Lactate IV infusion found to trick the body into releasing a hormone behind that post-workout brain boost
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
China: Using a simple nasopharyngeal airway before painless gastrointestinal endoscopy can dramatically cut the risk of dangerous oxygen drops in obese outpatients, new research in Respiratory Medicine has reported.
Powered by WPeMatico
A study presented at the European Academy of Dermatology and Venereology (EADV) Congress 2025 found that individuals with psoriasis face a significantly increased risk of developing age-related macular degeneration (AMD).
Psoriasis is a chronic, systemic inflammatory disease with multiple comorbidities, including cardiovascular disease and diabetes. This study is among the largest to date investigating whether psoriasis also predisposes individuals to AMD, an eye disease affecting millions worldwide.
Dr. Alison Treichel and her team conducted a 15-year retrospective cohort study using data from the US TriNetX collaborative network. The study included 22,901 patients over the age of 55 with psoriasis and compared their outcomes with three propensity-matched control groups: individuals with melanocytic nevi (MN) to represent other dermatology patients; patients diagnosed with major depressive disorder (MDD) to account for chronic disease and healthcare use; and patients who had undergone an ophthalmologic exam to ensure comparable opportunities for AMD diagnosis. Individuals with a prior diagnosis of AMD were excluded.
In a separate analysis, psoriasis patients treated with biologics were compared to those treated with topical corticosteroids who had not received biologics before or during the follow-up period.
Over the 10-year follow up period, people with psoriasis had a higher likelihood of developing AMD compared with patients in the MDD and MN cohorts, with a 56% and 21% increased risk, respectively. Looking at the two main forms of AMD – exudative (wet) and non-exudative (dry) – psoriasis was associated with a 40% and 13% higher risk, respectively, compared with the MDD cohort.
“Psoriasis is a systemic inflammatory disease in which lipid dysregulation contributes to cardiovascular disease,” explained Dr. Treichel. ““Because abnormal lipid deposition in the retina is a hallmark of age-related macular degeneration, particularly the dry form that causes progressive vision loss, it is biologically plausible that psoriasis could increase AMD risk. Our study is the first to demonstrate a novel association between psoriasis and non-exudative (dry) AMD and serves as a hypothesis generating observation for future studies”
Notably, psoriasis patients treated with biologic therapies had a 27% lower risk of developing AMD compared with biologic-naïve patients treated with topical corticosteroids only.
“Our findings support a connection between psoriasis and AMD, both exudative and non-exudative, which could be mediated by shared lipid dysregulation,” Dr. Treichel explained. “They also suggest that biologic therapies could offer protective benefits beyond skin symptoms. Further research is needed to determine whether these treatments have a true disease-modifying effect and to better understand the role of shared risk factors, including smoking, obesity, cardiovascular disease, and access to specialist care.”
Dr. Treichel emphasised that individuals with psoriasis should remain vigilant. “Patients with psoriasis should continue to follow standard eye exam guidelines and promptly report any changes in their vision to their healthcare providers. More research is needed before specific screening recommendations can be made.”
Looking ahead, the research team plans to build on these findings by analysing retinal imaging data from psoriasis patients to better characterise ocular abnormalities, define the prevalence of AMD, and evaluate the long-term effects of biologic therapy on disease progression.
Reference:
Psoriasis linked to increased risk of vision-threatening eye disease, study finds, Beyond, Meeting: EADV Congress 2025
Powered by WPeMatico

GLP-1 receptor agonists like Ozempic can be a lifeline for people with diabetes — helping stabilize blood glucose and lose weight which contributes to diabetes complications. But not everyone benefits equally. Scientists monitoring 92 individuals with diabetes in Japan over their first year of taking GLP-1 drugs found that people’s reasons for overeating may affect the success of these therapies. Individuals who overeat in response to the sight or smell of tasty food were most likely to respond well to the drugs in the long term, whereas individuals who overeat for emotional reasons were less likely to.
“Pre-treatment assessment of eating behavior patterns may help predict who will benefit most from GLP-1 receptor agonist therapy,” said Prof Daisuke Yabe of Kyoto University, senior author of the article in Frontiers in Clinical Diabetes and Healthcare. “GLP-1 receptor agonists are effective for individuals who experience weight gain or elevated blood glucose levels due to overeating triggered by external stimuli. However, their effectiveness is less expected in cases where emotional eating is the primary cause.”
How people eat
GLP-1 receptor agonists help lower blood glucose through several mechanisms, including boosting insulin secretion, and cause weight loss by modifying appetite. But not everyone loses weight while taking them. To investigate this problem, the researchers focused on people’s relationship to food, and what that might mean for their treatment.
They enrolled 92 people with type 2 diabetes beginning treatment with GLP-1 receptor agonists in Gifu Prefecture, Japan, and tracked their progress during their first year of treatment. At three different points — the beginning of treatment, three months later, and 12 months later — they collected data on participants’ body weight and composition, diet, and a range of relevant blood markers like blood glucose and cholesterol levels. They also asked about their relationship with food.
The scientists were particularly interested in three different types of eating behaviors associated with weight gain: emotional eating, where people eat in response to negative emotions rather than hunger, external eating, where people eat because the food looks great rather than because of hunger, and restrained eating, where people control their diet to lower their weight. In moderation, restrained eating can help with weight loss, but in excess, it can lead to disordered eating.
Different bodies, different results
In general, individuals saw a statistically significant reduction in body weight, cholesterol levels, and body fat percentage over the course of the year, while skeletal muscle mass stayed the same. Blood glucose levels also improved, but the improvements weren’t statistically significant.
However, there were some differences in results based on eating behaviors. At the three-month mark, participants reported more behaviors associated with restrained eating, and fewer behaviors associated with external or emotional eating. However, by the 12-month point, restrained and emotional eating behaviors returned to their baseline levels.
“One possible explanation is that emotional eating is more strongly influenced by psychological factors which may not be directly addressed by GLP-1 receptor agonist therapy,” said Dr Takehiro Kato of Gifu University, second author of the article. “Individuals with prominent emotional eating tendencies may require additional behavioral or psychological support.”
The scientists also didn’t find links between emotional or restrained eating scores at the beginning of treatment and the benefits that participants saw from the drugs by the end of the year. By contrast, the decrease in external eating was sustained over the full year, and people who reported high levels of external eating at the start saw the best results in terms of weight loss and blood glucose levels.
Although this study has the advantage of following individuals with diabetes under real-life conditions, as an observational study using self-reported measures, it can’t determine causation. The researchers also pointed out that this group of people may have been especially highly motivated to try to improve their control over their diabetes, which might have resulted in greater weight loss.
“While our study suggests a potential association between external eating behavior and treatment response to GLP-1 receptor agonists, these findings remain preliminary,” said Yabe. “Further evidence is necessary before they can be implemented in clinical practice. Should future large-scale or randomized controlled trials validate this relationship, incorporating simple behavioral assessments could become a valuable component in optimizing treatment strategies.”
Reference:Yuya Koide1,2,3Takehiro Kato,*Takehiro Kato1,2*Makoto HayashiMakoto Hayashi3Hisashi DaidoHisashi Daido4Takako MaruyamaTakako Maruyama5Takuma IshiharaTakuma Ishihara6Kayoko NishimuraKayoko Nishimura7Shin TsunekawaShin Tsunekawa8Daisuke Yabe,,,*Daisuke Yabe1,2,8,9* on behalf of G-DIET Investigators DOI: 10.3389/fcdhc.2025.1638681 Frontiers in Clinical Diabetes and Healthcare.
Powered by WPeMatico
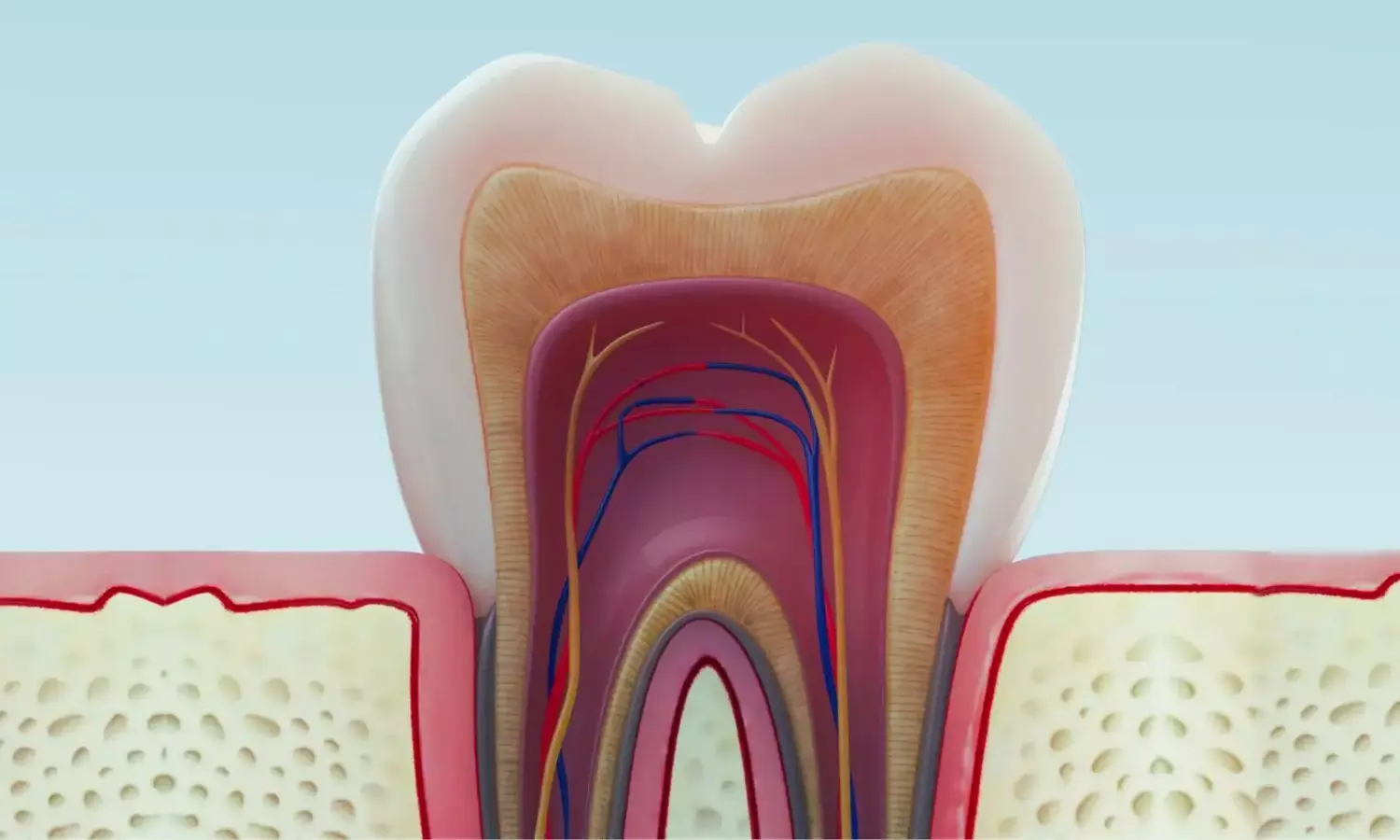
India: 1% phytic acid is a suitable irrigating solution compared to 17% EDTA, as it causes less demineralization of radicular dentin. This conclusion comes from a recent in vitro study published in the Journal of Conservative Dentistry and Endodontics, which assessed the effect of these irrigants on calcium ion loss and the microhardness of root canal dentin.
Powered by WPeMatico

Researchers have found in a large study of 927,130 adults that skipping breakfast raised fracture risk by 18% and late-night dinners by 8%. Smoking also increased risk, while daily alcohol intake, faster walking speed, and adequate sleep were protective, underscoring the role of meal timing in bone health.
People who skip breakfast and eat late dinners may have an increased risk of developing osteoporosis, according to a new study published in the Journal of the Endocrine Society.
Lifestyle habits, such as exercise, alcohol consumption and smoking, are known to increase people’s risk of osteoporosis, however little is known about the association between osteoporotic fracture and diet.
“This study aimed to examine the association between lifestyle habits such as diet, and the risk of osteoporotic fracture,” said study author Hiroki Nakajima, M.D., Ph.D., of Nara Medical University in Nara, Japan. “We found skipping breakfast and having late dinners was associated with an increased risk of osteoporosis. Furthermore, these unhealthy eating habits were found to be linked with the accumulation of other lifestyle risk factors such as physical inactivity, smoking and insufficient sleep.”
The researchers used a large health checkup cohort of 927,130 adults (45.3% male and 54.7% female) from a Japanese claims database to find the association between lifestyle factors and the diagnosis of osteoporotic fracture (hip, forearm, vertebral and humeral fractures).
They found people who had unhealthy habits such as smoking, daily alcohol consumption, not enough exercise or sleep, skipping breakfast, and having late dinners, were more likely to be diagnosed with osteoporosis.
“These results suggest that preventing osteoporosis and fractures requires not only healthy eating habits but also a broader effort to improve overall lifestyle behaviors,” Nakajima said.
Reference:
Hiroki Nakajima, Dietary Habits and Osteoporotic Fracture Risk: Retrospective Cohort Study Using Large-Scale Claims Data, Journal of the Endocrine Society, https://doi.org/10.1210/jendso/bvaf127.
Powered by WPeMatico
