Calcium and oxytocin combo Better for inducing labor in term women with premature rupture of membranes: Study
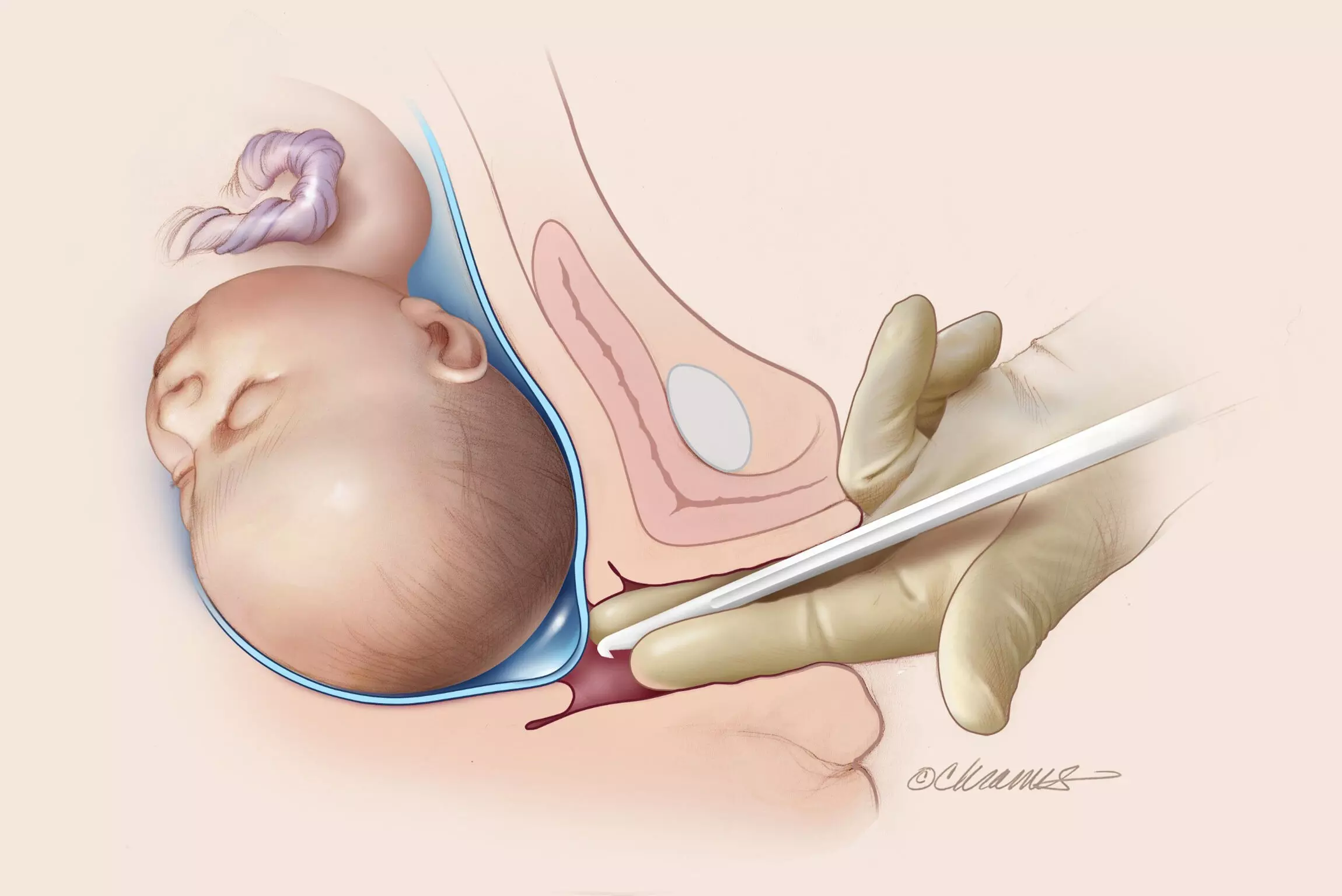
A study published in the American Journal of Obstetrics & Gynecology MFM suggests that a calcium and oxytocin combo is better for inducing labor in term women with premature membrane rupture.
Intravenous calcium administration has shown promise in enhancing uterine contractions and reducing blood loss during cesarean delivery, but this regimen has not been compared in vaginal labor induction. This study aimed to determine the efficacy of oxytocin combined with calcium vs oxytocin alone for inducing labor in women with term premature rupture of membranes. This single-blind, randomized controlled trial was conducted between October 2022 and May 2023 at a tertiary university hospital. Patients diagnosed with premature rupture of membranes were randomly allocated into 2 groups. The intervention group received a bolus of 10 mL of calcium gluconate followed by a continuous infusion of oxytocin via a pump (n=210), whereas the control group received only oxytocin infusion (n=218). The primary outcome was successful vaginal deliveries within 24 hours after labor induction. The secondary outcomes included the interval from labor induction to delivery, vaginal delivery blood loss, and maternal and neonatal complications. RESULTS: Baseline characteristics, including maternal age, body mass index, and Bishop score before labor induction, were comparable between the groups. The rate of vaginal delivery within 24 hours after labor induction was statistically higher in the intervention group (79.52% vs 70.64%; P=.04). The participants in the intervention group experienced a shortened interval between labor induction and delivery (10.48 vs 11.25 hours; P=.037) and demonstrated a higher success rate in labor induction assessed by the onset of the active phase (93.80% vs 87.61%; P=.04) without increasing the cesarean delivery rate. Reduced hemorrhage was observed in the intervention group (242.5 vs 255.0 mL; P=.0015), and the maternal and neonatal outcomes were comparable between the groups. The coadministration of calcium and oxytocin in labor induction among pregnancies with premature rupture of membranes was more efficient and safer than the administration of oxytocin alone. Our research suggests that the combination therapy of calcium and oxytocin may offer significant advantages during the process of labor induction and result in better outcomes.
Reference:
Ruixiang Cai, Lingyan Chen, Yunguang Xing, Yuguo Deng, Juan Li, Fangfang Guo, Li Liu, Cuihua Xie, Jinying Yang. Oxytocin with calcium vs oxytocin for induction of labor in women with term premature rupture of membranes: a randomized controlled trial. American Journal of Obstetrics & Gynecology MFM, Volume 6, Issue 11, 2024, 101502, ISSN 2589-9333,
https://doi.org/10.1016/j.ajogmf.2024.101502.
(https://www.sciencedirect.com/science/article/pii/S2589933324002283)
Keywords:
Calcium, oxytocin, combo, Better, inducing, labor, term, women, premature, rupture, membranes, study, American Journal of Obstetrics & Gynecology MFM, Ruixiang Cai, Lingyan Chen, Yunguang Xing, Yuguo Deng, Juan Li, Fangfang Guo, Li Liu, Cuihua Xie, Jinying Yang
Powered by WPeMatico