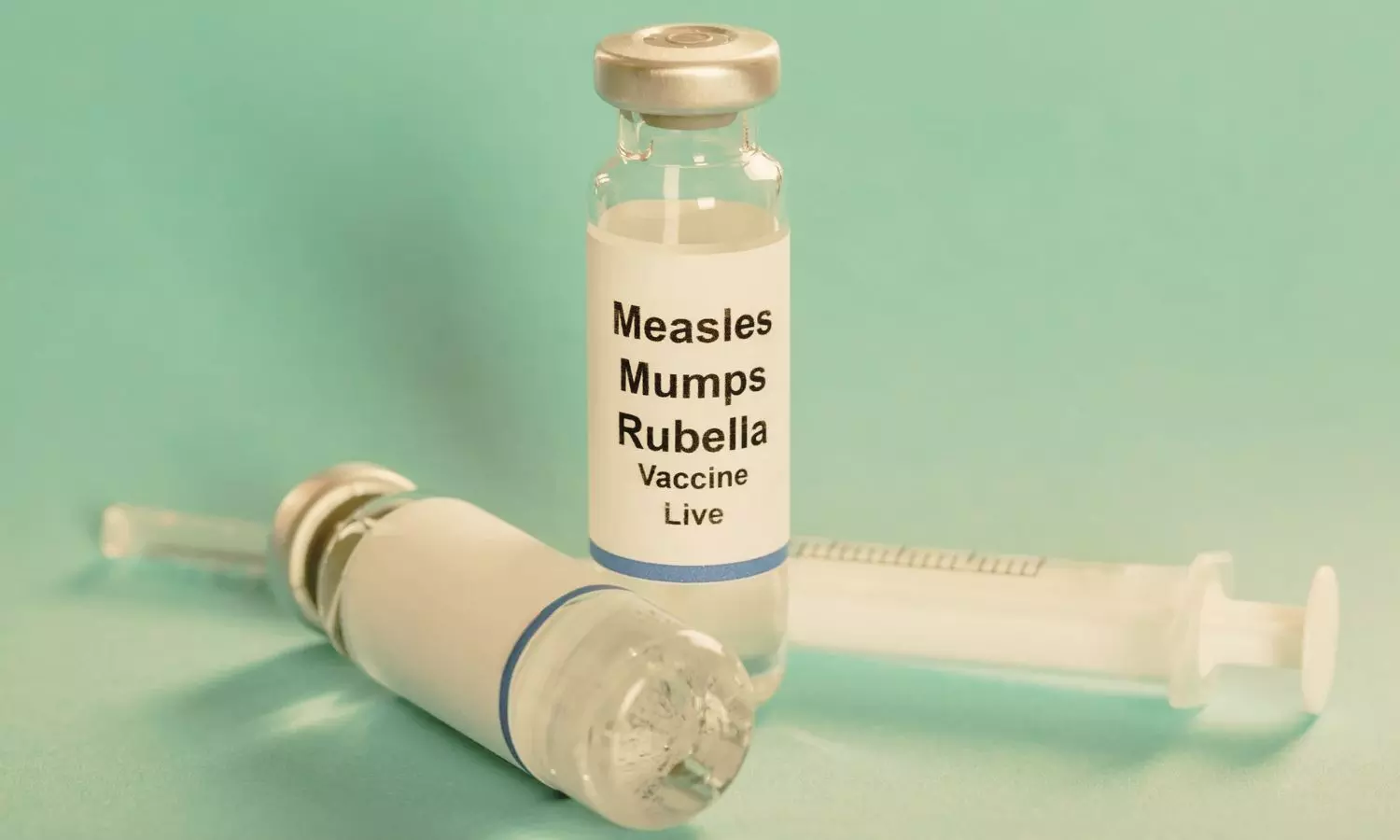
mRNA-1083 Effective and Safe for Adults Aged 50+ Against Flu and COVID-19, Phase 3 Trial Reveals

USA: A new phase 3 clinical trial has found that a single multi-component mRNA vaccine targeting both seasonal influenza and COVID-19 is not only well-tolerated but also produces immune responses on par with, or even better than, current standard vaccinations in adults aged 50 years and older.
The findings were published online in the Journal of the American Medical Association (JAMA) on May 7, 2025.
Despite strong recommendations, the uptake of seasonal influenza and COVID-19 vaccines continues to remain below optimal levels, particularly among older adults. To address this gap and simplify immunization strategies, Amanda K. Rudman Spergel, Moderna Inc, Cambridge, Massachusetts, and colleagues evaluated the immunogenicity and safety of an investigational multicomponent vaccine, mRNA-1083, designed to protect against both seasonal influenza and SARS-CoV-2.
The investigational vaccine, mRNA-1083, was evaluated in a randomized, observer-blinded study conducted at 146 sites across the United States. The trial enrolled over 8,000 participants between October and November 2023, including two distinct age groups: individuals aged 50–64 years and those aged 65 years or older. The primary aim was to determine if mRNA-1083 could generate immune responses that were at least as strong as those produced by the currently licensed influenza and COVID-19 vaccines.
Participants in the study were randomly assigned to receive either the mRNA-1083 vaccine with a placebo or a combination of licensed influenza and COVID-19 vaccines. Those aged 65 years and older received the high-dose quadrivalent inactivated influenza vaccine (HD-IIV4), while those aged 50–64 received the standard-dose version (SD-IIV4), along with an mRNA COVID-19 vaccine (mRNA-1273) in both groups.
The key findings of the study were as follows:
- mRNA-1083 generated noninferior immune responses against all influenza and SARS-CoV-2 strains compared to standard vaccines.
- In adults aged 50–64, the vaccine produced stronger antibody responses than the standard-dose influenza vaccine for all four flu strains.
- Among participants aged 65 and older, mRNA-1083 outperformed the high-dose flu vaccine for three flu strains: A/H1N1, A/H3N2, and B/Victoria.
- The vaccine also showed a superior immune response against SARS-CoV-2 in both age groups.
- Mild to moderate side effects, such as pain at the injection site, fatigue, and headache, were more frequently reported with mRNA-1083 but resolved quickly.
- No serious safety concerns were observed during the trial.
The authors concluded, “The phase 3 trial demonstrated that a single dose of the multicomponent mRNA-1083 vaccine is at least as immunogenic as the currently recommended influenza and COVID-19 vaccines in adults aged 50 and above.”
They stressed that the vaccine not only met noninferiority criteria but also elicited stronger immune responses against multiple influenza strains and SARS-CoV-2, with a favorable safety and tolerability profile, supporting its potential as a convenient and effective dual-protection option for older adults.
Reference:
Rudman Spergel AK, Wu I, Deng W, et al. Immunogenicity and Safety of Influenza and COVID-19 Multicomponent Vaccine in Adults ≥50 Years: A Randomized Clinical Trial. JAMA. Published online May 07, 2025. doi:10.1001/jama.2025.5646
Powered by WPeMatico