DSPN risk higher in patients with longer diabetes duration, higher A1C: Insights from Diabetes Prevention Program
USA: A recent study has revealed a higher average A1C and diabetes duration to be significant factors in the risk of developing distal symmetric polyneuropathy (DSPN).
Results from the Diabetes Prevention Program Outcome Study, published in Diabetes Care, informed the conclusions.
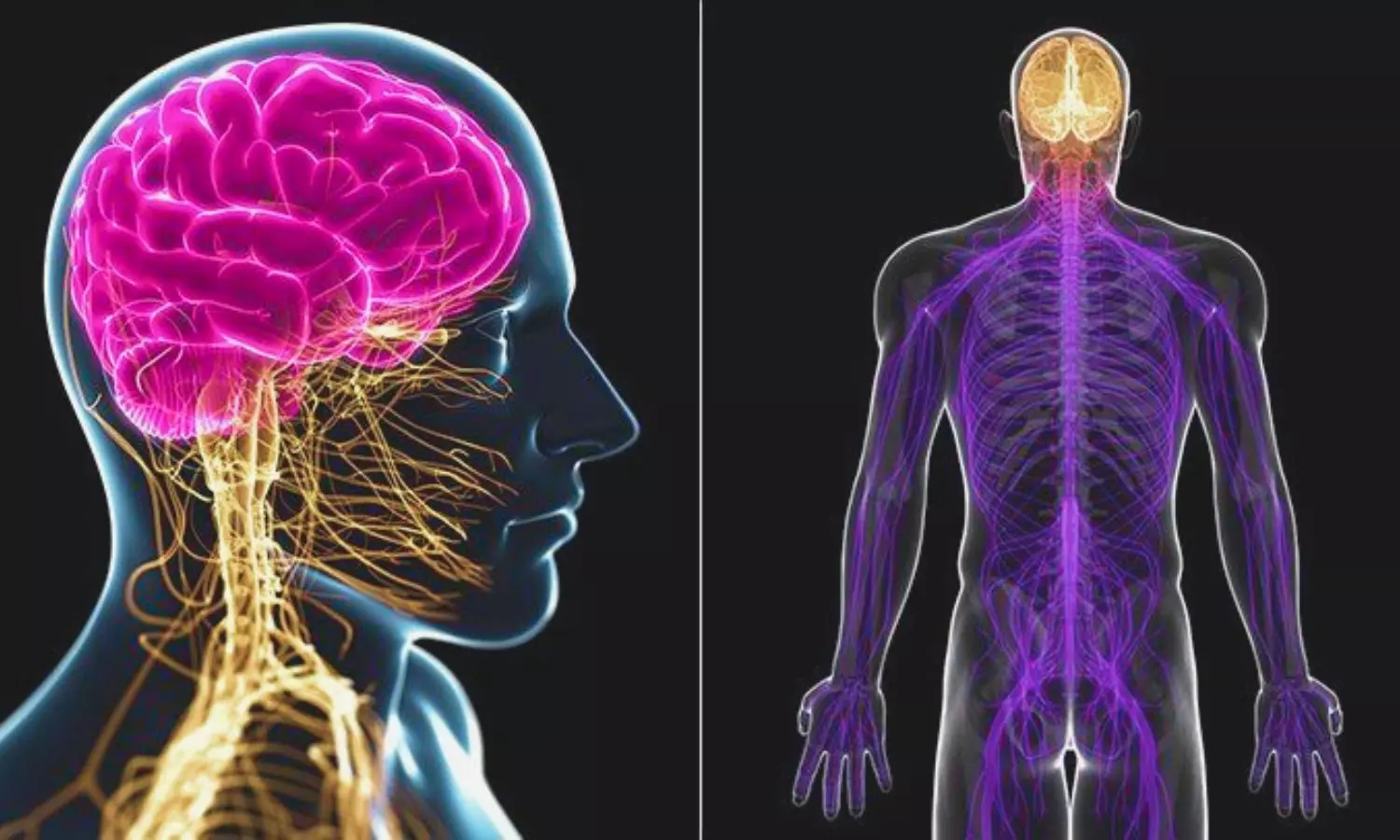
Distal symmetrical polyneuropathy (DSPN) is a common complication associated with diabetes mellitus, characterized by damage to peripheral nerves leading to sensory deficits, pain, and impaired motor function. The prevalence of DSPN among individuals with diabetes has been extensively studied, but the impact of various factors on its occurrence remains a subject of investigation.
To fill this knowledge gap, Christine G. Lee, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, and colleagues aimed to assess associations between distal symmetric polyneuropathy and Diabetes Prevention Program (DPP) treatment groups, diabetes status or duration, and cumulative glycemic exposure approximately 21 years following DPP randomization.
The DPP included 3,234 adults ≥25 years old at high risk for diabetes. They were randomized to intensive lifestyle (ILS), metformin, or placebo intervention for diabetes prevention. Following the DPP ending, 2,779 joined the Diabetes Prevention Program Outcomes Study (DPPOS).
Open-label metformin was continued, placebo was discontinued, ILS was provided as semiannual group-based classes, and all participants were offered quarterly lifestyle classes. At DPPOS year 17, signs and symptoms of DSPN were assessed in 1,792 participants. To evaluate DSPN associations with treatment group, diabetes status/duration, and cumulative glycemic exposure using multivariable logistic regression models.
The study led to the following findings:
- At 21 years after DPP randomization, 66% of subjects had diabetes. DSPN prevalence did not differ by initial DPP treatment assignment (ILS 21.5%, metformin 21.5%, and placebo 21.9%).
- There was a significant interaction between treatment assignment to ILS and age on DSPN.
- At DPPOS year 17, the odds ratio for DSPN compared to ILS with placebo was 17.4% lower with increasing 5-year age intervals.
- DSPN prevalence was slightly lower for those at risk for diabetes (19.6%) versus those with diabetes (22.7%) and was associated with longer diabetes duration and time-weighted HbA1c.
In conclusion, the likelihood of distal symmetric polyneuropathy was similar across DPP treatment groups, while higher for those with diabetes, higher cumulative glycemic exposure, and longer diabetes duration. For older adults, ILS may have long-term benefits on DSPN.
Insights from studies like the DPP provide valuable guidance for healthcare professionals in implementing strategies to mitigate or prevent DSPN risk in individuals with prediabetes or diabetes.
“Lifestyle modifications, early detection, and optimal glycemic control remain paramount in managing diabetes-related neuropathic complications,” the researchers wrote.
Reference:
Christine G. Lee, Adam Ciarleglio, Sharon L. Edelstein, Jill P. Crandall, Dana Dabelea, Ronald B. Goldberg, Steven E. Kahn, William C. Knowler, Maxwell T. Ma, Neil H. White, William H. Herman, Diabetes Prevention Program Research Group; Prevalence of Distal Symmetrical Polyneuropathy by Diabetes Prevention Program Treatment Group, Diabetes Status, Duration of Diabetes, and Cumulative Glycemic Exposure. Diabetes Care 2024; dc232009. https://doi.org/10.2337/dc23-2009
Powered by WPeMatico