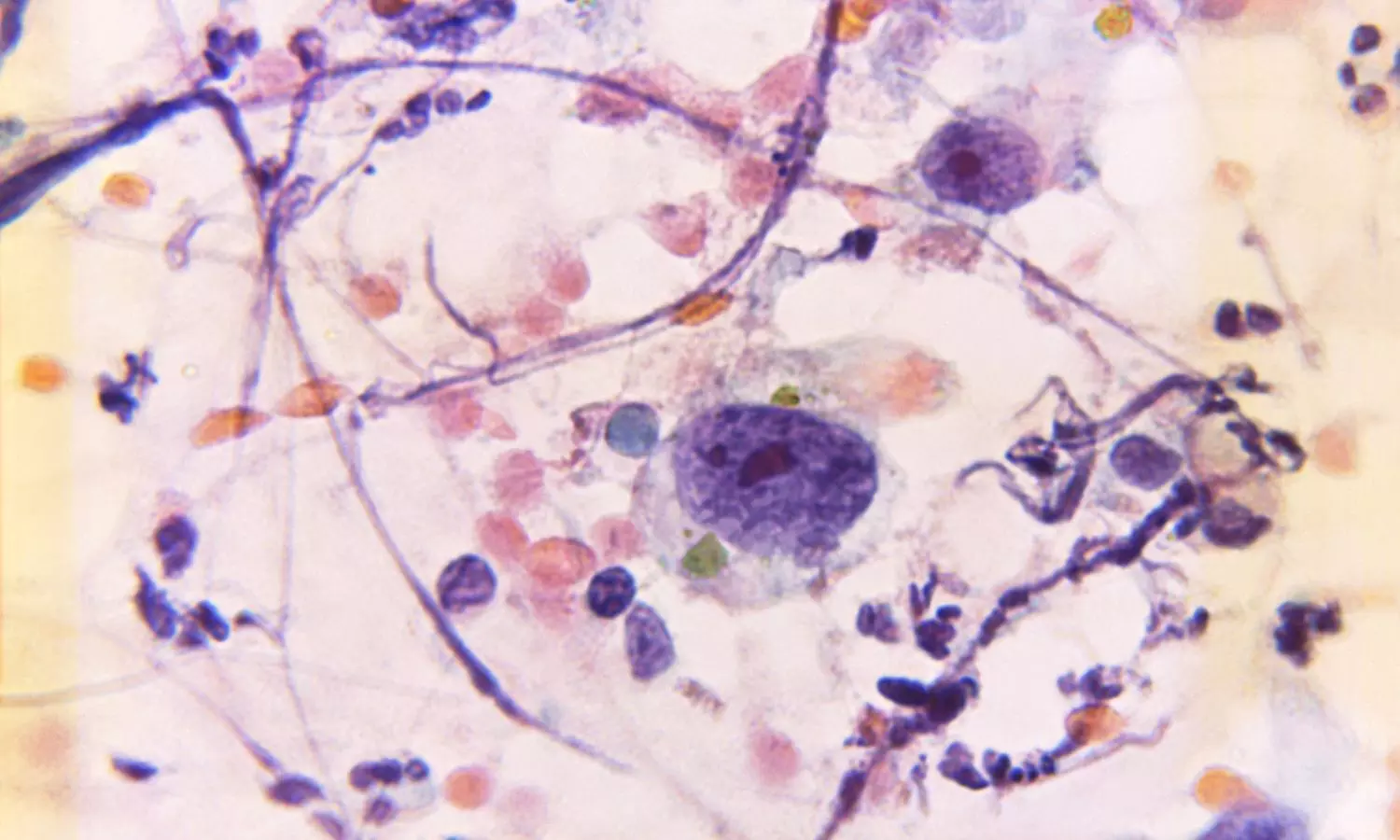
Rare but Manageable: Pediatric Patients with Leukemia Navigate COVID-19 Challenges

In a groundbreaking retrospective case series, researchers from St Jude Children’s Research Hospital and its affiliate sites shed light on the impact of COVID-19 on pediatric patients undergoing treatment for acute lymphoblastic leukemia or lymphoma (ALL/LLy). These findings contribute to our understanding of the interplay between COVID-19 and cancer treatment in pediatric patients, highlighting the challenges in maintaining chemotherapy schedules and the importance of considering individual patient characteristics in managing COVID-19 in this population.
The study results were published in the journal JAMA Network Open.
A detailed description of COVID-19 in pediatric patients with acute lymphoblastic leukemia or lymphoma (ALL/LLy) has not been provided, and its potential impact on both chemotherapy administration and long-term outcomes remains unclear. Hence, researchers conducted a study to describe the clinical presentation of COVID-19 and chemotherapy modifications in pediatric patients with ALL/LLy.
The study, conducted between March 30, 2020, and June 20, 2022, on patients treated with the Total XVII protocol, offers valuable insights into the clinical presentation of COVID-19 and the subsequent modifications in chemotherapy administration. Of the 308 pediatric patients included in the study, 110 (36%) were diagnosed with COVID-19 at a median age of 8.2 years.
Findings:
- The majority of cases occurred during the continuation/maintenance phase of chemotherapy, emphasizing the vulnerability of patients during this crucial period of their treatment journey.
- Remarkably, severe cases of COVID-19 were rare, accounting for only 6% of the affected patients.
- However, these severe instances were associated with specific factors, including older age, higher white blood cell counts at the time of ALL/LLy diagnosis, lower absolute lymphocyte counts at the onset of COVID-19, abnormal chest imaging findings, and instances of SARS-CoV-2 reinfection.
- Unprecedented in its scope, the study also highlighted rare but serious thrombotic events, such as pulmonary embolism and cerebral venous sinus thrombosis, occurring in isolated cases.
- Notably, no cases of multisystem inflammatory syndrome in children or deaths were reported among the pediatric patients.
- One of the significant challenges revealed by the study was the impact on chemotherapy administration.
- Chemotherapy interruptions affected a substantial 87% of the patients, leading to a careful examination of the duration of these interruptions.
Patients with severe disease, SARS-CoV-2 reinfection, and those diagnosed during the pre-Omicron variant period experienced longer interruptions compared to their counterparts diagnosed after December 27, 2021, when the Omicron variant emerged. SARS-CoV-2 reinfection emerged as a noteworthy aspect, occurring in 10% of patients and being more prevalent in older age groups and those receiving standard or high-risk ALL/LLy therapy. This finding underscores the need for tailored approaches to managing COVID-19 in pediatric patients, considering their specific treatment protocols. The study’s authors emphasized the necessity of conducting long-term studies to fully comprehend the outcomes of COVID-19 in this unique pediatric population. As the medical community continues to navigate the challenges posed by the pandemic, these findings contribute significantly to the evolving understanding of the intersection between COVID-19 and pediatric oncology, offering hope and insights for the future.
Further reading: Hashmi SK, Bodea J, Patni T, et al. COVID-19 in Pediatric Patients With Acute Lymphoblastic Leukemia or Lymphoma. JAMA Netw Open. 2024;7(2):e2355727. doi:10.1001/jamanetworkopen.2023.55727
Powered by WPeMatico