Immediate iFR-Guided PCI Not Superior to Deferred CMR-Guided for Non-Culprit Lesions in STEMI – TCT 2025
This news was covered by the Medical Dialogues Bureau, which was present at the TCT Conference 2025 held in San Francisco, USA.
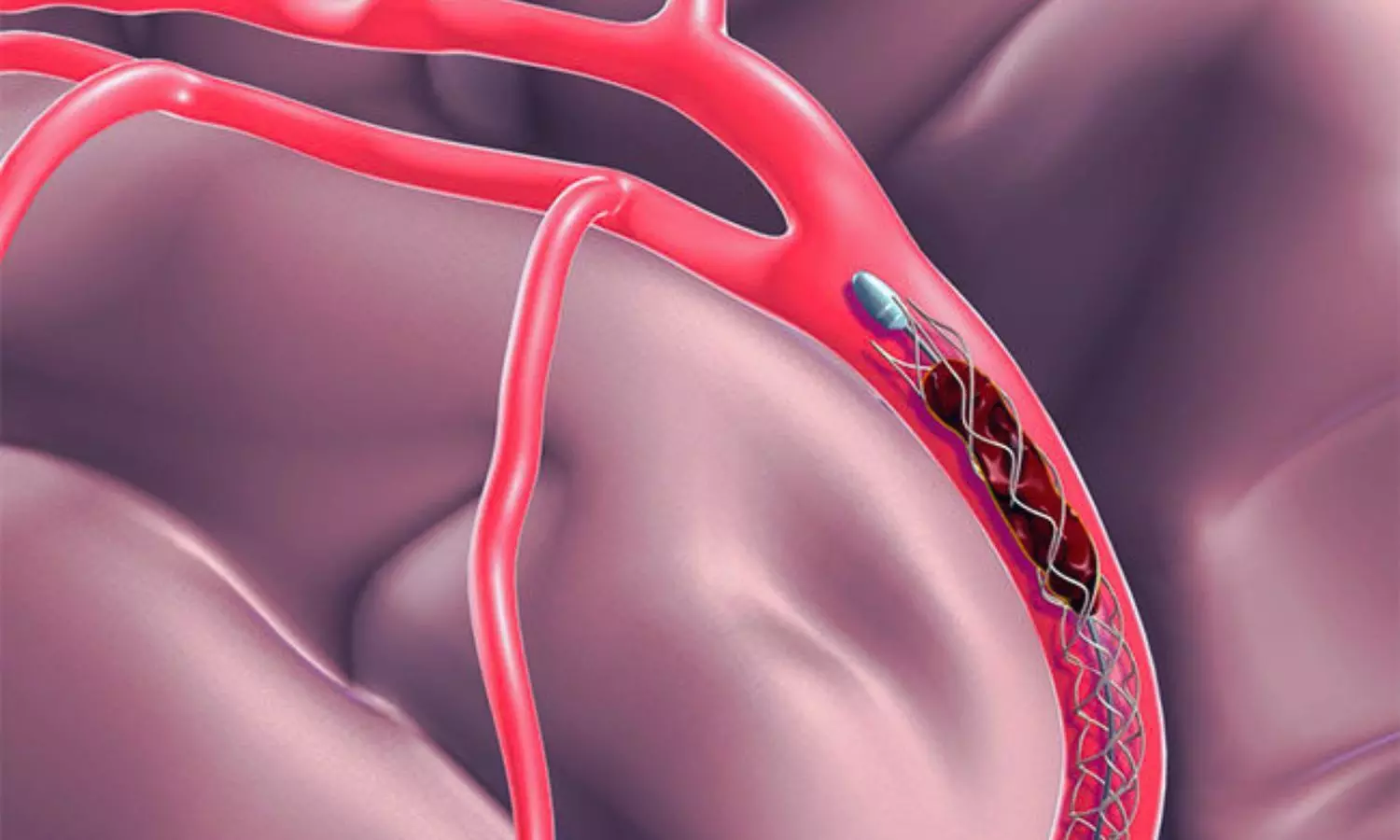
Immediate instantaneous wave-free ratio (iFR)–guided percutaneous coronary intervention (PCI) was not superior to a deferred cardiac magnetic resonance (CMR)–guided PCI approach for non-culprit lesions in patients with ST-segment elevation myocardial infarction (STEMI) and multivessel disease, according to results from the iMODERN trial presented by Dr. Robin Nijveldt at TCT 2025.
The iMODERN trial was an international, investigator-initiated, open-label, randomized controlled study designed to compare immediate iFR-guided revascularization with a deferred, CMR-guided strategy within six weeks of primary PCI.
A total of 1,143 patients were enrolled across 41 sites and randomized to immediate iFR-guided PCI (n=556) or deferred CMR-guided PCI (n=587). Eligible patients presented with acute STEMI and at least one non-culprit lesion greater than 50% stenosis. Baseline characteristics were balanced between groups, with a mean age of 63 years and approximately 78% male participants.
In procedure and per-patient treatment patterns, the immediate iFR arm had a higher rate of identified positive non-culprit lesions (43.7% vs 21.8%) and a higher rate of PCI of positive lesions (42.6% vs 18.7%). Total procedural time (culprit + non-culprit) was shorter with immediate iFR (75.4 ± 33.3 minutes vs 90.0 ± 43.7 minutes), and mean total stent length was greater in the iFR arm (48.7 ± 29.7 mm vs 42.1 ± 27.7 mm). Time to non-culprit PCI was immediate in the iFR arm and a median 40 days (IQR 28–58) in the CMR arm.
For the primary endpoint—a composite of all-cause death, recurrent myocardial infarction, or hospitalization for heart failure at three years—no significant difference was observed between the two strategies (hazard ratio 0.95; 95% confidence interval 0.65–1.40; p=0.81).
Secondary and sensitivity analyses (as-treated and per-protocol) produced consistent findings: target-lesion failure at three years was similar (10.2% vs 10.5%), and rates of recurrent MI and overall cardiac death were comparable between arms. Notable secondary observations included fewer stroke/transient ischemic attack events in the iFR arm (1.3% vs 3.7%; HR 0.36) and a lower hospitalization-for-heart-failure rate at 12 months (0.4% vs 1.8%; HR 0.21), but overall clinical event rates remained low and without a clear advantage for immediate physiology-guided revascularization.
At three years, rates of target lesion failure, recurrent myocardial infarction, cardiac death, and unplanned revascularization were comparable between groups. Both approaches resulted in low long-term event rates, with no evidence of harm from either strategy.
Investigators concluded that immediate physiology-guided revascularization did not improve long-term outcomes compared with deferred CMR-guided assessment for non-culprit lesions in STEMI with multivessel disease.
Reference: Robin Nijveldt, Immediate Instantaneous Wave-Free Ratio Guided Versus Deferred Cardiac Magnetic Resonance Imaging Guided Revascularization of Non-Culprit Lesions in Patients with Acute STEMI: A Randomized Superiority Trial, TCT Conference 2025, San Francisco.
https://www.tctconference.com/
About the Study Presenter: Robin Nijveldt is Professor of Cardiovascular Imaging and Cardiologist at the Radboud University Medical Center (Nijmegen, the Netherlands), and connected to the Radboud Institute for Health Sciences. He works at the department of Cardiology and focuses on the Vascular damage research theme, with a special interest in Cardiovascular Magnetic Resonance imaging, CT and echocardiography, and in close collaboration with the department of Radiology. His research explores new imaging techniques and innovative strategies on today’s scientific health challenges, aiming to improve patient outcome in a personalized approach. He currently serves as Vice-President of the European Association of Cardiovascular Imaging (EACVI) and CMR section chair.
Powered by WPeMatico