CKD predicts incomplete revascularization and subsequent MACE in CCS patients

Egypt: Chronic kidney disease predicts partial revascularization and subsequent major adverse cardiovascular events (MACE) in patients with chronic coronary syndrome (CCS), a recent study published in the Indian Heart Journal has revealed.
The study showed that among patients with CCS, chronic kidney disease (CKD) is associated with a higher syntax score (SS) and incomplete revascularization prevalence. Additionally, an association was observed between incomplete revascularization and an increased risk of MACE.
Atherosclerotic plaque formation in the epicardial coronary arteries is the pathological hallmark of coronary artery disease (CAD). Several clinical manifestations can be classified as either chronic coronary syndrome or acute coronary syndrome due to the dynamic nature of the CAD process.
Chronic kidney disease and coronary artery disease constitute a high-risk combination. Despite its high prevalence, few studies have been conducted on CAD, specifically in CKD patients, frequently excluded from most trials. Therefore, there is a lack of evidence for CAD management, which might lead to the inadequate treatment of CKD patients.
To fill this knowledge gap, Shereen Ibrahim Farag, Benha University, Faculty of Medicine, Cardiology Department, Benha, Egypt, and colleagues aimed to determine the impact of CKD on the completeness of revascularization and MACE in patients with chronic coronary syndrome.
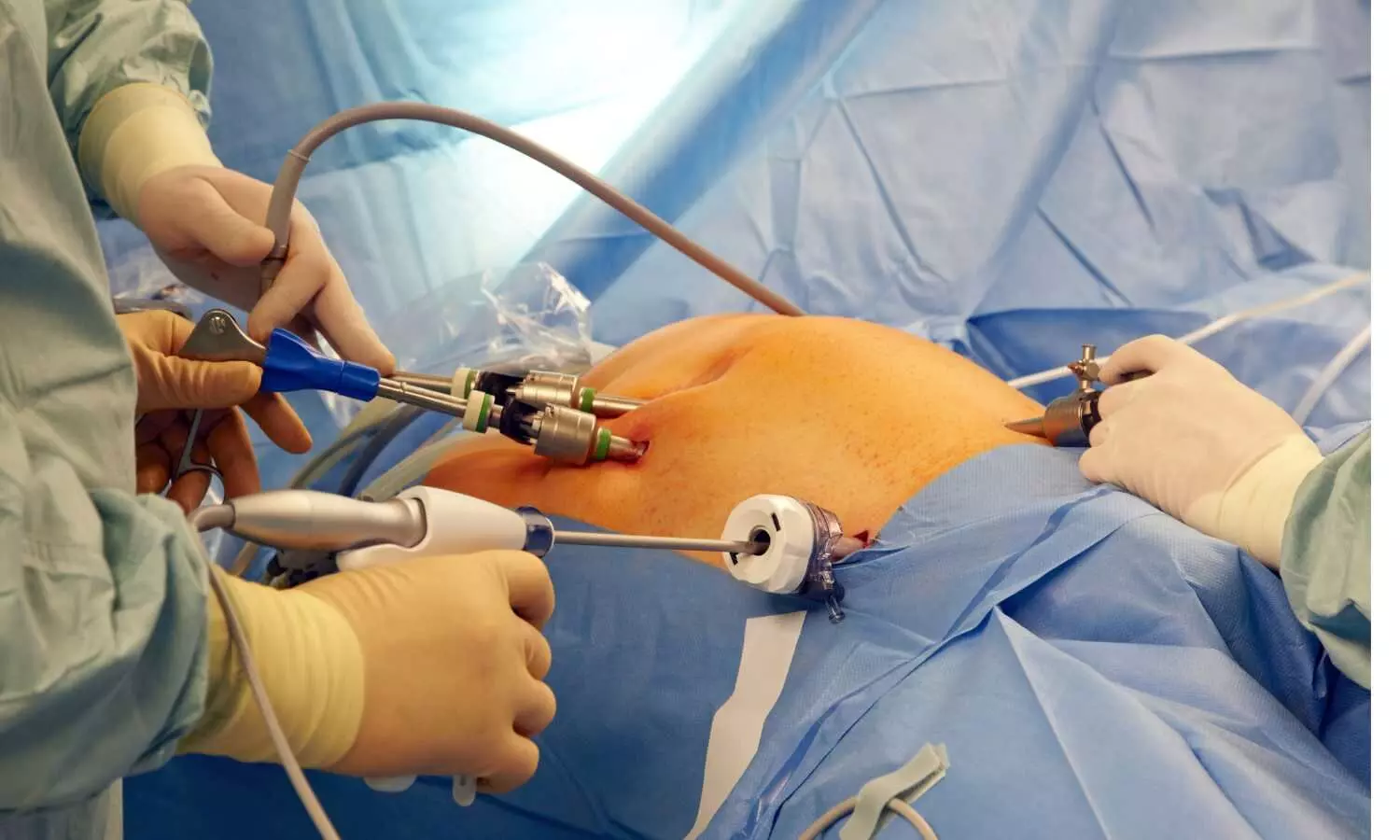
The study enrolled 400 patients with CCS who underwent revascularization by PCI. They were categorized into two categories according to their estimated glomerular filtration rate (eGFR) levels: the control group: 200 patients with eGFR ≥60mL/min/1.73m2, and the CKD Group: 200 patients with eGFR< 60ml/min/1.73m.
Reclassification of the patients was done according to revascularization into complete and incomplete revascularization groups with a one-year follow-up to assess the MACE.
Based on the study, the researchers reported the following findings:
- CKD patients were significantly older (65.78 ± 6.41 versus 56.70 ± 9.20 years). They had higher contrast-induced nephropathy, syntax scores, all-cause mortality, heart failure, and MACE.
- After reclassification according to revascularization, GFR was significantly reduced among patients with incomplete revascularization (51.08 ± 28.15 versus 65.67 ± 26.62, respectively).
- Repeated revascularization, stent thrombosis, STEMI, MACE, stroke, and all-cause mortality were more prevalent among patients with incomplete revascularization.
- Multivariate regression analysis revealed eGFR and SS as independent predictors of incomplete revascularization.
- The optimal eGFR cutoff value for predicting partial revascularization is 49.50mL/min/1.73m2, with 58.8% sensitivity and 69.3 % specificity.
“The findings showed that chronic kidney disease is linked with a higher prevalence of syntax score and incomplete revascularization in CCS patients,” the researchers wrote.
“Incomplete revascularization is also related to a higher prevalence of MACE. As a result, CKD predicts incomplete revascularization and subsequent MACE in CCS patients,” they concluded.
Reference:
Farag, S. I., Mostafa, S. A., Kabil, H., & Elfaramawy, M. R. (2023). Chronic kidney disease’s impact on revascularization and subsequent major adverse cardiovascular events in patients with chronic coronary syndrome. Indian Heart Journal. https://doi.org/10.1016/j.ihj.2023.11.006
Powered by WPeMatico