Standardized criteria for amino acid PET imaging could improve diagnosis and treatment of brain metastases
Powered by WPeMatico
Powered by WPeMatico
Reframing Aspirin’s Role in Primary Prevention: Evolving evidence has refined our understanding of aspirin’s role in primary prevention. While earlier trials established cardiovascular benefits, more recent data emphasize the importance of patient selection to optimise outcomes. A 2019 meta-analysis (N=164,225) showed aspirin reduced serious vascular events by 12% and non-fatal MI by ~20%, with a manageable rise in major bleeding [HR 1.43; NNH 210] (1); the Antithrombotic Trialists’ Collaboration echoed that absolute benefits in primary prevention, though smaller than in secondary prevention, remain clinically relevant in high-risk individuals, especially those with diabetes or multiple cardiovascular risk factors. (2)
This evolution is reflected in current guidelines. The USPSTF (United States Preventive Services Task Force, 2022) recommends individualized use of aspirin in adults aged 40–59 years with a ≥10% 10-year CVD risk. The ESC (European Society of Cardiology, 2021) suggests aspirin for patients with diabetes who are at high or very high cardiovascular risk and have no contraindications. The ACC/AHA (American College of Cardiology/American Heart Association, 2019) supports aspirin use in adults aged 40–70 years who are at high ASCVD risk and have a low risk of bleeding. Together, these guidelines support a risk-based approach, where judicious aspirin use offers preventive value in selected individuals. (3)
India’s Premature CVD Burden Requires a Different Lens: Indians develop CVD nearly a decade earlier than Western populations, with the age of developing MI being 53 years in Indians compared to 58 years in Western countries. (4) Premature deaths account for 62% of CVD mortality, and one-third of acute coronary syndrome cases occur before age 50. Despite this burden, less than half of patients with hypertension and diabetes are treated, and only ~20% achieve control. (5) Conventional 10-year risk scores often underestimate risk in younger Indians, making lifetime risk tools likely more appropriate. Genetic predisposition, inflammatory states, thin-fat phenotype, and poor cardiometabolic risk factor control heighten ASCVD risk, supporting earlier, more aggressive prevention, including aspirin when indicated. (4)
Lifetime Risk Depends on Classic Modifiable Factors: A pooled analysis by the Global Cardiovascular Risk Consortium (2025) highlighted the long-term impact of five key risk factors—cardio-metabolic (hypertension, diabetes, dyslipidemia), partially modifiable (smoking), and metabolic lifestyle-related (abnormal BMI)—which together account for ~50% of global CVD burden. At age 50, individuals with all five had a lifetime CVD risk of 38% in men and 24% in women, while those without gained 10–13 additional CVD-free years. Midlife modification of blood pressure and smoking provided the greatest gains in both CVD-free and overall survival, indicating the importance of early, integrated risk factor control for primary prevention. (6) In India, control of cardio-metabolic risk is poor, with only ~7% of T2D patients meeting targets for glucose, BP, and lipids, (7) and over 50% of newly diagnosed cases are overweight or obese, highlighting the need for aggressive CVD prevention. (8)
Individualized Use: CV Risk, Age, and Bleeding Must Guide: In primary prevention, the net clinical benefit of aspirin lies in carefully balancing ischemic versus bleeding risk. Risk scores often overlook enhancers such as kidney disease, family history, elevated Lp(a), or low socioeconomic status. (3) In individuals with elevated Lp(a ≥50 mg/dL), aspirin was linked to a 52% lower risk of ASCVD mortality (HR 0.48), supporting a precision-guided approach. For high-risk patients with low bleeding risk, accurate risk stratification is key to identifying when aspirin adds true preventive value with minimal harm. Clinical tools such as the Aspirin-Guide app support personalised decision-making for initiating aspirin for CV event prevention. (9)
Case Profile: High-Risk, Low-Bleed– A Candidate for Aspirin: A 55-year-old hypertensive, sedentary male with a family history of premature CHD. BMI: 26 kg/m²; systolic BP: 150 mmHg; total cholesterol: 220 mg/dL; HDL: 40 mg/dL. He is a non-smoker, non-diabetic, with no history of GI bleeding, peptic ulcer disease, or NSAID/steroid use.
His profile includes cardio-metabolic risk factors (hypertension, elevated LDL-C), a non-modifiable risk (family history of ASCVD), and a metabolic lifestyle-linked factor (BMI). He qualifies as high CV risk with low bleeding risk, where aspirin offers likely net benefit, per DCRM 2.0 (Diabetes, Cardiorenal, and Metabolic Diseases) 2024 guidelines recommending low-dose aspirin (75–100 mg/day) in such patients with ≥2 major risk factors.
Final Message: Low-dose aspirin for primary prevention is appropriate in individuals with elevated ASCVD risk and low bleeding risk. Current guidelines and risk assessment tools support a selective, individualised approach. When initiated in the right patient profile, aspirin can help reduce the incidence of primary cardiovascular events.
References:
1. Zheng, Sean L, and Alistair J Roddick. “Association of Aspirin Use for Primary Prevention With Cardiovascular Events and Bleeding Events: A Systematic Review and Meta-analysis.” JAMA vol. 321,3 (2019): 277-287. doi:10.1001/jama.2018.20578
2. Antithrombotic Trialists’ (ATT) Collaboration et al. “Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials.” Lancet (London, England) vol. 373,9678 (2009): 1849-60. doi:10.1016/S0140-6736(09)60503-1
3. Della Bona, Roberta et al. “Aspirin in Primary Prevention: Looking for Those Who Enjoy It.” Journal of clinical medicine vol. 13,14 4148. 16 Jul. 2024, doi:10.3390/jcm13144148
4. Puri, Raman et al. “Lipid Association of India 2023 update on cardiovascular risk assessment and lipid management in Indian patients: Consensus statement IV.” Journal of clinical lipidology vol. 18,3 (2024): e351-e373. doi:10.1016/j.jacl.2024.01.006
5. Kalra, Ankur et al. “The burgeoning cardiovascular disease epidemic in Indians – perspectives on contextual factors and potential solutions.” The Lancet regional health. Southeast Asia vol. 12 100156. 10 Feb. 2023, doi:10.1016/j.lansea.2023.100156
6. Global Cardiovascular Risk Consortium et al. “Global Effect of Cardiovascular Risk Factors on Lifetime Estimates.” The New England journal of medicine, 10.1056/NEJMoa2415879. 30 Mar. 2025, doi:10.1056/NEJMoa2415879
7. Anjana, Ranjit Mohan et al. “Metabolic non-communicable disease health report of India: the ICMR-INDIAB national cross-sectional study (ICMR-INDIAB-17).” The lancet. Diabetes & endocrinology vol. 11,7 (2023): 474-489. doi:10.1016/S2213-8587(23)00119-5
8. Dalal, N., Patel, D., Chaturvedi, A., & Shah, A. (2022). Real-world observational study to capture demographic details of newly diagnosed type 2 diabetes mellitus. International Journal of Research in Medical Sciences, 10(10), 2251–2256. https://doi.org/10.18203/2320-6012.ijrms20222375
9. Razavi, Alexander C et al. “Aspirin use for primary prevention among US adults with and without elevated Lipoprotein(a).” American journal of preventive cardiology vol. 18 100674. 27 Apr. 2024, doi:10.1016/j.ajpc.2024.100674
10. Handelsman, Yehuda et al. “DCRM 2.0: Multispecialty practice recommendations for the management of diabetes, cardiorenal, and metabolic diseases.” Metabolism: clinical and experimental vol. 159 (2024): 155931. doi:10.1016/j.metabol.2024.155931
Powered by WPeMatico
Kolkata: In a move to address rising complaints against private hospitals, the West Bengal Clinical Establishment Regulatory Commission (WBCERC) is set to implement new
regulations prohibiting the practice of withholding dead bodies until the patients’ families clear dues.
Speaking at the eighth state
conference of the Progressive Nursing Home Association held in Kolkata, WBCERC
commissioner and retired Calcutta High Court judge Justice Asim Banerjee
emphasized that private medical establishments must not delay the release of a
deceased person’s body over pending bills. He stressed that bodies should be
returned to the next of kin within a fixed timeframe following the patient’s
death.
According to The Statesman, he stated, “We are
planning to frame rules on how outstanding hospital bills are paid by relatives
of patients after the deaths of the latter at private hospitals and nursing homes
during treatments. We will also take clearance from the state government before the formation of the rules. But the release of a dead body should not be withheld by
private healthcare establishments by any means, not even by showing reasons for
non-payment of bills. At the same time, hospitals should not also withhold
indoor patients discharged by concerned doctors.”
Justice Banerjee
highlighted the need for 24/7 availability of trained nursing staff and
resident medical officers (RMOs) at all private hospitals and nursing homes,
underlining the importance of maintaining professional healthcare standards. He
also expressed concern over the alleged misuse of the state-run Swasthya Sathi
health insurance scheme by some private healthcare providers, urging them to
refrain from exploiting public funds for financial gain.
Launched in 2017, West
Bengal’s Clinical Establishment Act is unique to the state, with no equivalent
legislation found elsewhere in the country. The WBCERC, functioning as an
autonomous body under this Act, currently regulates between 5,000 and 7,000 private
hospitals and nursing homes across West Bengal. WBCERC is the apex body
overseeing treatment infrastructure in private hospitals and nursing homes
across the state, reports the Daily.
To prevent overcharging
by private hospitals, WBCERC had requested data from hospitals for the past
three years to determine the number of Swasthya Sathi patients treated at
private healthcare facilities. The direction came following complaints from
patients about inflated bills for surgeries and other amenities in private
hospitals.
Powered by WPeMatico
According to a new study published in JAMA ,calprotectin may serve as a mechanistically informed biomarker for atherosclerotic cardiovascular disease (ASCVD), independent of established risk factors and biomarkers. However its clinical utility requires further investigation. This study was conducted by Yu Zuo and fellow researchers.
Calprotectin, a marker of neutrophil activation, has been recognized to be an important player in inflammation, which is at the core of atherosclerotic cardiovascular disease (ASCVD) pathogenesis. Its understanding as a potential predictor of ASCVD may lead to enhanced early identification of individuals at high risk.
The research comprised 2,412 Dallas Heart Study participants, who were a multiethnic population-based cohort. Plasma samples taken at phase 2 of the study were used to measure calprotectin levels. Participants were followed up for a median of 8 years to assess the incidence of ASCVD events such as nonfatal myocardial infarction, nonfatal stroke, coronary revascularization, and cardiovascular mortality.
The association between calprotectin levels and ASCVD events was examined by Cox proportional hazards models, which controlled for recognized cardiovascular risk factors, such as high-sensitivity C-reactive protein (hs-CRP), N-terminal pro–brain natriuretic peptide (NT-proBNP), and high-sensitivity cardiac troponin T (hs-cTnT). The research also determined the effect of calprotectin on coronary artery calcium scores, an indicator of atherosclerosis. Additionally, experiments in vitro assessed the role of calprotectin in the mechanisms of endothelial dysfunction in order to elucidate the possible ways of progression in ASCVD.
Key Findings
Association with ASCVD Events:
A multivariable adjusted model demonstrated an association of a higher risk for ASCVD events over 8 years in conjunction with increased calprotectin levels.
A significant association of calprotectin increase was noted between each log value and 98% increased ASCVD events HR: 1.98; 95% CI, 1.54-2.53.
Even after adjustment for the traditional risk factors, the association remained significant, with an HR of 1.61 (95% CI, 1.22-2.13), and even after further adjustment for hs-CRP, NT-proBNP, and hs-cTnT, it remained significant with an HR of 1.43 (95% CI, 1.04-1.96).
Demographic Associations:
Higher calprotectin levels were more common among older individuals, males, individuals of Black race, and those with hypertension, diabetes, and smoking history.
Volunteers with increased calprotectin also had increased hemoglobin A1c, extremely low-density lipoprotein cholesterol, and triglycerides but decreased high-density lipoprotein cholesterol and cholesterol efflux capacity.
Effect on Coronary Artery Calcium:
Increased calprotectin levels correlated with substantially greater coronary artery calcium scores (P <.001), suggesting an association between calprotectin and severity of atherosclerosis.
Mechanistic Insights:
In vitro experiments showed that calprotectin damages coronary endothelial integrity, decreases nitric oxide production, and enhances endothelial-to-mesenchymal transition. These actions indicate a direct role of calprotectin in ASCVD development.
The study authors concluded that elevated calprotectin levels were independently linked to a higher risk of ASCVD in a multiethnic population, affirming its utility as a potential biomarker for cardiovascular risk.
Reference:
Powered by WPeMatico

Jaipur: The Narcotics Control Bureau (NCB) has arrested an MBBS doctor along with eight other individuals for their alleged involvement in a sophisticated smuggling network that spanned across five states, including Rajasthan, Madhya Pradesh, Tamil Nadu, Karnataka, and Maharashtra.
In a recent post on X, autopsy surgeon Yamraj highlighted a disturbing trend-highly educated individuals, including an engineer, an MBA graduate, and an MBBS doctor—were allegedly involved in an international drug trafficking network. They are accused of facilitating the trafficking and distribution of narcotics, including cocaine, MDMA, methamphetamine, methaqualone, and ecstasy.
According to the NCB, drugs shipped from France and Germany were entering India through international postal services, with several parcels routed via Jaipur’s Foreign Post Office, according to the Narcotics Control Bureau (NCB). In a coordinated operation, the Rajasthan unit of the NCB arrested nine smugglers across five states.
Although the identities of the accused have not been disclosed, NCB officials revealed that Jaipur is increasingly being used as a ‘drug distribution hub.’ The smuggled cocaine is reportedly transported from Jaipur to Mumbai through Udaipur, and investigators have also indicated possible links between the network and individuals in Bollywood.
Also Read: Lucknow: Two arrested for shipment of banned medicines to US
During the operation, 324.65 grams of cocaine were recovered along with large quantities of other synthetic narcotics. Two key parcels—containing 111 grams of ecstasy tablets, 101 grams of methaqualone, and 150 grams of MDMA—had arrived in Jaipur, confirming the city’s emerging status as a distribution hub for international narcotics.
Officials revealed that the trafficking ring operated via the dark net, utilizing cryptocurrency and encrypted communications. Jaipur, with its logistical connectivity and relatively lower law enforcement pressure, was being used as a central point to receive and redirect shipments to major cities, including Mumbai.
Also Read: BHMS doctor held with 577 grams Opium in Bhopal
Powered by WPeMatico
Patients suffering from long COVID may exhibit persistent inflammation in the heart and lungs for up to a year following SARS-CoV-2 infection-even when standard medical tests return normal results-potentially placing them at elevated risk for future cardiac and pulmonary conditions. These findings come from a new study conducted by researchers at the Icahn School of Medicine at Mount Sinai and published in the Journal of Nuclear Medicine.
The study, the largest of its kind using advanced PET/MRI imaging, discovered significant abnormalities in cardiovascular and pulmonary tissues, as well as altered levels of circulating immune-regulating proteins, in long COVID patients. These abnormalities could serve as early warning signs of diseases such as heart failure, valvular heart disease, and pulmonary hypertension.
“Long COVID has emerged as a major public health challenge, and the long-term sequelae remain largely undefined,” says corresponding author Maria G. Trivieri, MD, PhD, Associate Professor of Medicine (Cardiology), and Diagnostic, Molecular and Interventional Radiology at the Icahn School of Medicine. “This study brings us closer to understanding how SARS-CoV-2 affects the heart and lungs over time. We believe long COVID results in an inflammatory response that may predispose patients to premature coronary artery disease, pulmonary hypertension, and valvular damage such as stenosis or regurgitation.”
“Since 2020, we have been publishing work showing that even mild or asymptomatic COVID infections can have serious cardiovascular consequences, even in previously fit and healthy individuals,” says David Putrino, PhD, the Nash Family Director of Mount Sinai’s Cohen Center for Recovery from Complex Chronic Illness. “This paper provides more data to highlight that SARS-CoV-2 is a virus that profoundly affects vascular health and that every new infection can do damage. Infection prevention is crucial.”
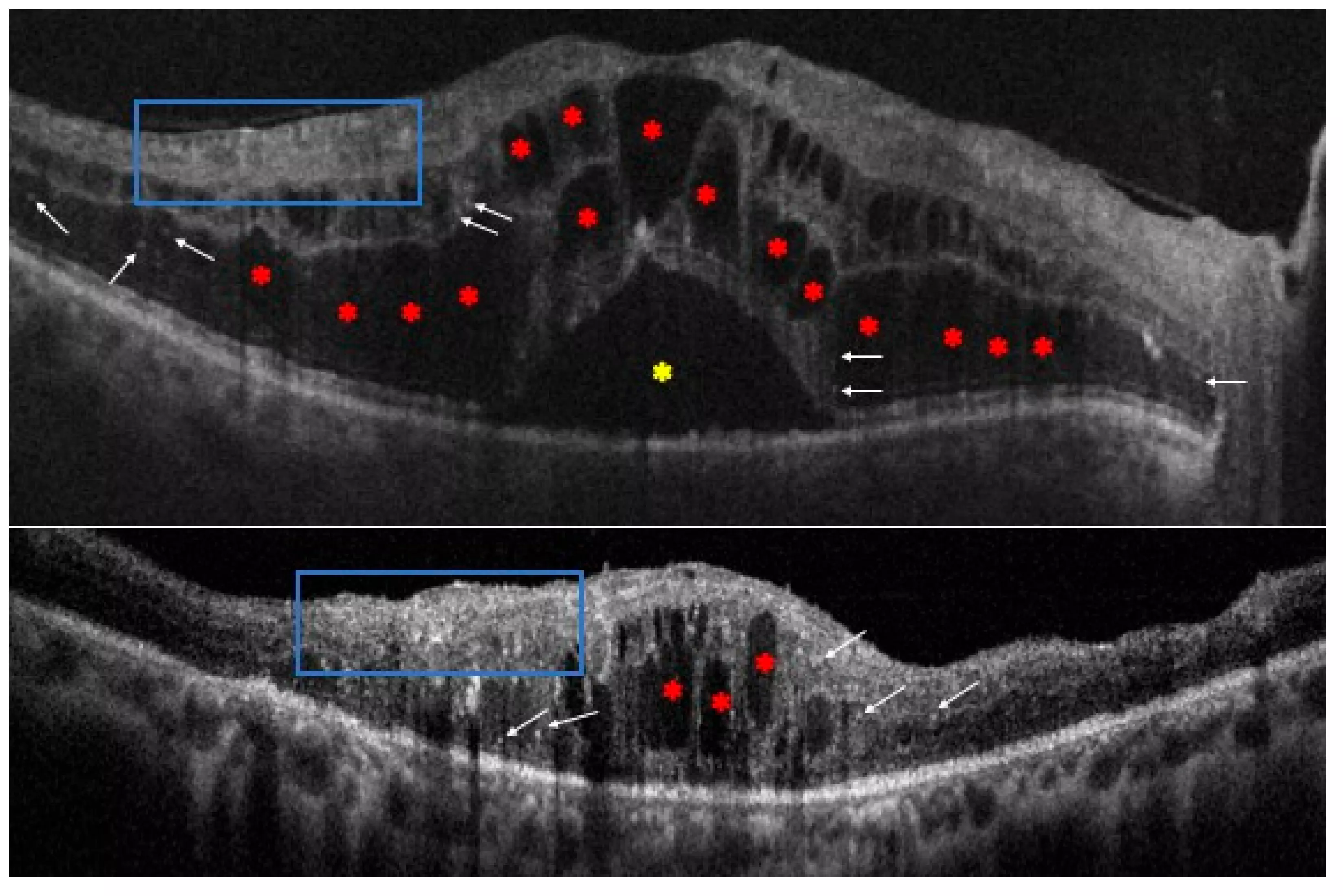
Researchers studied 100 adult Mount Sinai patients who had a confirmed COVID-19 infection between December 2020 and July 2021 and were experiencing persistent cardiopulmonary symptoms. Most of these patients had no previous diagnosis of cardiovascular disease. About 300 days after their initial infection, 91 participants underwent hybrid 18F-fluorodeoxyglucose positron emission tomography combined with magnetic resonance imaging (PET/MRI), an advanced imaging method that simultaneously detects structural and metabolic abnormalities. Among those scanned, 52 patients—representing 57 percent—demonstrated evidence of inflammation affecting the heart muscle, pericardium (the thin sac that surrounds the heart), heart valves, particularly the mitral valve, and the aortic and pulmonary blood vessels. In several cases, more than one of these regions was affected.
The PET/MRI scans revealed myocardial (heart muscle) abnormalities in 22 participants, characterized by scarring and thickening of the tissue, similar to findings of myocarditis or cardiomyopathy. Pericardial involvement was seen in 20 patients, indicating either inflammation or effusion, a buildup of fluid. Inflammation near the mitral valve was identified in 10 participants, and vascular inflammation involving the aorta or pulmonary arteries was observed in 28 participants. All abnormalities were associated with persistent symptoms such as chest pain, fatigue, and shortness of breath.
In parallel, researchers performed plasma protein analysis, which showed abnormal patterns in key biomarkers that regulate inflammation and immune signaling. These findings correlated with the imaging abnormalities, providing molecular-level confirmation of persistent inflammation.
To further validate the results, a control group of nine individuals with confirmed prior COVID-19 infection but no lingering cardiopulmonary symptoms was studied between March and October 2023. These controls underwent the same imaging and blood testing and did not exhibit the inflammatory changes observed in the symptomatic long COVID cohort.
“We found a range of cardiopulmonary inflammatory patterns, backed by abnormal protein profiles,” Dr. Trivieri says. “These insights could have far-reaching implications for diagnosis and surveillance. If patients experience lingering symptoms such as shortness of breath, they should consult a physician for further evaluation. Our results should also raise awareness among clinicians to consider a patient’s COVID history and evaluate persistent symptoms more thoroughly.”
Zahi Fayad, PhD, senior author of the study and Director of the Biomedical Engineering and Imaging Institute at the Icahn School of Medicine at Mount Sinai, emphasized the broader impact of these findings. “This study highlights the unique power of hybrid PET/MRI imaging to uncover hidden disease processes in long COVID patients,” Dr. Fayad says. “These findings should change how we approach care and surveillance-not only recognizing SARS-CoV-2 as a potential long-term cardiovascular risk factor, but also integrating molecular imaging into post-COVID evaluation protocols. We now have objective evidence that can guide earlier detection and potentially prevent future cardiopulmonary events.”
The Mount Sinai team continues to follow this patient cohort to assess long-term outcomes and is exploring whether these imaging and biomarker patterns can help predict who is most at risk for developing chronic cardiovascular or pulmonary disease after COVID-19.
Reference:
Maria Giovanna Trivieri et al, Prevalence of Persistent Cardiovascular and Pulmonary Abnormalities on PET/MRI and DECT Imaging in Long COVID Patients, Journal of Nuclear Medicine (2025). DOI: 10.2967/jnumed.124.268980.
Powered by WPeMatico
Researchers have discovered in an ongoing phase IIb trial that a single intravitreal injection of UBX1325 (foselutoclax), a novel senolytic agent, demonstrated a tolerable safety profile and showed signs of potential efficacy in patients with diabetic macular edema (DME) who had inadequate response to anti-VEGF treatments. The results of the ongoing phase IIb trial comparing UBX1325 to standard anti-VEGF therapy are anticipated later this year.
They tested the ability of a single intravitreal injection of foselutoclax (hereafter UBX1325), a novel senolytic small molecule inhibitor of antiapoptotic protein B-cell lymphoma–extra large, to mitigate the impact of diabetic macular edema.Patients with diabetic macular edema with prior suboptimal response to anti–vascular endothelial growth factor treatment were randomly assigned (1:1) to either a single intravitreal injection of 10 μg of UBX1325 or sham and were followed for up to 48 weeks. The primary trial objective was to evaluate the safety and side-effect profile of UBX1325 as assessed by ocular and systemic treatment-emergent adverse events (TEAEs). Our secondary objective was to probe efficacy, defined as mean changes from baseline for UBX1325 versus sham in best corrected visual acuity measured in Early Treatment of Diabetic Retinopathy Study (ETDRS) letters (range, 0–100 letters, higher scores indicate better vision) and retinal structure. Results: Between June 2021 and April 2022, 65 participants (32.3% women) were randomly assigned to either UBX1325 (n=32) or sham (n=33). There were four TEAEs of Grade 3 or greater in the sham group, of which three were considered serious, while there were five in the UBX1325 group of Grade 3 or greater and considered serious. There were no apparent between-group differences with respect to vital signs, electrocardiograms, or routine blood chemistries. For the secondary outcome of efficacy, the difference between UBX1325 and sham in mean change to week 48 in best corrected visual acuity was 5.6 more ETDRS letters (95% confidence interval, −1.5 to 12.7). In this sham-controlled trial there were no TEAEs that led to discontinuation of treatment with UBX1325 compared with sham. There were trends suggestive of potential efficacy; larger trials are needed to further evaluate these findings.
Reference:
Klier, S., Dananberg, J., Masaki, L., Bhisitkul, R. B., Khanani, A. M., Maturi, R., Salehi-Had, H., Mallinckrodt, C. H., Rathmell, J. M., Ghosh, A., & Sapieha, P. (2025). Safety and efficacy of senolytic UBX1325 in diabetic macular edema. NEJM Evidence, https://doi.org/10.1056/EVIDoa2400009
Keywords:
Klier, S., Dananberg, J., Masaki, L., Bhisitkul, R. B., Khanani, A. M., Maturi, R., Salehi-Had, H., Mallinckrodt, C. H., Rathmell, J. M., Ghosh, A., & Sapieha, P, diabetic, macular, edema. NEJM Evidence
Powered by WPeMatico

A single blood test, designed to pick up chemical signals indicative of the presence of many different types of cancer, could potentially thwart progression to advanced disease while the malignancy is still at an early stage and amenable to treatment in up to half of cases, suggests a modelling study published in the open access journal BMJ Open.
Incorporating the test, formally known as a multi-cancer early detection test, or MCED for short, either yearly or biennially, could therefore improve outcomes for patients by intercepting disease progression, suggest the researchers.
Currently, only a few cancers can be reliably screened for-those of the breast, bowel, cervix (neck of the womb), and lung for those at high risk. While effective at lowering death rates from these diseases, these screens can also result in false positive results and overdiagnosis, say the researchers.
The optimal interval at which screening will pick up the most cancers at an early stage (I and II) while at the same time avoiding unnecessary testing and treatment still isn’t clear.
To inform future clinical trials, the researchers drew on a previously published disease progression model for many different cancers. They used this to predict the impact of regular screening with an MCED test on the time of cancer diagnosis and patient death for different screening schedules among 50-79 year olds in receipt of usual care.
The screening schedules modelled ranged from 6 months to 3 years, but with an emphasis on annual and biennial screening for two sets of cancer growth scenarios. These were ‘fast’, where tumours remain at stage I for between 2 and 4 years before progressing; and ‘fast aggressive’ where tumours remain at stage 1 for between 1 and 2 years, with decreasing periods of time for progression to successive stages.
Cancer types included were those of the anus; bladder; breast; cervix; bowel/rectum; food pipe (oesophagus); gallbladder; head and neck; kidney; liver/ bile-duct; lung; ovary; pancreas; prostate; sarcoma (soft tissues/bone); stomach; thyroid; urothelial tract, and uterus, as well as leukaemia, lymphoma, melanoma, blood cancers (myeloid neoplasm, immune cell cancers (plasma cell neoplasm).
The researchers drew on MCED test characteristics from a recently published report and patient outcomes from population cancer data from the US Surveillance, Epidemiology and End Results (SEER) programme.
Their analysis showed that all MCED screening intervals had more favourable early-stage diagnostic rates than usual care alone. There was a larger impact on stage shift for tumours with ‘fast’ growth than for tumours with ‘fast aggressive’ growth.
But annual MCED screening under the fast tumour growth scenario was associated with a higher number of diagnoses: 370 more cancer signals were detected per year per 100,000 people screened, with 49% fewer late-stage diagnoses, and 21% fewer deaths within 5 years than usual care.
While biennial MCED screening was able to shift the stage at diagnosis and avert deaths, it was not as effective as annual screening: 292 more cancer signals were detected/year/100,000 people screened; 39% fewer late-stage diagnoses; and 17% fewer deaths within 5 years than usual care.
Annual MCED screening prevented more deaths within 5 years than biennial screening for the fast tumour growth scenario. But biennial screening had a higher positive predictive value: 54% compared with 43%. In other words ,it picked up more cancers for each completed test.
And it was more efficient at preventing more deaths within 5 years per 100,000 tests-132 compared with 84, although it prevented fewer deaths per year, so was less effective.
Given that 392 people are diagnosed each year with an aggressive cancer that would kill them within 5 years, earlier diagnosis through biennial MCED screening could have averted 54 (14%) of these deaths. But annual MCED screening could have avoided 84 (21%) fewer deaths, say the researchers.
“Based on the performance characteristics from a case control study, both annual and biennial screening with an MCED test have the potential to intercept 31–49% of cancers at stage I-II that would otherwise present at stage III-IV,” they estimate.
“Of these, approximately equal numbers would be detected at stage I and at stage II: 14% stage I and 16% stage II to 23% stage I and 26% stage II.”
The researchers acknowledge that their estimates assume 100% compliance with the recommended screening schedule and 100% accuracy of confirmatory follow up tests, and so represent the upper bounds of potential benefits of MCED cancer screening.
It is also assumed that a reduction in the number of late-stage cancer diagnoses would automatically reduce death rates from the disease. And they point out: “The optimal choice of screening interval will depend on assessments of real-world cancer survival and the costs of confirmatory testing after MCED screening.
“However, both annual and biennial MCED screening intervals have the potential to avert deaths associated with late-stage cancers when used in addition to current guideline-based cancer screening.”
Reference:
https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2024-086648
Powered by WPeMatico

Presented at ESTRO 2025, which gathered a record attendance of 7,908 participants this week in Vienna, Austria, a 10-year study, involving over 4,000 UK patients, confirms that a one-week course of post-surgery radiotherapy is just as safe and effective as the traditional three-week regimen for early-stage breast cancer patients. These long-term results from the FAST-Forward trial, could further reduce the burden on breast cancer patients worldwide, and expand access to life-saving radiotherapy.
The phase III randomised trial, which was sponsored by The Institute of Cancer Research, London and funded by a grant from UK National Institute of Health Research (NIHR), followed up patients for ten years and showed that a shorter, five-day radiotherapy schedule provides a similar level of cancer control as the standard 3-week treatment, without additional long-term side effects. This builds on previous five-year results that have already led to a shift in clinical practice.
Breast cancer is one of the most common cancers globally, and radiotherapy plays a critical role in reducing the risk of recurrence after surgery. A shorter treatment course offers major benefits:
• More convenient for patients, reducing hospital visits
• Reduces pressure on radiotherapy services, making treatment more accessible
• Same safety and effectiveness as the longer regimen
“This 10-year analysis provides definitive long-term evidence that one-week radiotherapy to the breast is a safe, effective, and more practical option for breast cancer patients,” said Professor Murray Brunt, lead investigator of the study.
Professor Judith Bliss, Professor of Clinical Trials at The Institute of Cancer Research, London, who co-led the trial, said:
“The FAST-Forward trial revolutionised cancer treatment by reducing the standard radiotherapy from three weeks to just one week, without compromising effectiveness.
“This approach has significantly improved patient experience and healthcare practices, both during and after the Covid-19 pandemic, by minimising hospital visits.
“The streamlined schedule has made radiotherapy more accessible to more women, particularly those who are less able to attend hospital and those from lower-income countries.”
Professor Matthias Guckenberger, President of ESTRO, Chairman of the Department of Radiation Oncology and full Professor at the University Hospital Zurich and University of Zurich, emphasised the broader significance of this research:
“Radiotherapy is a cornerstone of modern cancer treatment, and studies like FAST-Forward demonstrate how we can optimise its delivery to benefit more patients.
“By reducing treatment time without compromising effectiveness, we are not only improving patient experience but also making better use of radiotherapy resources and healthcare systems worldwide.”
“These findings reinforce the critical role of radiotherapy in the fight against cancer.”
Reference:
One-week breast cancer radiotherapy proven as safe and effective as standard three-week treatment in 4,000-patient study over 10 years, European Society for Radiotherapy and Oncology (ESTRO), Meeting: ESTRO 2025.
Powered by WPeMatico
Turkiye: New research shows that individuals with fibromyalgia syndrome (FMS) have significantly higher rates of astigmatism, dry eye disease (DED), and meibomian gland dysfunction (MGD) compared to those without the condition, highlighting the need for regular anterior eye assessments in this population.
Published in Rheumatology International, the cross-sectional study explored the potential link between FMS and ocular surface health by comparing various eye parameters between FMS patients and healthy individuals. Conducted between August and November 2024 at a tertiary care hospital, the study included a thorough evaluation of the anterior segment of the eye, focusing on central corneal thickness, visual acuity, refraction values, intraocular pressure, and signs of dry eye and meibomian gland dysfunction.
Key Findings:
The study emphasizes that although basic visual performance remains largely unaffected in fibromyalgia, the condition may increase the risk of anterior segment abnormalities. These findings point toward possible ocular involvement in fibromyalgia and suggest the condition could influence the eye’s surface environment.
Given the significant presence of dry eye and meibomian gland dysfunction in FMS patients, the researchers recommend regular eye checkups for individuals with the condition. Burhan Fatih Kocyigit from Adana City Training and Research Hospital in Adana, Türkiye, and colleagues also note the importance of further studies to explore the underlying mechanisms driving these changes. Future research should aim to understand how factors such as medication, autonomic nervous system imbalances, and associated mental health conditions, like anxiety, depression, and sleep disturbances, might contribute to the development of ocular issues in fibromyalgia.
“Ultimately, these insights could guide better screening strategies and inform more comprehensive management plans for FMS patients, extending care beyond musculoskeletal symptoms to include eye health monitoring,” they concluded.
Reference:
Emekli, D.T., Sahutoglu, E., Öztürk, G.Y. et al. Anterior segment alterations in fibromyalgia syndrome: a cross-sectional study on dry eye disease, meibomian gland dysfunction, and astigmatism. Rheumatol Int 45, 120 (2025). https://doi.org/10.1007/s00296-025-05872-w
Powered by WPeMatico
