Ultra-processed foods linked to heightened disease activity in early multiple sclerosis
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Mindfulness meditation may help people struggling with concurrent depression and Internet gaming disorder, according to a study. Guang-Heng Dong and colleagues treated 59 people with depression and Internet gaming disorder (IGD)-which is characterized by excessive and dysregulated video game playing.
About a third of people struggling with IGD also suffer from depression. For some, gaming becomes the only way to feel pleasure in an otherwise painful or colorless world. Of the 59 participants, 27 engaged in progressive muscle relaxation exercises and 32 engaged in mindfulness meditation training tailored for addiction.
For example, participants were taught to observe and experience their cravings as they rose and then dissipated, like a wave. Those who engaged in mindfulness meditation training for four weeks, with two 2.5–3.5-hour sessions per week, showed a significant decrease in depressive symptoms, a significant decrease in scores on the Internet Addiction Test, and a significant reduction in craving for video games. Participants who engaged in progressive muscle relaxation showed less improvement in symptoms.
Brain imaging showed that meditation practice decreased brain responses to gaming cues and increased activity in the lentiform nucleus, which could potentially indicate lessening anhedonia-dysfunction of the pleasure-seeking and pleasure-enjoying system. According to the authors, mindfulness meditation is a promising treatment for IGD and depression when they occur together.
Reference:
Luo, X., et al. (2025) Mindfulness meditation reduces symptoms and modulates neural circuitry in comorbid internet gaming disorder and depression. PNAS Nexus. doi.org/10.1093/pnasnexus/pgaf277
Powered by WPeMatico

A study found that a 2% sweet vanilla scent effectively distracted children aged 7-9 years, reducing injection pain during infiltration anesthesia for maxillary molars. The findings suggest that simple sensory interventions may help ease pediatric dental anxiety and discomfort.
Published in Journal of Integrative & Complementary Medicine (Shadman et al., 2025), the randomized, double-blind, controlled trial involved 48 children in need of local anesthesia for primary maxillary molars.
The children were split into three groups: a control group with no scent, a group that received anesthesia in a room filled with 2% vanilla scent, and a group exposed to the vanilla scent for 30 seconds before injection. Pain was assessed using both subjective scales (Wong-Baker Faces Pain Rating Scale) and objective scales (FLACC behavioural pain scale), along with physiological measures like heart rate and oxygen saturation. Results showed significantly lower FLACC scores and reduced heart rates in the scented intervention groups compared to control. Oxygen saturation was also better when using the scented room condition. However, the Wong-Baker self-report scores did not differ significantly across groups.
What this really means is that vanilla aromatherapy, which costs little and is easy to implement, could be a useful non-pharmacological strategy in pediatric dentistry. Though subjective pain didn’t always change, the behavioural and physiological responses suggest that children experienced less distress. The authors do note the need for larger trials and testing in other age ranges to confirm and generalize the findings.
Powered by WPeMatico
As a wound heals, it goes through several stages: clotting to stop bleeding, immune system response, scabbing, and scarring.
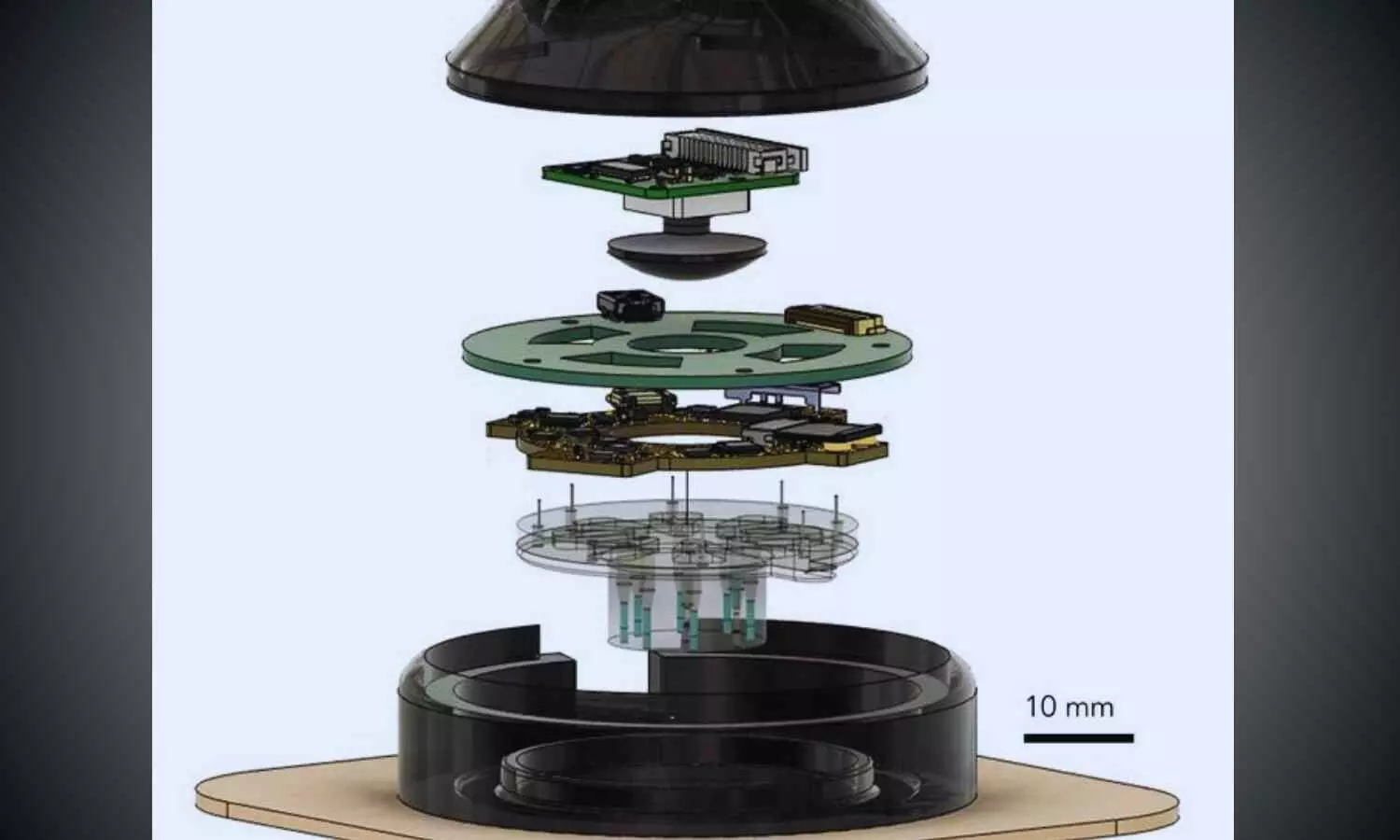
A wearable device called “a-Heal,” designed by engineers at the University of California, Santa Cruz, aims to optimize each stage of the process. The system uses a tiny camera and AI to detect the stage of healing and deliver a treatment in the form of medication or an electric field. The system responds to the unique healing process of the patient, offering personalized treatment.
The portable, wireless device could make wound therapy more accessible to patients in remote areas or with limited mobility. Initial preclinical results, published in the journal npj Biomedical Innovations, show the device successfully speeds up the healing process.
A team of UC Santa Cruz and UC Davis researchers, sponsored by the DARPA-BETR program and led by UC Santa Cruz Baskin Engineering Endowed Chair and Professor of Electrical and Computer Engineering (ECE) Marco Rolandi, designed a device that combines a camera, bioelectronics, and AI for faster wound healing. The integration in one device makes it a “closed-loop system”—one of the firsts of its kind for wound healing as far as the researchers are aware.
“Our system takes all the cues from the body, and with external interventions, it optimizes the healing progress,” Rolandi said.
The device uses an onboard camera, developed by fellow Associate Professor of ECE Mircea Teodorescu and described in a Communications Biology study, to take photos of the wound every two hours. The photos are fed into a machine learning (ML) model, developed by Associate Professor of Applied Mathematics Marcella Gomez, which the researchers call the “AI physician” running on a nearby computer.
“It’s essentially a microscope in a bandage,” Teodorescu said. “Individual images say little, but over time, continuous imaging lets AI spot trends, wound healing stages, flag issues, and suggest treatments.”
The AI physician uses the image to diagnose the wound stage and compares that to where the wound should be along a timeline of optimal wound healing. If the image reveals a lag, the ML model applies a treatment: either medicine, delivered via bioelectronics; or an electric field, which can enhance cell migration toward wound closure.
The treatment topically delivered through the device is fluoxetine, a selective serotonin reuptake inhibitor which controls serotonin levels in the wound and improves healing by decreasing inflammation and increasing wound tissue closure. The dose, determined by preclinical studies by the Isseroff group at UC Davis group to optimize healing, is administered by bioelectronic actuators on the device, developed by Rolandi. An electric field, optimized to improve healing and developed by prior work of the UC Davis’ Min Zhao and Roslyn Rivkah Isseroff, is also delivered through the device.
The AI physician determines the optimal dosage of medication to deliver and the magnitude of the applied electric field. After the therapy has been applied for a certain period of time, the camera takes another image, and the process starts again.
While in use, the device transmits images and data such as healing rate to a secure web interface, so a human physician can intervene manually and fine-tune treatment as needed. The device attaches directly to a commercially available bandage for convenient and secure use.
To assess the potential for clinical use, the UC Davis team tested the device in preclinical wound models. In these studies, wounds treated with a-Heal followed a healing trajectory about 25% faster than standard of care. These findings highlight the promise of the technology not only for accelerating closure of acute wounds, but also for jump-starting stalled healing in chronic wounds.
The AI model used for this system, which was led by Assistant Professor of Applied Mathematics Marcella Gomez, uses a reinforcement learning approach, described in a study in the journal Bioengineering, to mimic the diagnostic approach used by physicians.
Reinforcement learning is a technique in which a model is designed to fulfill a specific end goal, learning through trial and error how to best achieve that goal. In this context, the model is given a goal of minimizing time to wound closure, and is rewarded for making progress toward that goal. It continually learns from the patient and adapts its treatment approach.
The reinforcement learning model is guided by an algorithm that Gomez and her students created called Deep Mapper, described in a preprint study, which processes wound images to quantify the stage of healing in comparison to normal progression, mapping it along the trajectory of healing. As time passes with the device on a wound, it learns a linear dynamic model of the past healing and uses that to forecast how the healing will continue to progress.
“It’s not enough to just have the image, you need to process that and put it into context. Then, you can apply the feedback control,” Gomez said.
This technique makes it possible for the algorithm to learn in real-time the impact of the drug or electric field on healing, and guides the reinforcement learning model’s iterative decision making on how to adjust the drug concentration or electric-field strength.
Now, the research team is exploring the potential for this device to improve healing of chronic and infected wounds.
Reference:
Li, H., Yang, Hy., Lu, F. et al. Towards adaptive bioelectronic wound therapy with integrated real-time diagnostics and machine learning–driven closed-loop control. npj Biomed. Innov. 2, 31 (2025). https://doi.org/10.1038/s44385-025-00038-6.
Powered by WPeMatico

Patients who have a new type of lens implanted in their eyes during surgery for cataracts or to correct their eyesight have excellent or good vision over distances both near and far, and often no longer need spectacles for reading.
Research presented today (Sunday) at the 43rd Congress of the European Society of Cataract and Refractive Surgeons (ESCRS) [1] evaluated outcomes for around 200 patients in 17 sites in Europe and Asia-Pacific who had surgery to implant the TECNIS PureSEETM, a purely refractive extended depth of field (EDF) presbyopia correction Intraocular Lens (IOL). Presbyopia is the condition that affects all people as they age, making it harder to focus clearly on close objects and text.
The study looked at visual acuity after surgery: how well the patients could see over far, intermediate and near distances on the logMAR visual acuity charts used by ophthalmologists that consist of rows of letters that become smaller as they go down the chart. It also measured Manifest Refraction Spherical Equivalent (MRSE) – a way of quantifying the refractive errors of the eye. In addition, the study reported on how patients were managing after surgery in terms of whether or not they needed spectacles for reading, how satisfied they were with their outcomes and whether they would recommend the lens to others.
Data were available for 238 patients at the time of the Congress, making it one of the biggest studies to report on this type of lens so far. The findings showed that the EDF presbyopia correction IOL, on average, provided excellent distance, very good intermediate, and functional near vision without glasses, with little refractive error. (Full details of results are in note).
Nearly all patients (96%) reported needing glasses ‘none’ or ‘a little of the time’ for distance vision; 93% reported this for intermediate distances, 62% for near distances, and 85% for overall vision.
For satisfaction with the outcomes, 96% were ‘mostly’ or ‘completely’ satisfied with their distance vision, 94% with intermediate, 73% with near, and 95% with overall vision; 96% would recommend the lens to their family and friends.
Professor Oliver Findl, Chair of the ESCRS Education Committee, is a consultant eye surgeon and head of the ophthalmology department at Hanusch Hospital, Vienna. He presented the findings to the congress.
He said: “The PureSee EDF IOL gave patients excellent distance, very good intermediate and functional near vision, which resulted in high patient satisfaction with less need for spectacles. The data in this study came from several surgical centres throughout Europe and Asia in a ‘real world setting’ outside of the usual clinical trials.
“The category of EDF IOLs, such as the TECNIS PureSee, are a great alternative to multifocal lenses for patients who wish to be less dependent on spectacles after lens surgery and do not want to take the risk of unwanted optical side-effects.”
Currently, when a person requires cataract surgery, their cloudy lens is replaced with an artificial lens. To enable a patient to see objects both near and far, their surgeon may offer them a choice of lenses, such as:
• Monofocal lens, which enables patients to see clearly at one distance point (far, intermediate or near), but which mean they need spectacles for the distances they have not chosen. If surgery is needed on both eyes, patients can choose to have a lens for close-up work in one eye, and another lens for distances in the other eye. This combination is known as monovision and the brain then adjusts to the two distances so that the patient can see both near and far.
• Multifocal lens, which can provide good vision over all distances, without the need for glasses. The lens is split into different zones or concentric rings, with different prescription lengths for each section, which provide clear, complete vision when combined. However, these lenses may cause some unwanted optical side-effects, especially at night.
• Extended depth of field (EDF) lens, which provides good distance and intermediate (arm’s length) vision, but spectacles may still be needed for close work such as reading small print.
“The difference between some of these lenses and the EDF presbyopia correction IOL that we used in this study is that it is a fully ‘refractive’ IOL, meaning it uses variations in the lens curvature to focus light at a single distance. The surface of the lens is smooth and you don’t see bumps or rings,” said Prof. Findl. “This means you have better night vision and don’t see halos, starbursts, glare and other visual disturbances that can occur with other lenses.”
Dr Joaquín Fernández is ESCRS Secretary, CEO of Qvision and Medical Director of Andalusian Ophthalmology Institute at Vithas Hospitals. He was not involved in the research. He commented: “Eye surgery for cataracts or to correct vision is constantly evolving but, so far, the ‘holy grail’ of developing a lens that can give patients good vision over all distances without any visual disturbances has been elusive. These data from a ‘real world’ study are very encouraging and suggest that the available options are expanding to better meet the expectations of our patients. However, other options still need to be explored. We look forward to further results from the study.”
Reference:
Patients who had cataracts removed or their eyesight corrected with a new type of lens have good vision over all distances without spectacles, European Society of Cataract and Refractive Surgeons, Meeting: 43rd Congress of the European Society of Cataract and Refractive Surgeons.
Powered by WPeMatico
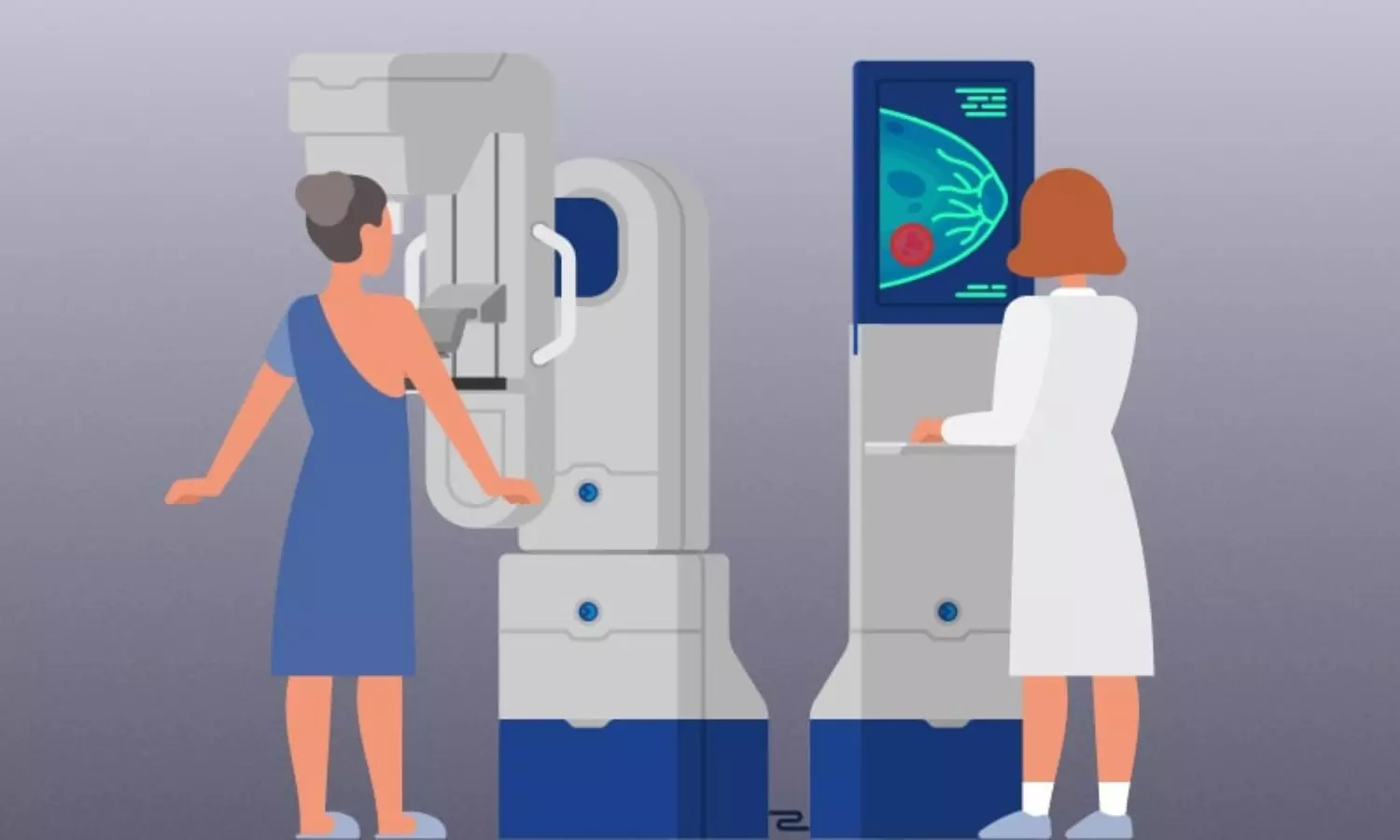
Screening women with dense breasts with both molecular breast imaging (MBI) and digital breast tomosynthesis (DBT) increased overall invasive cancer detection while modestly increasing the recall rate compared with screening only with DBT, according to a new study published today in Radiology, a journal of the Radiological Society of North America (RSNA).
“To our knowledge, this is the first multicenter, prospective evaluation of MBI as a supplement to DBT in women with dense breasts,” said lead author Carrie B. Hruska, Ph.D., professor of medical physics at Mayo Clinic in Rochester, Minnesota.
An estimated 47% of women who undergo breast cancer screening have dense breasts, according to the Centers for Disease Control and Prevention. DBT is an advanced form of mammography that takes multiple X-ray images of the breast from different angles to create a 3D reconstruction of the breast, but it does not detect all breast cancers, especially in women with dense breasts.
MBI is one of several options available for supplemental breast screening for dense breasts, such as breast ultrasound, breast MRI and contrast-enhanced mammography. The Density MATTERS (Molecular Breast Imaging and Tomosynthesis to Eliminate the Reservoir) Trial was designed to assess the performance of screening MBI as a supplement to DBT in women with dense breasts.
For the trial, women with dense breasts from five sites were prospectively enrolled from 2017 to 2022 and underwent two annual screening rounds of DBT and MBI (prevalence screening at Year 1 and incidence screening at Year 2). One-year follow-up after each screening round was completed in September 2024.
Eligible participants included women aged 40–75 years who were asymptomatic and had dense breasts as visually assessed by a radiologist and reported on their last mammogram.
The study cohort included 2,978 participants (mean age 56.8 years). The women were mostly postmenopausal, and 82% had category C breast density. Approximately 80% of participants had no family history of breast cancer, and 98% had no personal history of breast cancer.
Across both screening rounds, 30 breast cancer lesions were detected in 29 participants by MBI only and not found with DBT. Most of these incremental breast cancers were invasive (22 of 30 or 71% of lesions). The median invasive lesion size was 0.9 cm. Among the participants with MBI-only detected breast cancer, 26 of 29 (90%) had node-negative cancers, and 6 of 29 (20%) had node-positive disease.
“MBI detected an additional 6.7 cancers per 1,000 screenings at Year 1 and an additional 3.5 cancers per 1,000 screenings at Year 2,” Dr. Hruska said. “Among the incremental cancers detected only by MBI, 70% were found to be invasive. Additionally, 20% of those incremental cancers were node positive, suggesting that MBI can reveal mammographically occult, clinically important disease.”
In the first screening round, 7 of 2,978 participants (2.4 per 1,000 screened) were diagnosed with node-positive cancers. DBT alone detected 4 of 7 (57%), and DBT plus MBI detected 7 of 7 (100%).
In Year 2, 6 of 2,590 participants (2.3 per 1,000 screened) had node-positive cancers. DBT alone detected 1 of 6 (16%) and DBT plus MBI detected 4 of 6 (67%). Neither modality detected 2 of the 6 node-positive cancers (33%).
“Someone who’s having their routine annual screen every year should not be diagnosed with advanced breast cancer,” Dr. Hruska said. “That’s just unacceptable. With a supplemental screening every few years, we hope to find cancers earlier and see the diagnosis of advanced cancer go way down.”
Dr. Hruska said one of the strengths of the Density MATTERS trial was the mix of academic medical centers and community hospitals involved. Participating centers also included MD Anderson Cancer Center, Henry Ford Health System, ProMedica Breast Care (regional practice in Ohio), and a Mayo Clinic Health System site in La Crosse, Wisconsin.
“The enrollment of 12% minority patients extends the generalizability of our findings,” she said.
She said the trial results provide important data for healthcare institutions assessing the best modality for supplemental breast screening.
“I don’t want to discourage anyone from getting a mammogram, because they absolutely should,” Dr. Hruska said. “However, DBT doesn’t find all cancers, and women need to understand its limitations and consider how supplemental screening can fill the gap.”
According to Dr. Hruska, MBI is considered safe for routine screening, is well-tolerated by patients and is relatively inexpensive.
“MBI uses a well-established radiotracer that’s been used in cardiac imaging for a really long time,” she said. “It has fewer risks than other modalities and no contrast reactions. If a woman has a choice of modalities, it’s important that she understands the benefits and risks of each and be involved in the decision-making.”
Reference:
Carrie B. Hruska , Katie N. Hunt, Nicholas B. Larson, Molecular Breast Imaging and Digital Breast Tomosynthesis for Dense Breast Screening: The Density MATTERS Trial, Radiology, https://doi.org/10.1148/radiol.243953
Powered by WPeMatico

Canada: Dry eye syndrome (DES) emerges as a frequently overlooked extraintestinal manifestation of inflammatory bowel disease (IBD), a systematic review and meta-analysis published in Frontline Gastroenterology has revealed.
Powered by WPeMatico
A new study published in the journal of BMC Nephrology showed that as a non-invasive biomarker to distinguish between steroid-resistant nephrotic syndrome (SRNS) and steroid-sensitive nephrotic syndrome (SSNS), urinary neutrophil gelatinase-associated lipocalin (NGAL) has great promise for supporting early diagnosis, risk assessment, and treatment.
Massive proteinuria (more than 40 mg/m^2 per hour) causes hypoalbuminemia (less than 30 g/L), which leads to hyperlipidemia, edema, and other problems. Nephrotic syndrome is a clinical illness characterized by this condition. Although patient response varies, corticosteroids are usually used as the first line of treatment.
Early in the course of the disease, it’s critical to distinguish between steroid-sensitive nephrotic syndrome (SSNS) and steroid-resistant nephrotic syndrome (SRNS), as the latter is linked to a higher risk of unfavorable long-term consequences. One possible non-invasive indicator of renal impairment is neutrophil gelatinase-associated lipocalin (NGAL), a biomarker generated in response to tubular injury. Therefore, this systematic review and meta-analysis attempted to establish if urine NGAL values change between patients with SRNS, SSNS, and healthy controls.
Following the PRISMA standards, this research performed a systematic review and meta-analysis of papers that reported NGAL levels in SSNS and SRNS. Using PubMed, Web of Science, Scopus, ScienceDirect, and the WHO Virtual Health Library Regional, a thorough literature search was carried out. A random-effects model was used for the statistical analysis in order to determine the standardized mean difference (SMD) with a 95% confidence range.
There were 16 investigations in all. Both SSNS and SRNS patients had much greater urine NGAL levels than healthy controls, according to meta-analyses. In comparison to healthy controls, SSNS and SRNS patients had substantially higher urinary NGAL levels (SMD = 0.78 (95% CI: 0.434–1.128, P <.001) and SMD = 2.56 (95% CI: 1.152–3.971, P <.001), respectively.
Urinary NGAL levels were significantly greater in SRNS patients than in SSNS patients (SMD = 1.889, 95% CI: 0.819–2.959, P <.001). Urinary NGAL has a moderate to great discriminative power in differentiating between SRNS and SSNS, according to ROC analysis from many investigations.
Overall, urinary NGAL showed great promise as a non-invasive, early indicator of steroid resistance in nephrotic syndrome. Its incorporation in clinical evaluation processes is supported by its relevance across populations, biological plausibility, and diagnostic accuracy. With more research, NGAL may be crucial in helping children patients with nephrotic syndrome achieve better results, reduce needless steroid exposure, and customize treatment plans.
Source:
Abdalla, A., Ali, A., Abufatima, I. O., Majzoub, S., Elbasheer, T. A. E., Ahmed, S. M. A. O., Osman, S., Khalid, Y. K. K., Elamir, A., Khalid, H. K. K., Abdelmutalib, N. M. A., & Mohamed, S. O. O. (2025). Use of urinary NGAL in steroid-resistant vs. steroid-sensitive nephrotic syndrome: a systematic review and meta-analysis. BMC Nephrology, 26(1). https://doi.org/10.1186/s12882-025-04420-9
Powered by WPeMatico

France: Even moderate alcohol consumption significantly increases the risk of squamous cell cancers of the upper aerodigestive tract (UADT), a large pooled analysis of 28 prospective cohorts published in the JNCI: Journal of the National Cancer Institute has shown.
Powered by WPeMatico
