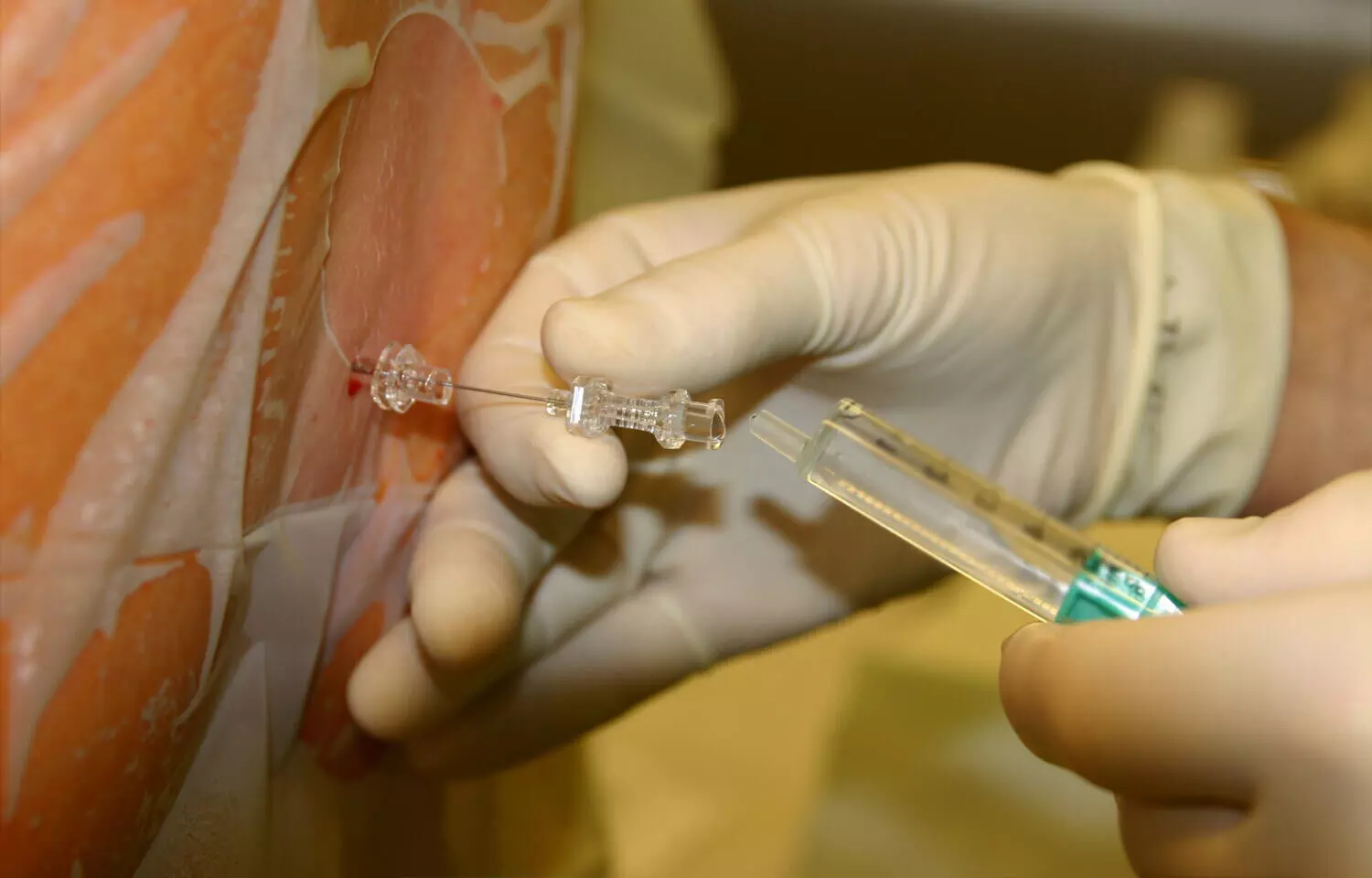
This study was a multicenter, randomized, double-blind,
placebo-controlled pilot study in which post-menarchal female subjects between
18 and 65 years of age clinically diagnosed with bacterial vaginosis and
vulvovaginal candidiasis were enrolled. The participants were randomized to
receive treatment with SilverSol® Vagigel or placebo (vehicle) gel (both
treatments as one 4 gm application inserted into the vagina with an applicator
device, once daily at bedtime for internal use and 2 gm gel for local
application to the vulva and vagina for external use twice daily for a period
of 14 days). The primary endpoint evaluated was the proportion of subjects
achieving clinical cure. The secondary endpoint was the proportion of subjects
achieving microbiological cure at the end of the study visit.
A total of 57 subjects were randomized in the study out of
which 38 subjects were randomized in SilverSol® Vagigel arm and 19 subjects
were randomized in placebo arm. SilverSol® Vagigel significantly improved cure
rates of vaginal infections compared to placebo.
The proportion of subjects achieving clinical cure of
vaginal infections was higher i.e., 33 (86.84%) subjects in SilverSol® Vagigel
arm compared to 07 (41.18%) subjects in Placebo gel arm (p-value: 0.0009).
The clinical cure rate with SilverSol® Vagigel was 81.82%
(P=0.1758) for bacterial vaginosis and 92.59% (P=0.0010) for vulvovaginal
candidiasis patients at the end of the study.
Overall SilverSol® Vagigel treatment resulted in a
significantly higher microbial cure of vaginal infections (P=0.0028) compared
to placebo, with a microbial cure rate of 100% for bacterial vaginosis
(P=0.0330) and 85.19% for vulvovaginal candidiasis (P=0.0097).
No adverse events were reported in subjects treated with
SilverSol® Vagigel.
In this study, SilverSol® Vagigel was effective and safe in
treating the most common vaginal infections i.e. bacterial vaginosis and
vulvovaginal candidiasis. Overall, the findings of this study, combined with
the existing body of evidence, indicate that SilverSol® Vagigel may represent a
valuable addition to the armamentarium of available therapies for vaginal
infections, offering potential benefits for patients in terms of improved
outcomes and reduced side effects. Overall, SilverSol Vagigel represents an
excellent advancement in women’s health, offering a highly effective and safe
solution for treating vaginal infections. Leveraging the exceptional antibacterial,
antiviral, antifungal, andimmune-enhancing properties of SilverSol®, SilverSol®
Vagigel formulation can emerge as a promising therapeutic option for treating a
wide range of vaginal infections and delivering unparalleled safety and
efficacy in addressing diverse feminine health concerns.
Source: Dani, Godbole and Mehta / Indian Journal of
Obstetrics and Gynecology Research 2024;11(1):83–89;
https://doi.org/10.18231/j.ijogr.2024.015
Powered by WPeMatico