Millions of women rely on contraceptives, but a new study shows they may do more than just prevent pregnancy
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
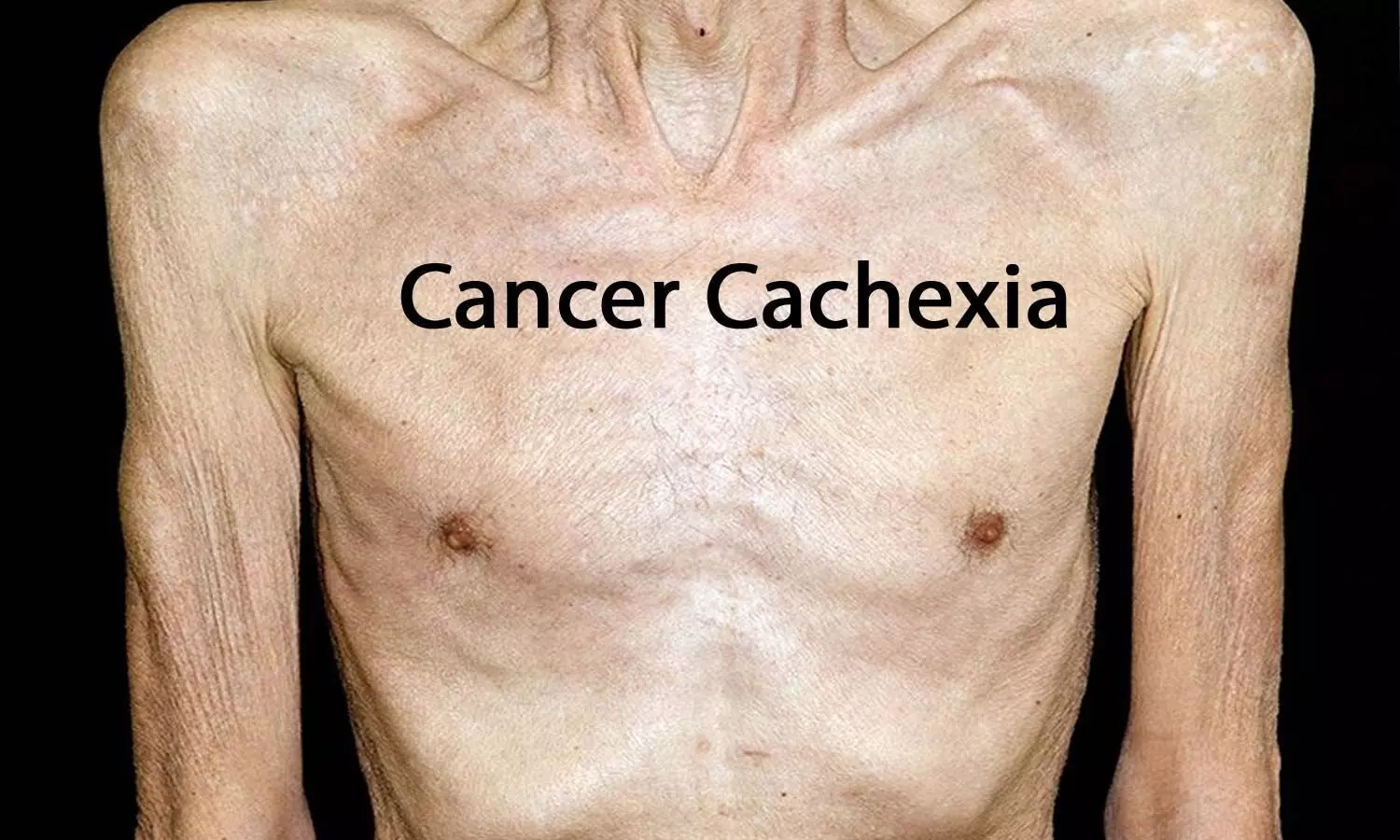
Researchers have found in a new study that cachexia index (CXI) may be a valuable indicator for assessing cancer cachexia and health-related quality of life in gastric cancer patients. The study was published in BMC Cancer journal by Yan H. and colleagues.
Cachexia, a multifaceted metabolic syndrome involving intense muscle wasting and weight loss, is well recognized to be connected with unfavorable clinical outcomes in GC patients. In the present study, CXI was calculated according to the following formula: skeletal muscle index (SMI) × serum albumin / neutrophil–lymphocyte ratio (NLR). The present study was conducted to determine if CXI could efficiently detect cachexia and foretell HRQoL impairments.
The analysis involved 431 patients with GC, made up of 309 men (71.7%) and 122 women (28.3%), with an age at median of 68 years. Diagnosis of cachexia was made according to both AWGC criteria and Fearon’s criteria. Univariate logistic regression and multivariate logistic regression analyses were employed to determine independent risk factors for cachexia and for poor HRQoL. ROC curve analysis was conducted to establish diagnostic performance of CXI in diagnosing cachexia, as well as calculate the area under the curve (AUC).
Results
• CXI scores were much lower in cachexia patients than in non-cachexia patients, according to both AWGC and Fearon’s definitions (p < 0.001).
• CXI was independently related to AWGC-defined cachexia after controlling for confounding variables (OR = 0.98, 95% CI: 0.97–0.99, p < 0.001) but was not related to Fearon-defined cachexia (OR = 1.00, 95% CI: 0.99–1.01, p = 0.601).
• ROC analysis identified an AUC of 0.752 for men and 0.717 for women in detection of AWGC-defined cachexia, with best cut-off scores of 74.46 and 43.80 respectively.
• Patients with low scores on CXI had more severe impairment on several HRQoL domains, and low CXI was independently linked with compromised HRQoL (OR = 1.79, 95% CI: 1.05–3.07, p = 0.033).
The research concluded that cachexia index is a useful and trustworthy biomarker for the diagnosis of cachexia according to AWGC criteria and for the prediction of poor HRQoL in gastric cancer patients. The integration of CXI into clinical practice would potentially improve patient surveillance and inform early interventions directed at enhancing survival as well as quality of life.
Reference:
Huang, Y., Huang, Z., Hou, W. et al. Cachexia index as a biomarker for cancer cachexia and quality of life in patients with gastric cancer. BMC Cancer 25, 1293 (2025). https://doi.org/10.1186/s12885-025-14752-2
Powered by WPeMatico

New Delhi: The Subject Expert Committee (SEC) functional under the Central Drugs Standard Control Organisation (CDSCO) has deferred further action on Biosphere Clinical Research Pvt. Ltd.’s Colloidal Nano Silver Gel (SilverSole), after observing that the pharmacokinetic study details were not fully reflected in the presentation.
Additionally, the Committee directed Biosphere to submit the complete clinical trial protocol, detailed report, and toxicity data for review before any further decision could be taken.
The company had appeared before the committee to present findings from a Phase I clinical trial (Protocol No. BCR-VIR-003, dated May 12, 2025) that sought to evaluate the safety and pharmacokinetics of Colloidal Nano Silver Gel in healthy adult female subjects. The application was linked to an earlier recommendation dated July 25, 2024.
However, after deliberation, the SEC observed that the pharmacokinetic study details were not adequately reflected in the PowerPoint presentation submitted by the firm. The panel observed:
“Complete details with respect to the pharmacokinetics study are not reflected in PowerPoint presentation presented by firm.”
The committee also emphasized that Colloidal Nano Silver vaginal gel is not yet approved in India or in any other country. In view of this, it decided that a comprehensive review of the full study protocol, detailed report, and toxicity data would be required before taking any further decision on the clinical trial.
“Colloidal Nano Silver vaginal gel is not yet approved in India and other countries and opined that committee needs to review complete protocol, report and toxicity data for further necessary action,” the Expert Committee said.
Colloidal silver products have historically been promoted for their antimicrobial properties. However, global regulatory authorities, including the U.S. Food and Drug Administration (FDA), have repeatedly raised safety concerns due to lack of robust clinical evidence. The FDA had issued warning letters to companies marketing colloidal silver products with unapproved health claims, underscoring that such products require rigorous clinical validation before being considered safe for medical use
Powered by WPeMatico

For women with inflammatory bowel disease (IBD), pregnancy can be an uncertain time due to limited clinical data about how IBD medications impact pregnancy outcomes and infants who have been exposed to IBD medications in utero.
As a matter of policy, pregnant women are excluded from clinical trials of experimental therapies for IBD and when a new therapy achieves regulatory approval, there is only animal safety data, but no human pregnancy safety data.
For patients with IBD, stopping medication leads to an increase in IBD symptoms, which can make their pregnancies high-risk. These women are often young and otherwise healthy, so they are not always recognized as high-risk despite the association of uncontrolled IBD with adverse maternal and obstetric outcomes.
To improve treatment of IBD during pregnancy worldwide, the Helmsley PIANO Expert Global Consensus was convened to provide standardized, evidence-based recommendations to providers caring for women with IBD. The PIANO (Pregnancy Inflammatory Bowel Disease And Neonatal Outcomes) study looked at the safety of IBD medications in pregnancy and short- and long-term outcomes of the children.
Based on reviews of the literature by the consortium experts, final recommendations for the global consensus were published simultaneously on August 28, in six international journals including Clinical Gastroenterology and Hepatology,American Journal of Gastroenterology, GUT, Inflammatory Bowel Diseases, Journal of Crohn’s and Colitis, and Alimentary Pharmacology and Therapeutics.
The final study results and guidelines include new findings such as continuing all biologics throughout pregnancy and lactation, universal pre-conception counseling, understanding of high-risk maternal status, providing low dose aspirin to prevent preterm preeclampsia, and giving the rotavirus vaccine on schedule.
“Some of the findings were expected, but others were novel,” said Uma Mahadevan, MD, director of the Colitis and Crohn’s Disease Center at UCSF, principal investigator of the PIANO study, and chair of the Global Consensus Conference. “The goal of our study and consortium has been to provide hope, comfort, and the same high-level care to current and future mothers with IBD. The consensus recommendations are the first truly global effort to improve treatment and outcomes for women with IBD and their children.”
Specifically, the consortium recommends women with inflammatory bowel disease receive preconception counseling and ideally be in remission for three to six months prior to considering conception. It also recommends that all women with IBD are followed as high-risk pregnancies.
Also recommended is the continuation of medications that are considered low risk for use during pregnancy, such as 5-ASAs, sulfazalazine, thiopurines, and all monoclonal antibodies during preconception, pregnancy, and lactation. For small molecule drugs, the consortium recommends they be avoided for at least one month, and in some cases for three months prior to attempting conception, unless there is no alternative for the health of the mother. They should also be avoided during lactation.
Another novel recommendation is that women with IBD may breastfeed with all monoclonal antibodies, including newer IL-23s, even though there is not yet clinical trial data. The recommendation to continue them through pregnancy and lactation is based on placental physiology, as well as on the physiology of monoclonal antibody transfer in breast milk.
While biologic medication can cross the placenta and be detected in infants from 1 to 6 months, levels of biologic drugs detected in breast milk in the study were very low and did not adversely affect infant outcomes. The consensus recommends that women with IBD can breastfeed while on biologic therapy. Additionally, there was no increase in infant infections at 4 months or 12 months if they were exposed to a biologic or thiopurine (or both) during pregnancy.
The consortium also recommends that all women with IBD be started on aspirin by 12 to 16 weeks of pregnancy. This is to reduce the risk of preterm preeclampsia. Women with IBD should also be monitored for venous thromboembolism (VTE) risk, both before delivery as well as in the postpartum period. Offspring of women with IBD should also receive a rotavirus vaccine on schedule, even among infants exposed to biologic therapy in utero.
“A unique aspect of this consensus conference was the geographically diverse representation from around the globe,” said Millie D. Long MD, MPH, co-chair of the Global Consensus Conference and chief of the Division of Gastroenterology and Hepatology at the University of North Carolina at Chapel Hill. “Through this international collaboration, we ensured that all recommendations were feasible and appropriate for women with IBD. In addition, we included patient representatives from each continent to maximize the role of the patient voice in determining best practices of care. We hope that this consensus statement will provide a blueprint for evidence-based management of women with IBD, from pre-conception to post-delivery.”
The PIANO research study, a national study of women with IBD and their children around the U.S., enrolled 2,268 pregnant women with IBD who had 1,702 live births. Among the women, 598 IBD mothers were exposed to steroids during pregnancy. Compared to unexposed mothers, those on steroids had higher rates of preterm birth, low birth weight infants, and infants being admitted to the neonatal intensive care unit. However, there was no increase in birth defects, brain deficits, or infant infection based on steroid use. The researchers concluded that steroid use may be a marker of active disease, which is the real driver of these outcomes. Active disease during pregnancy was more common in patients with ulcerative colitis and led to increased miscarriage.
The study found no reduction in brain development or developmental milestones based on maternal IBD medication use. Infants of mothers with IBD who go to daycare were not more likely to get infections than other children based on medication exposure during pregnancy.
The Global Consensus Consortium consisted of 50 experts from around the world, including IBD specialists, teratologists, maternal fetal medicine specialists, patient advocates, and surgeons. The members of the group convened to review and assess current data and come to an agreement on best practices based on these data. They used the GRADE process (Grading of Recommendations Assessment, Assessment, Development, and Evaluation) when appropriate and the RAND process (Research and Development) in those instances where expert opinion was needed to guide consistent practice.
Reference:
Mahadevan, UmaAbreu, Maria et al., Global Consensus Statement on the Management of Pregnancy in Inflammatory Bowel Disease, Clinical Gastroenterology and Hepatology, DOI: 10.1016/j.cgh.2025.04.005
Powered by WPeMatico

New Delhi: A senior pharmaceutical executive was duped of more than Rs 1.1 crore in a high-profile cyber fraud where two men, posing as representatives of Abbott Pharmaceutical UK and the World Health Organization (WHO), lured him into a fake kola nut trade deal. The case came to light after Kolkata Police arrested the accused from Delhi.
The accused, identified as Ejike Benjamin Nwabunwanne and Believe Onyeacholem, were nabbed from their rented residence in Mahavir Enclave, South West Delhi. According to investigators, the duo used forged WHO and pharma documents, fake email accounts, and WhatsApp communication to convince the victim of the scheme’s legitimacy. Once trust was established, the executive was persuaded to transfer over ₹1.1 crore.
During the raid, police recovered a large cache of incriminating material, including 12 Android phones, two keypad mobiles, a laptop, a Wi-Fi router, multiple UK SIM cards, ATM cards, and a pen drive containing fabricated letters and a database of other potential targets.
Authorities noted that this is not the first time pharma executives have been targeted by international cyber fraudsters. Similar scams involving impersonation of reputed global organisations have been reported earlier this year, raising concerns over the sector’s vulnerability to such sophisticated attacks.
As per a report by the Times of India, the arrests are part of a larger crackdown on organised cybercrime networks targeting pharmaceutical professionals across the country. The two accused remain in police custody as further investigations continue to trace their wider network.
Powered by WPeMatico
According to a recent study adding perioperative pembrolizumab to standard therapy such as surgery and radiotherapy with or without cisplatin consistently improves event-free survival (EFS) in patients with locally advanced head and neck squamous-cell carcinoma (HNSCC), researchers have discovered. Significantly, this increase in EFS was seen in patients with various levels of programmed death ligand 1 (PD-L1) expression, with no adverse effect on surgical completion and with no new safety issues. The study was published in The New England Journal of Medicine by Ravindra U. and colleagues.
HNSCC is a highly recurrant cancer, and outcomes with surgery and adjuvant treatment continue to be suboptimal for most patients. Immunotherapy, such as checkpoint inhibition with agents like pembrolizumab, has been of value in recurrent and metastatic disease, but its place in locally advanced disease treated with curative intent has remained unclear. This large phase 3 trial gives vital proof that the addition of pembrolizumab in both the neoadjuvant and adjuvant environments can enhance long-term outcomes.
This open-label, phase 3 randomized trial included patients with locally advanced HNSCC. The participants were randomly assigned in a 1:1 ratio to receive:
• Pembrolizumab group: 2 cycles of neoadjuvant pembrolizumab and then 15 cycles of adjuvant pembrolizumab (200 mg every 3 weeks) plus standard treatment.
• Control group: Standard treatment alone (surgery and radiotherapy ± cisplatin).
The main endpoint was event-free survival (EFS), which was measured sequentially in patients with CPS ≥10, CPS ≥1, and the overall population.
Key Results
• 714 participants were randomized: 363 to pembrolizumab and 351 to control. Of these, 234 pembrolizumab vs. 231 control patients had CPS ≥10, and 347 pembrolizumab vs. 335 control patients had CPS ≥1.
• Surgical completion rate: ~88% in both groups.
• Median follow-up: 38.3 months.
• Event-free survival at 36 months:
• CPS ≥10 population: 59.8% (pembro) vs. 45.9% (control); HR 0.66; 95% CI 0.49–0.88; P=0.004.
•CPS ≥1 population: 58.2% vs. 44.9%; HR 0.70; 95% CI 0.55–0.89; P=0.003.
• Total population: 57.6% vs. 46.4%; HR 0.73; 95% CI 0.58–0.92; P=0.008.
• Grade ≥3 treatment-related adverse events: 44.6% (pembro) vs. 42.9% (control).
• Deaths due to treatment: 1.1% (pembro) vs. 0.3% (control).
• Immune-mediated grade ≥3 adverse events: 10.0% in the pembro group.
This extensive phase 3 trial reaffirms that perioperative pembrolizumab added to surgery and adjuvant therapy greatly enhances event-free survival in locally advanced HNSCC without sacrificing surgical procedure or adding new safety issues. The trial is a significant advancement in the management of head and neck cancer, with immunotherapy entering earlier stages of disease.
Reference:
Uppaluri, R., Haddad, R. I., Tao, Y., Le Tourneau, C., Lee, N. Y., Westra, W., Chernock, R., Tahara, M., Harrington, K. J., Klochikhin, A. L., Braña, I., Vasconcelos Alves, G., Hughes, B. G. M., Oliva, M., Pinto Figueiredo Lima, I., Ueda, T., Rutkowski, T., Schroeder, U., Mauz, P.-S., … KEYNOTE-689 Investigators. (2025). Neoadjuvant and adjuvant pembrolizumab in locally advanced head and neck cancer. The New England Journal of Medicine, 393(1), 37–50. https://doi.org/10.1056/NEJMoa2415434
Powered by WPeMatico

Researchers have found in a new cluster randomized trial that selecting men for osteoporosis screening by fracture risk factors and using a centralized screening model enhanced screening rates, treatment initiation, and medication adherence. The findings, published in JAMA, highlight a potential shift in how osteoporosis prevention and care can be effectively implemented in men, a group often underdiagnosed and undertreated for bone health.
The study included older male participants who were identified through primary care practices. Rather than relying solely on opportunistic screening during clinic visits, the intervention used a centralized process that flagged high-risk individuals based on established fracture risk profiles. These men were then invited for dual-energy X-ray absorptiometry (DXA) testing and, if indicated, were offered treatment and follow-up support.
Compared to usual care, the risk-based centralized strategy led to significantly higher screening completion rates. Importantly, it also increased the number of men who started pharmacologic therapy for osteoporosis, with better persistence and adherence to prescribed medications. This is particularly relevant given that men tend to present later in the course of osteoporosis, often after experiencing a fragility fracture, leading to worse outcomes compared to women.
The authors suggest that integrating centralized screening pathways within health systems may reduce the burden on primary care providers, while ensuring that men at greatest risk are not overlooked. Such approaches could ultimately reduce fracture incidence, health care costs, and disability related to osteoporosis.
Further research is needed to evaluate scalability across diverse populations and health systems, as well as to assess long-term impacts on fracture prevention and mortality. Still, the results add to growing evidence that proactive, risk-based, and system-level interventions can close existing gaps in men’s osteoporosis care.
Reference:
Crandall, C. J., et al. (2025). Effect of risk-based, centralized screening on osteoporosis detection and treatment in men: A cluster randomized clinical trial. JAMA. https://jamanetwork.com/journals/jama/fullarticle/xxxx
Powered by WPeMatico
Powered by WPeMatico
