How genetics and lifestyle drive dilated cardiomyopathy
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
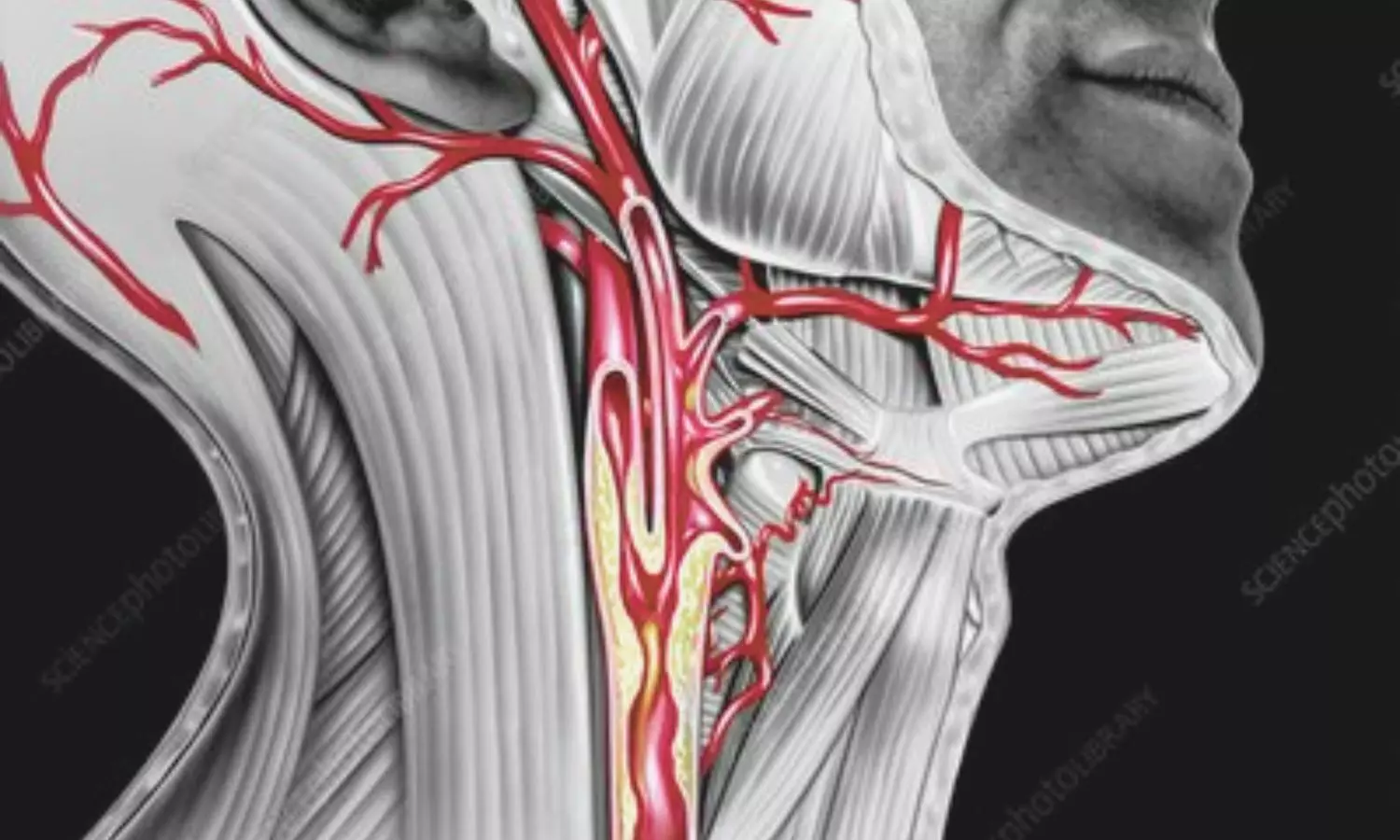
China: A prospective cohort study published in BMJ Open has revealed a strong link between long-term atherogenic index of plasma (AIP) levels and the development and progression of carotid atherosclerosis (CAS). The research, conducted by Hui Li and colleagues from the Department of Health Management Center, Hunan Provincial People’s Hospital, highlights the potential of AIP as an important biomarker for identifying individuals at higher risk of subclinical atherosclerosis.
The study followed 528 adults who underwent annual health examinations over three years from January 2019 to December 2021. Participants were divided into quartiles based on their AIP levels, and carotid atherosclerosis was evaluated using high-resolution ultrasonography. CAS progression was defined as the appearance of new carotid plaques or a significant increase in carotid intima-media thickness (CIMT) compared to baseline measurements.
The notable study findings were as follows:
The analysis demonstrated that the relationship between AIP and CAS risk followed an approximately linear pattern, reinforcing the importance of monitoring AIP over time. According to the authors, these findings suggest that tracking changes in AIP trajectories during routine health check-ups could help identify individuals at heightened risk earlier, allowing for preventive strategies to be implemented before significant vascular damage occurs.
The researchers emphasized that AIP, a marker derived from triglyceride and HDL cholesterol levels, could serve as a cost-effective and easily accessible tool in cardiovascular risk assessment. “Regular monitoring of AIP trends may provide valuable insights for early detection of carotid atherosclerosis and guide targeted interventions,” they noted.
Despite its strengths, including the use of a three-year follow-up and trajectory-based analysis, the study had certain limitations. Being a single-center investigation, the findings may not fully represent broader or high-risk populations. The absence of data on lifestyle factors, inflammatory markers, and genetic variables also restricts the understanding of underlying mechanisms. Furthermore, as all participants were from China, applicability to other ethnic or demographic groups may be limited.
“Nevertheless, the study emphasizes the value of incorporating AIP into regular health assessments. By identifying individuals with persistently high or rising AIP levels, clinicians may be able to intervene earlier to prevent or slow the development of carotid atherosclerosis, ultimately reducing the risk of cardiovascular events such as stroke and heart attack,” the authors concluded.
Reference:
Li H, Duan J, Chen J, Tan C, Hu C, Peng J. Association between long-term atherogenic index of plasma and carotid atherosclerosis: a prospective cohort study of a health examination population. BMJ Open. 2025 Jul 30;15(7):e098874. doi: 10.1136/bmjopen-2025-098874. PMID: 40738628.
Powered by WPeMatico

Researchers have found in a new study that pregnancy-associated acute kidney injury poses a major risk to maternal health in low- and middle-income countries. Therefore strengthening prevention strategies for common causes and expanding antenatal care access can help minimize harmful effects on both mothers and babies. The study was published in the journal of Bull World Health Organ by Tran PNT and colleagues.
The review summarised data from 43 studies, and 40 of these went into the final meta-analysis. Search databases covered Cochrane Central Register of Controlled Trials, Embase, Google Scholar, OvidMedline, ProQuest, and Scopus for studies published between 2013 and 2025. Exclusively, the studies based on the Kidney Disease: Improving Global Outcomes (KDIGO) diagnostic criteria were considered for statistical pooling. The study also performed subgroup analysis and meta-regression to assess factors underlying heterogeneity in results.
Key findings
The combined incidence of PA-AKI was 91 cases per 10,000 pregnancies (95% CI: 63–133).
The incidence was highest in World Health Organization African Region studies, where it was 254 per 10,000 pregnancies (95% CI: 152–421).
These results indicate that the burden of PA-AKI is unevenly distributed and is heavily dependent on regional healthcare infrastructure and maternal health resources.
The condition was linked to high maternal and neonatal mortality.
The fatality of the case was 10.8% (95% CI: 7.6–15.3), and death during neonatal life or stillbirth resulted in 29.8% of the cases (95% CI: 24.2–36.1).
Additionally, mothers with PA-AKI had an 18.8 times increased risk of maternal death (95% CI: 10.0–35.5) compared to those without the condition, and there was a 4.6 times increased risk (95% CI: 2.1–10.0) of poor fetal outcomes, such as preterm birth and low birth weight.
Pre-eclampsia emerged as the most common cause of PA-AKI, at 44.1% of the cases, followed by hemorrhage (26.2%) and sepsis (16.5%).
These etiologies underscore the preventable nature of most cases of PA-AKI through early obstetric intervention, infection control, and enhanced maternal monitoring during pregnancy.
The research points to the fact that PA-AKI is a significant public health threat among LMICs, with a high risk of mortality for both mother and fetus. Interventions targeted specifically towards public health programs and strengthened maternal healthcare facilities can go a long way toward mitigating incidence and outcomes of PA-AKI in low-resource environments.
Reference:
Tran, P. N. T., Wannakittirat, A., Luyckx, V., Wiles, K., Yadla, M., Chakravarthi, R., Ostermann, M., Wu, V. C., Mehta, R. L., & Srisawat, N. (2025). Incidence of pregnancy-associated acute kidney injury in low- and middle-income countries: a meta-analysis. Bulletin of the World Health Organization, 103(8), 493–506. https://doi.org/10.2471/BLT.24.293077
Powered by WPeMatico
New research in Diabetes, Obesity and Metabolism reveals that metformin, a medication traditionally prescribed to treat diabetes, is linked to lower risks of dementia and early death.
In the study by investigators at Taipei Medical University that included 452,777 adults with varying degrees of overweight and obesity, 35,784 cases of dementia and 76,048 deaths occurred over 10 years. Metformin users exhibited significantly lower risks of both dementia and all-cause death than nonusers.
The benefits of metformin were seen across all categories of overweight, obesity, and severe obesity, with 8–12% lower risks of dementia and 26–28% lower risks of death.
“Although our study results are promising for metformin’s effects on dementia and mortality, further research is required to explore the mechanisms involved,” said co-corresponding author Chiehfeng Chen, MD, PhD, MPH.
Reference:
Yu-Liang Lin, Protective effect of metformin against dementia in patients with obesity: Results from a global federated health network analysis, Diabetes Obesity and Metabolism, DOI: 10.1111/dom.16647.
Powered by WPeMatico

A new study published in the Journal of American Medical Association showed that during endocrine neck surgery, fiber-based near-infrared autofluorescence (NIRAF) improves parathyroid gland identification and might potentially lower complications.
Accurately identifying and protecting parathyroid glands (PGs) during parathyroidectomy and thyroidectomy is essential since their removal or injury can result in hypoparathyroidism. Thus, this study determined if fiber-based NIRAF lowers the incidence of hypoparathyroidism and enhances the number of PGs discovered intraoperatively.
From March 2020 to July 2024, this clinical study with a 6-month follow-up was carried out. It comprised 3 junior (less than 5 years of experience) and four senior (more than 10 years of experience) surgeons from 4 medical centers across the US. A total of 398 individuals (2 withdrew) got parathyroidectomy, and 354 patients had total/completion thyroidectomy, out of the 754 patients who were recruited and 752 who were randomized. The use of fiber-based NIRAF during thyroid and parathyroidectomy was one of the primary therapies.
The primary outcome (94.4%) was examined for 712 out of 752 randomly assigned individuals. In all, 159 patients had traditional surgery, and 161 got parathyroidectomy with NIRAF. Furthermore, 178 had conventional surgery, and 176 had thyroidectomies utilizing NIRAF.
Using NIRAF for targeted operations did not substantially increase the mean number of PGs found during parathyroidectomy (mean, NIRAF, 1.6; 95% CI, 1.4-1.8 vs. control, 1.5; 95% CI, 1.4-1.7). The mean number of PGs found by the surgeons utilizing NIRAF during bilateral explorations was higher (mean NIRAF, 3.5; 95% CI, 3.4-3.7 vs. control, 3.2; 95% CI, 3.0-3.4; P <.001).
The mean number of PGs detected during thyroidectomy was higher when NIRAF was used (mean NIRAF, 3.3; 95% CI, 3.2-3.4 versus control, 2.8; 95% CI, 2.7-3.0; P <.001). Hypoparathyroidism following thyroidectomy did not significantly vary at the last follow-up (NIRAF: 3 of 176 patients [1.7%]; control: 6 of 176 patients [3.4%]) or during the transitory period (NIRAF: 48 of 173 patients [27.8%]; control: 44 of 169 patients [26%]).
Overall, this study suggest fiber-based NIRAF, may assist surgeons in confidently identifying more PGs during bilateral exploration, but it offers no further benefit during targeted surgeries. Regardless of the method, the number of PGs found increased during thyroidectomy. Even while NIRAF had no discernible effect on short-term patient outcomes, surgeons may find it useful as an intraoperative tool in situations where alternative techniques for PG tissue confirmation are not accessible.
Source:
Cousart, A. G., Kiernan, C. M., Willmon, P. A., Thomas, G., Wang, T. S., Gauger, P. G., Duh, Q.-Y., Underwood, H. J., Jackson, A., Patel, A., Mahadevan-Jansen, A., & Solórzano, C. C. (2025). Near-infrared autofluorescence for parathyroid detection during endocrine neck surgery: A randomized clinical trial: A randomized clinical trial. JAMA Surgery. https://doi.org/10.1001/jamasurg.2025.2233
Powered by WPeMatico
People who practised blowing through a conch shell regularly for six months experienced a reduction in their symptoms of obstructive sleep apnoea (OSA), according to a small randomised controlled trial published today (Monday) in ERJ Open Research.
OSA is a common sleep disorder where breathing repeatedly stops during the night due to a blocked airway. It leads to loud snoring, restless sleep and daytime sleepiness. It also increases the risk of high blood pressure, heart disease, and stroke.
Blowing the conch shell, or shankh blowing, has been part of Indian culture for thousands of years. The new research showed that people with moderate OSA who practised shankh blowing slept better, felt more alert during the day and had fewer breathing interruptions at night. The researchers say conch blowing is a simple, low-cost intervention that could help reduce symptoms without the need for medication or machines.
The study was led by Dr Krishna K Sharma from the Eternal Heart Care Centre and Research Institute in Jaipur, India. He said: “The standard treatment for OSA is a continuous positive airway pressure machine, or CPAP, which keeps the patient’s airway open by blowing air through a facemask throughout the night. While effective, many patients find it uncomfortable and struggle to use it consistently.
“In my clinical practice, several patients reported feeling more rested and experiencing fewer symptoms after regularly practising shankh blowing – a traditional yogic breathing exercise involving exhaling through a conch shell. These observations led us to design a scientific study to rigorously test whether this simple, ancient practice could serve as a meaningful therapy for people with OSA.”
The study included 30 people with moderate OSA, aged between 19 and 65, who were assessed at the Eternal Heart Care Centre and Research Institute between May 2022 and January 2024. They were tested with polysomnography, meaning they are monitored throughout a night’s sleep, and asked questions about the quality of their sleep and how sleepy they feel during the day.
They were randomly assigned to either be trained to practise blowing through a conch shell (16 patients) or to practise a deep breathing exercise (14 patients). Participants were provided with a traditional shankh used in yogic practices. They were trained in person at the clinic by a study team member before beginning home-based practice. Participants were encouraged to practise at home for a minimum of 15 minutes, five days per week. After six months, the patients were reassessed.
Compared to the people who practised deep breathing, the people who practised shankh blowing were 34% less sleepy during the daytime, they reported sleeping better and polysomnography revealed that they had four to five fewer apnoeas (where breathing stops during sleep) per hour on average. They also had higher levels of oxygen in their blood during the night.
Dr Sharma said: “The way the shankh is blown is quite distinctive. It involves a deep inhalation followed by a forceful, sustained exhalation through tightly pursed lips. This action creates strong vibrations and airflow resistance, which likely strengthens the muscles of the upper airway, including the throat and soft palate – areas that often collapse during sleep in people with OSA. The shankh’s unique spiralling structure may also contribute to specific acoustic and mechanical effects that further stimulate and tone these muscles.
“For people living with OSA, especially those who find CPAP uncomfortable, unaffordable, or inaccessible, our findings offer a promising alternative. Shankh blowing is a simple low-cost, breathing technique that could help improve sleep and reduce symptoms without the need for machines or medication.
“This is a small study, but we are now planning a larger trial involving several hospitals. This next phase will allow us to validate and expand on our findings in a broader, more diverse population and assess how shankh blowing performs over longer periods. We also want to study how this practice affects airway muscle tone, oxygen levels and sleep in greater detail. We’re particularly interested in comparing shankh blowing with standard treatments like CPAP, and in examining its potential help in more severe forms of OSA.”
Professor Sophia Schiza, Head of the ERS group on sleep disordered breathing, based at the University of Crete, Greece, who was not involved in the research said: “Obstructive sleep apnoea is a common disease around the world. We know that OSA patients have poor quality of sleep, and higher risks of high blood pressure, strokes and heart disease. A proportion of patients experience sleepiness during the day. While CPAP and other treatments are available based on careful diagnosis of disease severity, there is still need for new treatments.
“This is an intriguing study that shows the ancient practice of shankh blowing could potentially offer an OSA treatment for selected patients by targeting muscles training. A larger study will help provide more evidence for this intervention which could be of benefit as a treatment option or in combination with other treatments in selected OSA patients.”
Reference:
Krishna K. Sharma, Rajeev Gupta, Titiksha Choyal, Efficacy of blowing shankh on moderate sleep apnea: a randomised control trial, ERJ Open Research, https://doi.org/10.1183/23120541.00258-2025.
Powered by WPeMatico

A new study in the International Journal of Hygiene and Environmental Health finds parents’ workplace chemical exposure may be linked to a range of behavioral challenges and developmental delays in their children with autism.
Autism is a neurodevelopmental condition that is marked by challenges with social skills, communication struggles and repetitive behaviors. Autism traits can vary widely in how mild or strong they are.
“Past research explored the impact of environmental factors on the likelihood of a child developing autism,” said Irva Hertz-Picciotto, a co-author and professor in the Department of Public Health Sciences and the UC Davis MIND Institute.
“This study is one of the first to connect parental job exposures to the severity of their child’s autism based on the Autism Diagnostic Observation Schedule, 2nd edition” (ADOS-2),” Hertz-Picciotto said. “The ADOS-2 Calibrated Severity Score is considered the ‘gold standard’ diagnostic assessment of autism,” Hertz-Picciotto said.
Hertz-Picciotto directs the UC Davis Environmental Health Sciences Center and has led a large autism study, CHARGE (ChildHood Autism Risks from Genes and Environment), since 2002. The CHARGE study is funded by the National Institute of Environmental Health Sciences. It includes children with autism or other developmental delays and children with typical development.
In collaboration with the UC Davis CHARGE Study team, researchers from the National Institute for Occupational Safety and Health (NIOSH) studied data from over 500 families in the CHARGE study. They focused entirely on children already diagnosed with autism.
Industrial hygienists assessed both mothers’ and fathers’ job histories from three months before pregnancy to birth. They estimated each parent’s exposure to 16 chemicals or agents. This included plastics, car fluids, disinfectants, medicines and other chemicals.
They then matched the data with the children’s autism severity scores (using the ADOS-2) and their behaviors, cognitive skills and daily living skills.
The researchers found these associations among children with autism:
• Plastics and polymers (like polyethylene, polypropylene and polyvinyl chloride or PVC) are linked to poorer cognitive performance, reduced adaptive skills and increased behavioral issues like hyperactivity and social withdrawal.
• Ethylene oxide, a chemical used for sterilizing, is linked to higher autism severity scores and weaker daily living skills.
• Phenol exposure is tied to increased autism severity and behavioral symptoms like hyperactivity, repeated movements or vocalizations.
“Our findings suggest that parental exposure to certain workplace chemicals during key fetal development periods may influence not just autism likelihood, but also severity and functioning outcomes for children with autism,” said lead author Erin McCanlies, formerly with NIOSH’s Health Effects Laboratory Division.
The authors noted important limitations to the study. The number of families may have been too small to find links for less common exposures. The exposure estimates relied on reported job histories and expert judgment, which might not reflect actual exposures. Lastly, while certain agents showed associations with certain autism traits, the study did not prove that those chemicals caused the traits.
The authors say more research is needed to understand how these exposures impact brain development. They also call for including fathers in similar studies on reproductive health and child neurodevelopment, as many associations in this study were linked to paternal exposures.
For instance, the strongest cognitive deficits for children with autism were linked to fathers’ job exposures to plastics and polymers. These exposures correlated with significantly lower skills, including fine motor, visual reception, receptive language, and expressive language.
“This research shows that workplace safety isn’t just about protecting the worker — it’s also about protecting their future children,” said Hertz-Picciotto. “We must consider how workplace chemicals might affect the next generation.”
Reference:
Erin C. McCanlies, Ja Kook Gu, Claudia C. Ma, Wayne T. Sanderson, Yunin J. Ludeña-Rodriguez, Irva Hertz-Picciotto, The effects of parental occupational exposures on autism spectrum disorder severity and skills in cognitive and adaptive domains in children with autism spectrum disorder, International Journal of Hygiene and Environmental Health, https://doi.org/10.1016/j.ijheh.2025.114613.
Powered by WPeMatico

India: A new prospective cohort study published in the Journal of Clinical and Experimental Hepatology has shed light on the patterns of liver injury and recovery in patients with abdominal tuberculosis (ATB) undergoing anti-tuberculosis treatment (ATT).
Conducted by Abhishek Kumar and colleagues from the Department of Gastroenterology, All India Institute of Medical Sciences (AIIMS), Patna, the research highlights how early monitoring and nutritional assessment can play a critical role in preventing severe drug-induced liver injury (DILI).
Patients with extra-pulmonary tuberculosis, including ATB, are known to have a higher risk of developing DILI during ATT. However, in some cases, liver function abnormalities resolve spontaneously through a process known as hepatic adaptation (HA). While previous studies have looked at DILI risk in pulmonary tuberculosis, prospective data specifically focusing on ATB patients have been scarce.
The study followed 140 patients with confirmed ATB and normal baseline liver function tests (LFTs). All participants received the standard four-drug ATT regimen, and their LFTs were monitored at regular intervals. Potential predictors of liver injury progression were assessed using multivariable logistic regression.
The study revealed the following notable findings:
The analysis revealed that low serum albumin levels and vitamin D deficiency were independent predictors of progression from mild LFT abnormalities to DILI. These findings suggest that nutritional status may influence the liver’s ability to adapt during ATT.
When ATT was temporarily halted due to liver injury, complete reintroduction was successful in 65.8% of patients. Pyrazinamide was the drug most frequently linked to reintroduction failure. Importantly, none of the patients who developed DILI progressed to acute liver failure.
The authors note that while liver test abnormalities are common during ATT in ATB patients, nearly half can recover naturally due to hepatic adaptation. Identifying those at higher risk—particularly patients with hypoalbuminemia or vitamin D deficiency—could help clinicians prevent severe outcomes through closer monitoring and early intervention.
The study highlights the importance of regular LFT monitoring during the initial weeks of ATT, alongside nutritional assessment, to improve treatment safety and outcomes in abdominal TB patients.
Reference:
Kumar, A., Kumar, R., Kumar, V., Kumar, S., Marrapu, S., Anand, U., & Priyadarshi, R. N. (2025). Patterns of Liver Injury and Adaptation in Patients with Abdominal Tuberculosis on Antituberculosis Treatment: A Prospective Cohort Study. Journal of Clinical and Experimental Hepatology, 103124. https://doi.org/10.1016/j.jceh.2025.103124
Powered by WPeMatico
