A central theme of the updated guidelines is the reinforced importance of a multidisciplinary Heart Team operating within an integrated regional Heart Valve Network. This network approach, which incorporates outpatient clinics and specialist Heart Valve Centres, aims to ensure timely diagnosis and optimal patient care. The guidelines recommend that complex procedures be concentrated in high-volume, experienced centers to ensure high-quality treatment.
The 2025 update also highlights the growing importance of advanced imaging modalities. Techniques such as three-dimensional (3D) echocardiography, cardiac computed tomography (CCT), and
cardiac magnetic resonance (CMR) have become crucial for the screening, evaluation, and intervention planning for patients with VHD.
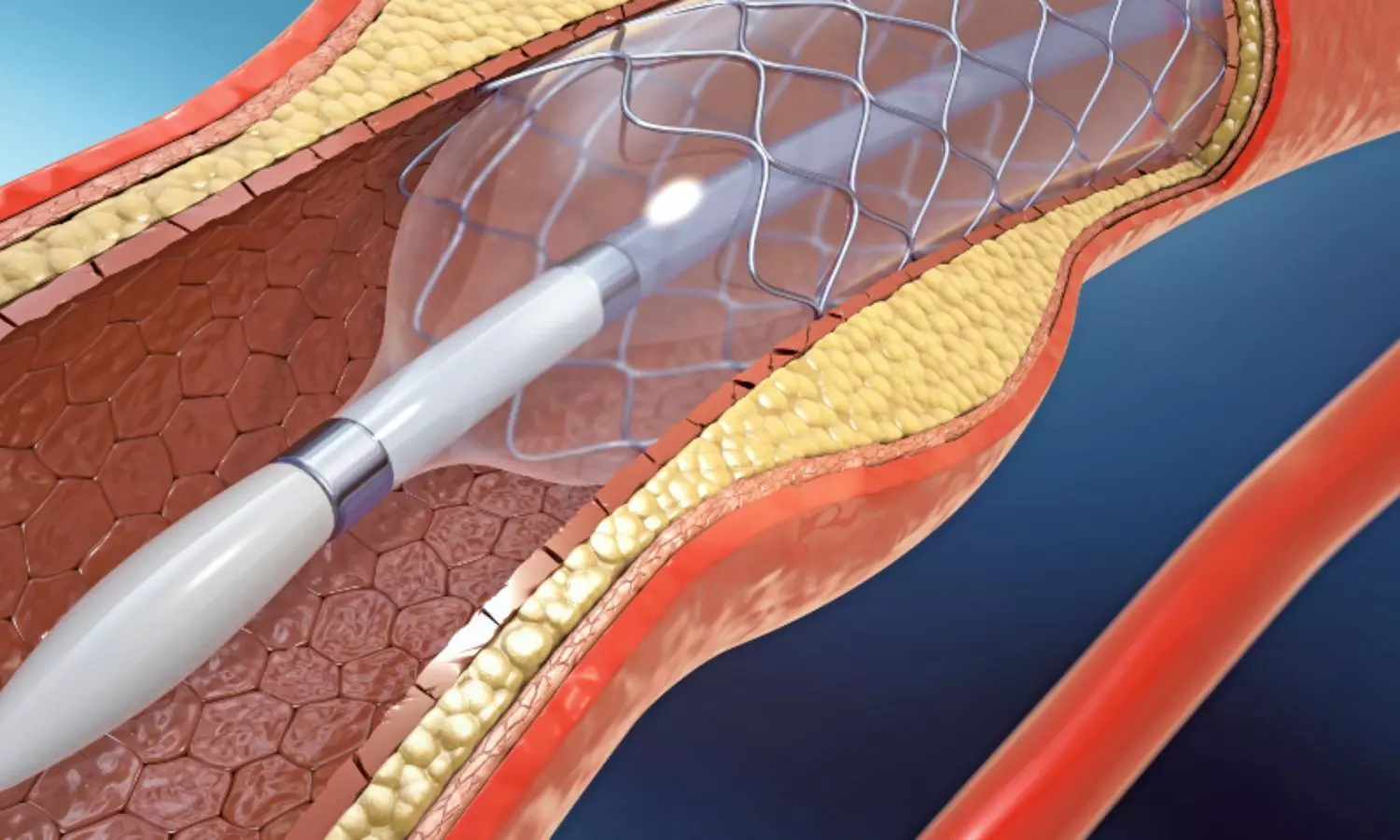
Significant new evidence has reshaped recommendations for specific conditions. For severe aortic stenosis (AS), intervention is now supported irrespective of symptoms, left ventricular ejection fraction, or flow reserve. The criteria for selecting between transcatheter aortic valve implantation (TAVI) and surgical aortic valve replacement (SAVR) have been refined, incorporating a combination of age, procedural risk, anatomical suitability, and lifetime management considerations.
In
mitral regurgitation (MR), the guidelines stress the importance of correctly assessing the cause and distinguishing between atrial and ventricular secondary mitral regurgitation (SMR), as this has clear implications for prognosis and management. For tricuspid regurgitation (TR), growing evidence supports concomitant TV repair during left-sided valve surgery and highlights the role of transcatheter options in improving quality of life.
The guidelines also feature updated recommendations on the use of direct oral anticoagulants (DOACs) and introduce a new dedicated section on sex-specific considerations in patients with VHD.
Key Takeaways from the 2025 ESC/EACTS VHD Guidelines:
1. Heart Team and Network: An integrated regional Heart Valve Network, with Heart Teams at its core, is essential for optimal patient care. Complex procedures should be performed in the most experienced centers.
2. Advanced Imaging: Multimodality imaging, including 3D echocardiography, CCT, and CMR, is now central to the diagnosis, planning, and guiding of interventions in VHD.
3. Aortic Stenosis (AS) Intervention: Intervention is recommended for symptomatic patients with severe AS. The choice between TAVI and SAVR is based on Heart Team assessment of age, life expectancy, procedural risk, and lifetime management. TAVI is recommended for suitable patients aged ≥70 years.
4. Asymptomatic Severe AS: For asymptomatic patients with severe, high-gradient AS and low procedural risk, early intervention should be considered as an alternative to close active surveillance.
5. Mitral Regurgitation (MR) Classification: Distinguishing between primary, ventricular secondary, and atrial secondary MR is crucial, as the evaluation and management differ for each type.
6. Secondary MR Management: Guideline-directed medical therapy is the essential first step for ventricular SMR. TEER is recommended for specific symptomatic patients to reduce heart failure hospitalizations. For atrial SMR, surgery and AF ablation should be considered.
7. Tricuspid Regurgitation (TR): Concomitant TV repair is preferred for patients with moderate or severe TR undergoing left-sided valve surgery. For high-risk patients with isolated severe TR, transcatheter treatment should be considered to improve quality of life.
8. Mixed Aortic Valve Disease: Intervention is recommended for symptomatic patients with mixed moderate AS and moderate AR if they present with a high gradient (mean gradient ≥40 mmHg or Vmax ≥4.0 m/s).
9. Mechanical Heart Valves (MHV): Lifelong anticoagulation with a Vitamin K antagonist (VKA) is required. Patient education and INR self-monitoring are recommended to improve efficacy.
10. Sex-Specific Considerations: A new dedicated section acknowledges sex-specific differences in VHD prevalence, pathophysiology, and outcomes, which may influence management strategies.
The authors stress that these recommendations support, but do not override, individual clinical judgment. By identifying key gaps in evidence, the guidelines standardize care and direct future research.
Reference:
Praz, F., Borger, M. A., Lanz, J., Abreu, A., Adamo, M., Ajmone Marsan, N., Barili, F., Bonaros, N., Cosyns, B., De Paulis, R., Gamra, H., Jahangiri, M., Jeppsson, A., Klautz, R. J., Mores, B., Pöss, J., Prendergast, B. D., Rocca, B., Rossello, X., . . . Moorjani, N. 2025 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the task force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal. https://doi.org/10.1093/eurheartj/ehaf194