Breastfeeding, even partially alongside formula feeding, changes the chemical makeup-or metabolome-of an infant’s gut in ways that positively influence brain development and may boost test scores years later, suggests new CU Boulder research.
“For those who struggle with exclusively breastfeeding, this study suggests your baby can still get significant benefits if you breastfeed as much as you can,” said senior author Tanya Alderete, an assistant professor of integrative physiology at CU Boulder.
The study, published Dec. 13 in the journal npj Metabolic Health and Disease, also identifies specific metabolites that manufacturers may want to consider adding to infant formula to optimize healthy brain development and concerning compounds they should try to leave out.
“Our research suggests that even at low levels, some contaminants found in formula may have negative neurodevelopmental effects downstream,” said first author Bridget Chalifour, a postdoctoral researcher in Alderete’s lab.
A health report card for the gut
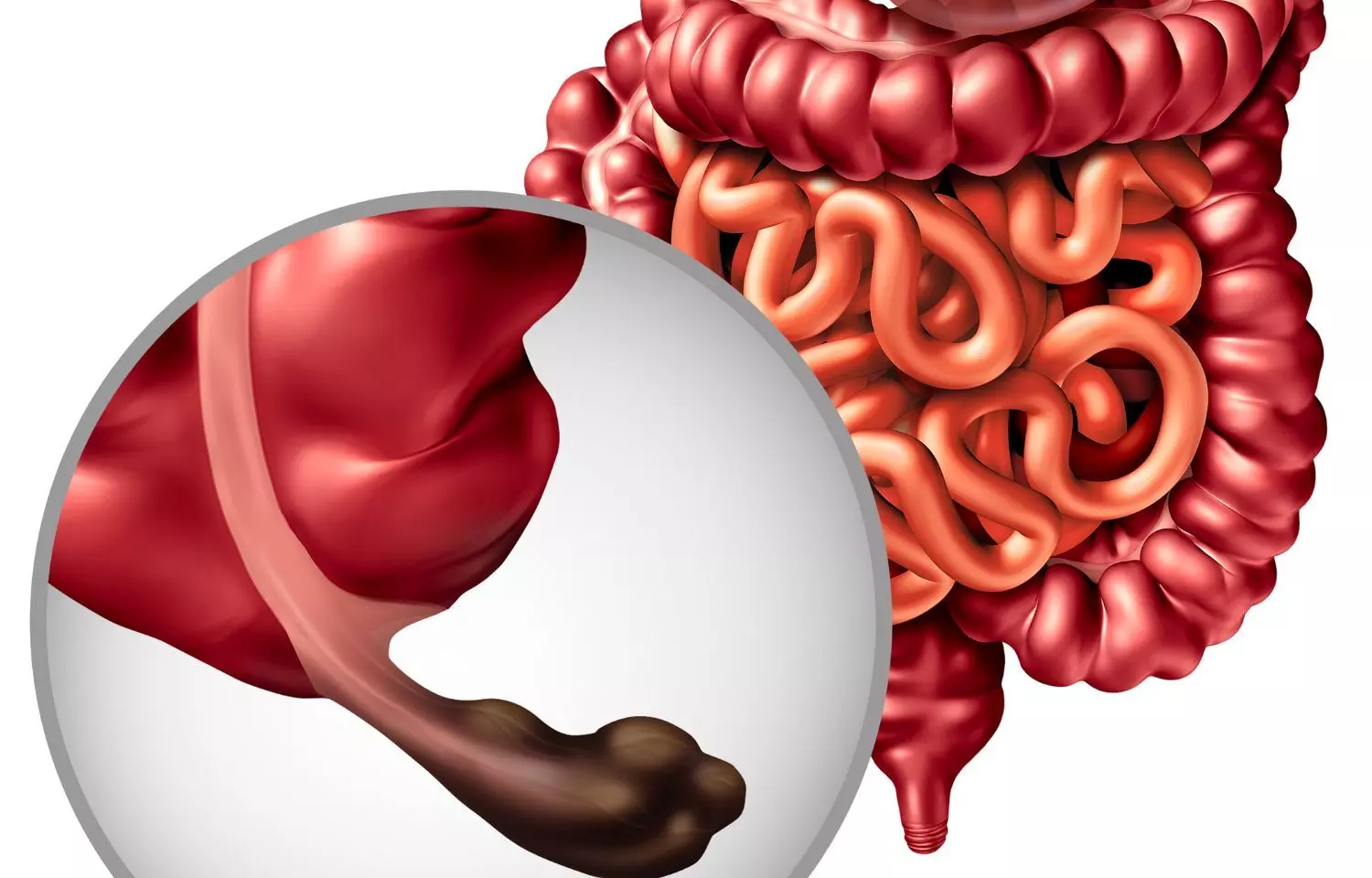
For the study, the research team examined what is known as the “fecal metabolome”-the diverse collection of metabolites found in the gut and shed in poop. Metabolites are small molecules that are churned out by gut bacteria as a byproduct of metabolizing food and make their way into the bloodstream, impacting the brain and other organs.
Breastmilk, formula and solid food also contain metabolites.
While scientists have long studied our resident bacteria, or microbiome, to better understand human health, the emerging field of “metabolomics” goes a step further.
“Looking at the gut microbiome tells us which bacteria are there, while looking at the fecal metabolome can help tell us what they are doing,” said Chalifour. “It’s like a health report card for the gut.”
The team collected fecal samples from 112 infants at 1- and 6-months-old and worked with Donghai Liang, assistant professor of environmental health at Emory University in Atlanta, and other colleagues to chemically analyze which metabolites were present. They grouped infants based on how much they were breastfed vs. formula fed. At age 2, the children took cognitive, motor and language tests.
The study found that the samples from infants in different feeding groups contained significantly different levels of metabolites.
For instance, at 1 month old, 17 metabolites were more abundant the more a baby was breastfed, and 40 were more abundant the more a baby was formula fed.
When looking more closely at specific metabolites, the researchers identified 14 that were also associated with differences in test scores at age 2.
With only one notable exception, caffeine, the more metabolites associated with breast milk a baby had in their stool, the better they did on cognitive tests as toddlers (more on caffeine later.)
The more metabolites associated with formula feeding they had, the worst they did.
“The consistency of these results is striking and supports the benefits of breastfeeding as much as possible in early life,” said Alderete.
Some metabolites associated with formula concerning
One particularly beneficial metabolite was cholesterol: At both 1 and 6 months old, the more a baby was breastfed the more cholesterol they had in their stool. And the more cholesterol babies had in their stool, the better they did on cognitive tests. This makes sense, as the fatty acid is critical for forming healthy circuits between brain cells. As the authors note, 80% to 90% of the brain’s volume grows in the first two years of life.
In contrast, the more a baby was formula fed, the higher their levels of a metabolite called cadaverine, a known contaminant formed via fermentation.
In the study, the more a child was formula fed, the higher their levels of cadaverine and the lower their test scores at age 2. While the compound is considered a toxin at higher levels, the Food and Drug Administration permits low levels in infant formula.
“It may be that formula manufacturers should be more vigilant in getting levels of this compound down to zero,” said Chalifour.
Interestingly, babies who were breastfed had higher levels of caffeine in their stool-perhaps because moms may have been breastfeeding over a cup of coffee.
Not surprisingly, higher levels of caffeine, a stimulant, were associated with poorer cognitive scores. Prenatal caffeine exposure has previously been associated with lower neurodevelopmental scores, and experts recommend no more than 12 ounces, or a cup and a half, of coffee per day for pregnant women.
Not all or nothing
The World Health Organization recommends that infants be exclusively breastfed for the first six months of life, but in the United States, only 63% of infants are exclusively breastfed immediately following birth. By six months, only a quarter of U.S. babies are exclusively breastfed.
Alderete acknowledges that for some parents, breastfeeding isn’t possible. She hopes her research can ultimately help manufacturers improve formula to make it as close to breastmilk as it can be. And she stresses that just because a child was not breastfed does not mean they’ll have neurodevelopmental deficits. Early feeding patterns are just one of many factors that contribute to how a brain develops.
Her takeaway to new parents having trouble breastfeeding exclusively: Don’t give up. It doesn’t have to be all or nothing.
“Just increasing the proportion of breastmilk relative to formula may have a positive impact on your developing child,” she said.
Reference:
Bridget Chalifour, Elizabeth A. Holzhausen, Joseph J. Lim, Emily N. Yeo, Natalie Shen, Dean P. Jones, Bradley S. Peterson, Michael I. Goran, Donghai Liang, Tanya L. Alderete. The potential role of early life feeding patterns in shaping the infant fecal metabolome: implications for neurodevelopmental outcomes. npj Metabolic Health and Disease, 2023; 1 (1) DOI: 10.1038/s44324-023-00001-2.