SC to hear NEET PG exam case on October 4

Powered by WPeMatico

Powered by WPeMatico

Japan: A recent case report published in BMC Nephrology sheds light on the long-term management of intermediate cystinosis with a decade-long cysteamine therapy. This rare and insightful case highlights the effectiveness of early diagnosis and sustained treatment in stabilizing renal function in affected patients.
Intermediate cystinosis, a rare lysosomal storage disorder, poses diagnostic challenges due to its diverse clinical presentations and slower progression compared to nephropathic cystinosis. This condition affects roughly 5% of cystinosis cases and can lead to end-stage kidney disease (ESKD) if diagnosis and treatment are delayed. Unlike other types, intermediate cystinosis may not present with classic symptoms like Fanconi syndrome or ocular manifestations, making diagnosis challenging. Additionally, the management of this condition can be complicated, as cystine-depleting medications such as cysteamine are difficult for many patients to tolerate due to complex administration requirements and side effects. The report details a case of intermediate cystinosis successfully managed with a decade-long course of cysteamine treatment.
Daisuke Katagiri, Center Hospital of the National Center for Global Health and Medicine (NCGM), Tokyo, Japan, and colleagues described the case of a patient who initially showed urinary abnormalities at age three during a routine health examination for children—a screening unique to Japan. Cystinosis was confirmed when the patient turned 12, leading to the initiation of cysteamine therapy and regular monitoring of cystine levels.
Despite persistent proteinuria, the patient’s renal function advanced slowly. Two renal biopsies revealed multinucleated podocytes and cystine crystals but no focal segmental glomerulosclerosis. Throughout the treatment, the patient’s renal function remained stable.
In this case, the patient was initially diagnosed with cystinosis at age 12, based on symptoms including Fanconi syndrome, proteinuria, and corneal cystine deposits. Cysteamine treatment commenced and was maintained for ten years. Two renal biopsies conducted during this period revealed multinucleated podocytes and cystine crystals, confirming the diagnosis. Despite persistent proteinuria, renal function remained stable, showcasing the efficacy of long-term cysteamine therapy.
Intermediate cystinosis often lacks the hallmark symptoms of nephropathic cystinosis and can be difficult to diagnose. A specific health screening for 3-year-olds in Japan enabled early detection in this patient, which was crucial for successful treatment. Cysteamine remains the only effective treatment, though it is challenging to administer due to side effects and its distinctive odor. Continuous treatment and adherence are essential for improving outcomes and delaying complications.
“Our case underscores the importance of early diagnosis and sustained cysteamine therapy in managing intermediate cystinosis. While the use of renal biopsies in ongoing treatment is rare, our findings suggest they are valuable for monitoring disease progression and treatment efficacy. Further research is needed to understand the implications of multinucleated podocytes and their relationship to glomerular damage in cystinosis,” the researchers concluded.
Reference:
Kawamura, M., Katagiri, D., Yamamoto, Y. et al. Intermediate cystinosis: a case report of 10-year treatment with cysteamine. BMC Nephrol 25, 275 (2024). https://doi.org/10.1186/s12882-024-03722-8
Powered by WPeMatico
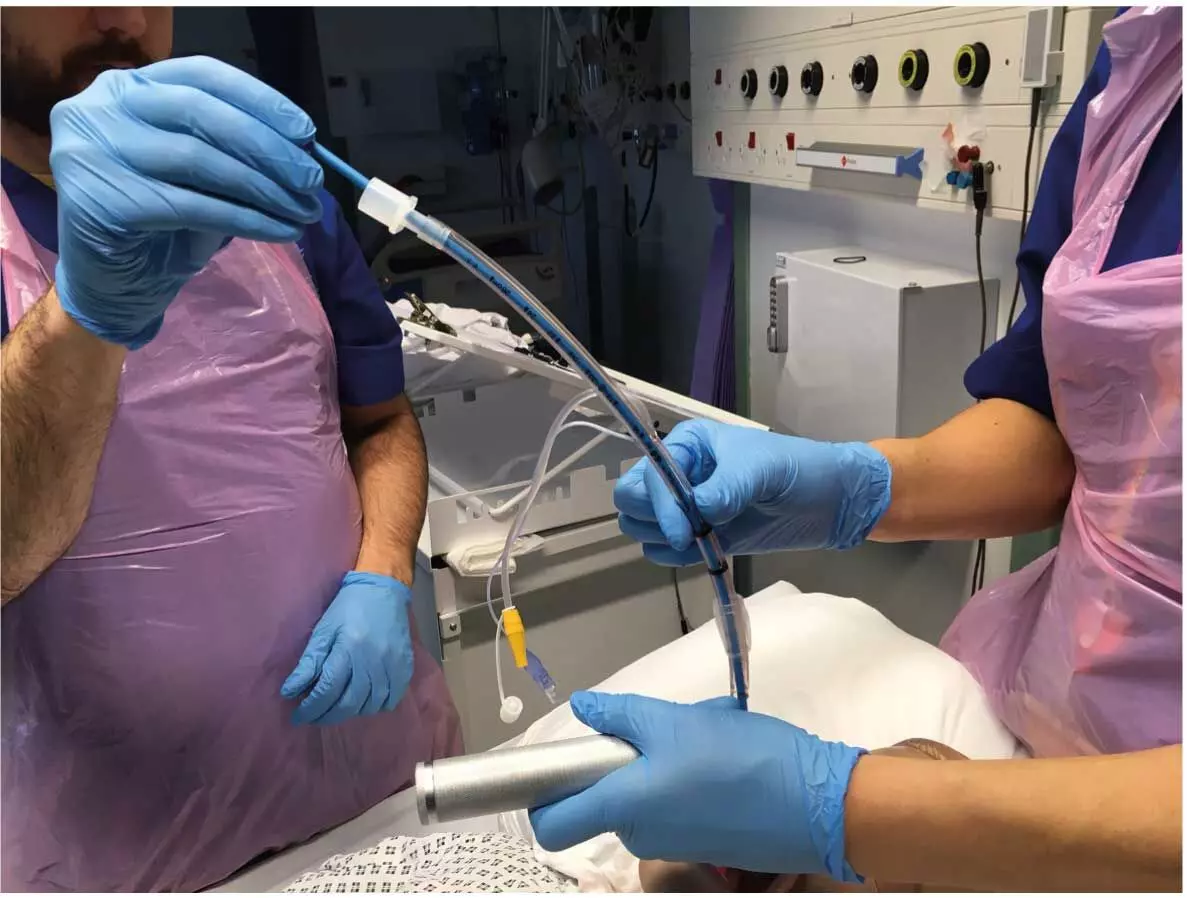
Accurate airway management is crucial in thoracic surgeries, especially those involving lung resections. Achieving ideal lung isolation is vital for patient safety and surgical effectiveness. While double-lumen tubes (DLTs) are now the standard for lung isolation, the task of selecting the right DLT size remains difficult. Recent research paper investigates the use of ultrasonography (USG) and computed tomography (CT) in measuring cricoid cartilage diameter for objective double-lumen tube (DLT) sizing in thoracic surgeries. The study involves a randomized comparative trial of 120 adult patients undergoing thoracic surgery, grouped into USG, CT, and conventional DLT size determination based on height and gender. The primary outcomes were appropriateness of DLT size, degree of lung collapse, and sore throat. The results indicated improved accuracy of DLT sizing based on cricoid cartilage diameter, with significantly lower rates of inappropriate sizes and better outcomes in lung collapse and sore throat in the USG and CT groups compared to the conventional group.
Methodology and Tool Exploration
The research discusses the challenges of selecting the correct DLT size for thoracic surgeries, a vital aspect of airway management. Factors such as patient height, gender, tracheal diameter, left main bronchial (LMB) diameter, and cricoid cartilage transverse diameter play significant roles in DLT size selection. Ultrasonography and computed tomography are explored as tools for accurately measuring the cricoid cartilage diameter, with advantages such as quick, convenient, safe, and radiation-free assessment of airway anatomy. The study is based on a single-center trial with 120 adult patients, and the primary inclusion criteria were patients undergoing thoracic surgery requiring single-lung ventilation, excluding those with anticipated difficult airways. The results showed that DLT sizing based on cricoid cartilage diameter improved accuracy, with significantly lower rates of inappropriate sizes in the USG and CT groups compared to the conventional group. Lung collapse was also better in the USG and CT groups, with significantly lower rates of sore throat in these groups compared to the conventional group. The study underscores the superiority of USG and CT in DLT measurement over the conventional group, and the compatibility of USG with real-time, non-invasive, and cost-effective measurements. The paper acknowledges the limitations of the study, such as being a single-center trial and not examining other anatomical parameters that may influence DLT size selection. However, the study’s results indicate that ultrasonography and computed tomography-guided measurement of cricoid cartilage diameter is a reliable and effective method compared to the conventional method for determining the size of a double-lumen tube in thoracic surgery.
Key Points
– The study focused on the use of ultrasonography (USG) and computed tomography (CT) to measure cricoid cartilage diameter for objective double-lumen tube (DLT) sizing in thoracic surgeries.
– The research involved a randomized comparative trial of 120 adult patients undergoing thoracic surgery, categorized into USG, CT, and conventional DLT size determination based on height and gender, with the primary outcomes being appropriateness of DLT size, degree of lung collapse, and sore throat.
– The article discussed the callenges of selecting the correct DLT size for thoracic surgeries, considering factors such as patient height, gender, tracheal diameter, left main bronchial (LMB) diameter, and cricoid cartilage transverse diameter.
– Ultrasonography and computed tomography were explored as tools for accurately measuring the cricoid cartilage diameter, with advantages including quick, convenient, safe, and radiation-free assessment of airway anatomy. – The results showed improved accuracy of DLT sizing based on cricoid cartilage diameter, with significantly lower rates of inappropriate sizes and better outcomes in lung collapse and sore throat in the USG and CT groups compared to the conventional group.
– The study acknowledged limitations such as being a single-center trial and not examining other anatomical parameters that may influence DLT size selection, but concluded that ultrasonography and computed tomography-guided measurement of cricoid cartilage diameter is a reliable and effective method for determining the size of a double-lumen tube in thoracic surgery.
Reference –
Mathew RM, Gautam S, Raman R, Rai A, Srivastava VK, Singh MK. Evaluating the precision of ultrasound versus computed tomography‑guided measurement of cricoid cartilage diameter for double‑lumen tube selection in thoracic surgery: A randomised comparative study. Indian J Anaesth 2024;68:896‑901
Powered by WPeMatico

China: A recent study investigating the relationship between high-density lipoprotein cholesterol (HDL-C) and vitamin D deficiency in adults aged 20 to 59 has shed light on an important aspect of cardiovascular health. The findings were published online in BMC Endocrine Disorders.
Utilizing data from the National Health and Nutrition Examination Survey (NHANES), researchers found a significant association between HDL-C levels and serum 25-hydroxyvitamin D (25(OH)D) levels, highlighting the need for integrated monitoring of these two crucial health indicators. Based on the findings, the researchers suggest that boosting vitamin D intake should be a priority, especially for males with low HDL-C levels, to help prevent associated health problems.
HDL-C is often referred to as “good cholesterol” due to its role in transporting cholesterol away from arteries and back to the liver, where it can be processed and eliminated. Higher levels of HDL-C are associated with a reduced risk of heart disease, making it a key target for cardiovascular health management. Meanwhile, vitamin D is essential for various bodily functions, including bone health and immune function. Recent evidence suggests that it may also play a role in lipid metabolism and cardiovascular risk.
Serum lipids are significantly influenced by genetics and are crucial for cardiovascular and metabolic health. However, the connection between high-density lipoprotein cholesterol (HDL-C) and serum 25(OH)D levels remains uncertain. Considering this, the researchers Biting Zhao & Shuang Yang from China aimed to investigate the relationship between serum 25(OH)D levels and HDL-C in adults aged 20 to 59.
For this purpose, the researchers utilized data from the NHANES in the cross-sectional study. They employed multivariable logistic regression to assess the relationship between HDL-C and serum 25(OH)D levels, along with additional analyses using smooth spline fitting and generalized additive models. The study included a total of 28,084 adults.
Based on the study, the following findings were revealed:
The study authors demonstrated a significant positive correlation between HDL-C levels and serum 25(OH)D levels, revealing notable gender-specific differences. In females, the relationship remains consistently positive, while in males, it takes on an inverted U-shaped curve. These findings underscore the importance of considering gender when assessing the connection between HDL-C and vitamin D levels.
The clinical and public health implications of these results are substantial. The authors recommend concurrent monitoring of HDL-C and vitamin D levels to provide a more comprehensive evaluation of cardiovascular risk.
“For individuals, especially males with lower HDL-C levels, the authors suggest that increasing vitamin D intake should be considered to enhance overall health and prevent deficiencies that could impact cardiovascular and skeletal health,” they concluded.
Reference:
Zhao, B., Yang, S. Exploring the unique association between high-density lipoprotein cholesterol and vitamin D deficiency in adults aged 20–59: findings based on the NHANES database. BMC Endocr Disord 24, 192 (2024). https://doi.org/10.1186/s12902-024-01719-w
Powered by WPeMatico

A new study shows the potential power of imaging paired with radiation to shape treatment for glioblastoma patients in real time.
The study, led by researchers at Sylvester Comprehensive Cancer Center, part of the University of Miami Miller School of Medicine, is the first to quantify tumor changes in glioblastoma patients receiving MRI-guided radiation therapy. This novel technique, also known as MRI-linear accelerator or MRI-linac, pairs daily imaging with radiation. Sylvester was the first to use this technology for patients with glioblastoma and remains one of the few cancer centers to offer it for the disease.
The Sylvester researchers found that this daily imaging can serve as an important monitoring system to signal tumor growth during treatment earlier than standard imaging, providing evidence that the method could one day be used to guide rapid treatment adaptation during radiation therapy.
The study was published Sept. 30 in the International Journal of Radiation Oncology-Biology-Physics and simultaneously presented at the American Society for Radiation Oncology (ASTRO) meeting by the study’s first author, Kaylie Cullison, Ph.D., an M.D./Ph.D. student in the Miller School’s Medical Scientist Training Program.
“Our study shows that these daily scans can serve as an early warning sign for potential tumor growth,” Cullison said.
In the study, which was led by Eric A. Mellon, M.D., Ph.D., a radiation oncologist and co-leader of Sylvester’s Neurologic Cancer Site Disease Group, the researchers followed 36 glioblastoma patients over a six-week course of daily radiation and MRI scans using MRI-linac. They then compared the data from these daily scans to standard-of-care imaging to measure tumor size, namely, a single MRI image with contrast performed one week before radiation treatment and another a month after the radiation course is completed. Although MRI-linac could be paired with a contrast agent, some patients are concerned about frequent use of these heavy metals, so the study was conducted without contrast for the daily scans.
Typically, brain radiation is guided by X-ray or CT scan to position the patient correctly under the radiation beam. But these kinds of imaging only reveal the position of the skull.
“Any machine that does not include MRI, which is 99% of radiation-delivery equipment out there, cannot see what’s going on inside of the brain,” Mellon said. “MRI-linac allows you to see what’s going on in the brain, for the first time.”
The researchers found that for 74% of the trial participants, their MRI-linac imaging matched the information found in the typical, contrast MRI performed before and after treatment. That is, both modalities agreed on whether the patients’ tumors grew, shrank, or remained the same size during the course of radiation therapy. For the other 26% of patients, the MRI-linac imaging predicted tumor growth while the pre- and post-treatment imaging showed that the tumor shrank.
Although the daily MRI did not agree with the contrast imaging 100% of the time, the fact that it did not miss any cases of true tumor growth suggests that it could be used to signal possible tumor growth during radiation therapy, the researchers said. That signal could then be confirmed with contrast imaging and, ultimately, could be used to adapt the patient’s treatment to more quickly address the tumor growth.
The daily imaging could also be useful in other cases besides tumor growth. If a tumor is shrinking, the radiation field could be narrowed to ensure only cancerous tissue is targeted. Additionally, most glioblastoma patients undergo surgery before radiation therapy, and the site where the tumor was removed, the surgical resection cavity, often shrinks as the brain heals. Following that shrinkage over time and changing the radiation therapy accordingly could be critical to spare healthy tissue from irradiation. In their current study, the Sylvester researchers traced changes in both the tumor size and surgical cavity size.
Mellon and his team plan to conduct future studies to test MRI-linac’s ability to guide treatment decisions for glioblastoma patients during the course of radiation therapy as well as to test the method in other types of brain cancer. Because so few clinics use the technology to treat brain cancers, it was not realized prior to Mellon’s studies that glioblastomas change significantly during radiation. The research team hopes to use that knowledge to improve outcomes for patients with this all-too-often deadly form of cancer.
Reference:
Cullison, Kaylie et al.Dynamics of Daily Glioblastoma Evolution During Chemoradiotherapy on the 0.35T MRI-Linear Accelerator, International Journal of Radiation Oncology, Biology, Physics, doi:10.1016/j.ijrobp.2024.09.028.
Powered by WPeMatico

Ahmedabad: Zydus Lifesciences Limited has received tentative approval from the United States Food and Drug Administration (USFDA) to manufacture Enzalutamide Tablets, 40 mg and 80 mg (USRLD: Xtandi Tablets, 40 mg, 80 mg).
Zydus Lifesciences Ltd. is an innovative, global life sciences company that discovers, develops, manufactures, and markets a broad range of healthcare therapies. Zydus has been actively discovering and developing New Chemical Entities (NCEs) novel biologicals, several biosimilars and vaccines as a part of its innovation pipeline. Over the last decade, Zydus has introduced several products in the market for treating unmet healthcare needs with vaccines, therapeutics, biologicals and biosimilars
Read also: Zydus, CSIR-CDRI Lucknow to develop drug for Chronic Kidney Disease induced Osteoporosis
Powered by WPeMatico

People with low- and intermediate-risk prostate cancer treated with either of two types of contemporary radiation therapy-proton beam therapy or intensity modulated radiation therapy (IMRT)-achieved equally high rates of tumor control with no differences in patient-reported quality of life, according to a first-of-its-kind phase III clinical trial comparing the two technologies. Findings of the PARTIQoL trial will be presented today at the American Society for Radiation Oncology (ASTRO) Annual Meeting.
“We tested two contemporary, advanced forms of external beam radiation for a very common cancer, and we demonstrated that both are very safe, effective treatments that give patients excellent outcomes in terms of quality of life and cancer control,” said Jason Efstathiou, MD, PhD, FASTRO, principal investigator of the trial and vice chair of faculty and academic affairs in the department of radiation oncology at Massachusetts General Hospital.
Patients diagnosed with localized prostate cancer, in which the cancer has not spread outside the prostate and may grow slowly, have many treatment options. About 70% of new prostate cancer cases-more than 200,000 people in the U.S. each year-are diagnosed as localized disease. And since many of these patients will survive their cancer and live many years after treatment, their quality of life becomes particularly paramount when making treatment decisions, Dr. Efstathiou said.
External beam radiation therapy is a common option for patients with localized prostate cancer. Most types of this therapy use photon beams, the same radiation used in lower doses for x-rays. Photon beams can reach tumors deep inside the body but scatter bits of radiation along the way, which can lead to side effects in the area treated. IMRT, for example, is an advanced form of photon-based radiation that allows oncologists to shape and modulate the radiation beams to conform to the three-dimensional shape of a tumor.
Another external-beam option-proton therapy-uses protons rather than photon beams. These charged particles kill cancer by producing a sudden burst of energy once they stop inside a tumor. Because this release happens directly at the tumor site, protons deliver less radiation along their path and are potentially less likely to harm surrounding healthy tissue. This increased precision also comes with significantly higher costs, however. The specialized equipment and facilities required for proton therapy are less widely available than those for IMRT and the treatment can be substantially more expensive.
“Patients now have many options for how they might manage their prostate cancer, but trying to sift through all of the information to understand the consequences for their quality of life can be confusing,” said Dr. Efstathiou, who is also professor of radiation oncology at Harvard Medical School. “To aid them in making these decisions, we compared two of the most advanced forms of external beam radiation, IMRT and proton beam therapy, head-to-head.”
Between June 2012 and November 2021, Dr. Efstathiou and his colleagues randomly assigned 450 patients with low- or intermediate-risk localized prostate cancer enrolled from 29 recruiting centers to receive either proton therapy or IMRT, without hormonal therapy. The median age was 68 years old. Patients were asked to self-report bowel, urinary and sexual functions via questionnaires at baseline and at multiple timepoints after treatment; median follow-up was 60.3 months.
No differences were observed between the IMRT and proton arms for any of the quality of life domains at any timepoint, and patients treated with either technique reported only small, clinically non-meaningful declines from baseline levels. For example, patients reported average bowel function scores of 93.7 (IMRT) and 93.5 (protons) out of 100 at baseline; after two years, the averages were 91.8 and 91.9, respectively, for a decrease of roughly 2% for each arm (p=0.836).
The groups also did not differ in progression-free survival. Five years after treatment, 93.7% and 93.4% of patients treated with IMRT and protons, respectively, had not experienced tumor progression (p=0.706).
“We can use either of these tools with comparably excellent outcomes,” Dr. Efstathiou said. “There have been so many advances in the delivery of contemporary radiation-such as the incorporation of scanned and modulated beams and in-room imaging-that I think the potential gaps between these technologies have narrowed over time.”
There also were no sustained differences in quality of life or survival between the arms for any pre-defined subgroups: low vs. intermediate risk disease, older vs. younger than 65, yes vs. no rectal spacer use and shortened vs. conventional fractionation schedule. Dr. Efstathiou explained that analyses are continuing on this large dataset, however.
“There may be subgroups that benefit from one technology over another, and we’re actively continuing analyses of that,” he said, noting that the study only compared the efficacy of each technology for patients with localized prostate cancer and not more advanced stages of the disease.
Dr. Efstathiou said the completion of this trial is also a win for the field, which relies on advanced technologies that can be difficult to assess in a randomized controlled trial.
“Providing the best evidence-based care calls for rigorously testing the tools we use for that care. We commonly use randomized controlled trials to evaluate new drugs, for example, but not necessarily for new technologies,” he said. “I hope that our work shows that randomized, controlled trials are critical in technology assessment.”
Reference:
IMRT and proton therapy offer equally high quality of life and tumor control for people with prostate cancer, American Society for Radiation Oncology,Meeting American Society for Radiation Oncology (ASTRO) 2024 Annual Meeting.
Powered by WPeMatico
Gynaecologic malignancies contribute significantly to morbidity and mortality with more than half of the cost is associated with hospital stays for diagnosis and treatment. Recent study aimed to identify novel risk factors for conversion from minimally invasive to open surgeries for gynecologic oncology operations. The researchers conducted a retrospective cohort study of 1,356 patients who underwent surgeries for gynecologic masses or malignancies between 2015-2020 at a single academic medical center. The key findings of the study were: 1. Overall conversion rate from minimally invasive to open surgery was 6.1% (43/704 cases). 2. Patients who required conversion had significantly lower preoperative hemoglobin levels compared to minimally invasive and open surgery cases (11.6 ± 1.9 vs 12.8 ± 1.5 vs 11.8 ± 1.9 g/dL, p<.001). 3. Patients with preoperative hemoglobin <10 g/dL had an adjusted odds ratio of 3.94 for conversion, while patients with BMI ≥30 kg/m2 had an adjusted odds ratio of 2.86 for conversion. 4. A risk prediction model incorporating age >50 years, BMI ≥30 kg/m2, ASA status >2, and preoperative hemoglobin <10 g/dL had an AUROC of 0.71, indicating good discriminatory ability. Patients with 2 or more risk factors had a 12% conversion rate.
Novel Findings
The novel finding of lower preoperative hemoglobin as a significant risk factor for conversion provides important insights. Lower hemoglobin may signal greater disease burden and extent of adhesions, leading to increased conversion risk. Incorporating this variable into a risk prediction model can help surgical teams better anticipate conversion, allowing for improved preoperative planning and patient counseling. This can ultimately improve outcomes for patients undergoing minimally invasive gynecologic oncology procedures.
Key Points
Here are the 6 key points from the research paper: 1. The overall conversion rate from minimally invasive to open surgery was 6.1% (43/704 cases). 2. Patients who required conversion had significantly lower preoperative hemoglobin levels compared to minimally invasive and open surgery cases (11.6 ± 1.9 vs 12.8 ± 1.5 vs 11.8 ± 1.9 g/dL, p<.001). 3. Patients with preoperative hemoglobin <10 g/dL had an adjusted odds ratio of 3.94 for conversion, while patients with BMI ≥30 kg/m2 had an adjusted odds ratio of 2.86 for conversion. 4. A risk prediction model incorporating age >50 years, BMI ≥30 kg/m2, ASA status >2, and preoperative hemoglobin <10 g/dL had an AUROC of 0.71, indicating good discriminatory ability. Patients with 2 or more risk factors had a 12% conversion rate. 5. The novel finding of lower preoperative hemoglobin as a significant risk factor for conversion provides important insights, as lower hemoglobin may signal greater disease burden and extent of adhesions, leading to increased conversion risk. 6. Incorporating the preoperative hemoglobin variable into a risk prediction model can help surgical teams better anticipate conversion, allowing for improved preoperative planning and patient counseling, ultimately improving outcomes for patients undergoing minimally invasive gynecologic oncology procedures.
Reference –
Kevin H. Nguyen, Hyundeok Joo, Solmaz Manuel, Lee-may Chen & Lee-
lynn Chen (2024) Incorporating low haemoglobin into a risk prediction model for conversion in minimally invasive gynaecologic oncology surgeries, Journal of Obstetrics and Gynaecology,
44:1, 2349960, DOI: 10.1080/01443615.2024.2349960
Powered by WPeMatico

Remote video consultations between patients and mental health specialists show a small but significant improvement on symptoms of depression and anxiety, finds a trial published by The BMJ today.
Although the effect size is small, the researchers say the effect is still meaningful given the high levels of these disorders in the community.
Globally, depression and anxiety disorders are among the top leading causes of years lived with disability, but most people with depression and anxiety are treated in primary care and don’t have access to specialised mental health care.
Previous studies have shown that telemedicine in primary care settings can be effective, but evidence is scarce for remote consultations between patients in primary care settings and offsite mental health specialists.
To explore this further, researchers in Germany investigated the effectiveness of a new mental health video consultation model (PROVIDE) for treating people with symptoms of depression and anxiety in primary care settings.
Their findings are based on 376 adults (average age 45 years; 63% women) who visited their general practitioner (GP) with at least moderately severe depression or anxiety, or both, between 24 March 2020 and 23 November 2021.
Severity of symptoms was measured using the patient health questionnaire anxiety and depression scale (PHQ-ADS) and participants were randomly assigned to receive the PROVIDE model or usual care.
The PROVIDE model comprised five 50-minute real-time video sessions featuring brief psychotherapy over eight weeks between the patient at the primary care practice and a mental health specialist at an offsite location. Usual care was provided by a GP and included brief counselling, medication, and referral to specialists.
Compared with usual care, the PROVIDE intervention led to small improvements in the severity of depressive and anxiety symptoms (average 2.4 point reduction on the PHQ-ADS score) at six months, and effects were sustained at 12 months (average 2.9 point reduction).
The PROVIDE model was also more effective in reducing psychological distress related to physical (somatic) symptoms, at both six and 12 months, but did not seem to offer any additional benefit for recovery.
No serious adverse events were reported in either group.
The researchers point to several limitations, such as the difficulties of meeting a fully representative and unbiased sample in practice based clinical research and the potential impact of missing data.
And although the effect size is small (below the average minimal clinically important difference of 3-5 points on the PHQ-ADS score), they argue that the improvement is still meaningful “given the high prevalence of depression and anxiety in community settings.”
While further research is needed to help tailor interventions more effectively and maximise their public health impacts, they conclude: “The PROVIDE model shows promise as a scalable intervention that can collectively benefit population health in terms of depression and anxiety disorders.”
Reference:
Haun M W, Tönnies J, Hartmann M, Wildenauer A, Wensing M, Szecsenyi J et al. Model of integrated mental health video consultations for people with depression or anxiety in primary care (PROVIDE-C): assessor masked, multicentre, randomised controlled trial BMJ 2024; 386 :e079921 doi:10.1136/bmj-2024-079921
Powered by WPeMatico

According to research, the ophthalmic solution of phentolamine 0.75% (RYZUMVI™), developed by Ocuphire Pharma, strongly and quickly reverses pharmacologically induced mydriasis with results from the pivotal MIRA-2 and MIRA-3 trials.
Mydriasis, or pharmacologically-induced dilation of the pupils, lasts for up to 24 hours and causes some side effects to include photophobia and blurred vision that can interfere with activities on a day-to-day basis. Developing phentolamine ophthalmic solution 0.75% serves to fill the gap that brings the patient out of the comfort zone much sooner than mydriasis, once again after examination and diagnostic procedures by an eye care specialist.
MIRA-2 and MIRA-3 were Phase 3, two randomized, double-masked, placebo-controlled, multi-center studies designed to evaluate the efficacy and safety of phentolamine ophthalmic solution 0.75% in reversing pharmacologically induced mydriasis. In total, 553 healthy subjects aged between 12 and 80 years enrolled for the study that included subjects who received the assigned, blinded treatment at randomization with either the phentolamine solution or placebo after the pupils had been pharmacologically dilated.
Phentolamine ophthalmic solution 0.75% was significantly better than placebo at terminating mydriasis, according to the results of achieving two of the major endpoints of the studies.
In MIRA-2, pupil diameter reversal within 90 minutes was seen in 48.9% of patients in the phentolamine solution arm compared with 6.6% in the placebo group (P < 0.0001).
In MIRA-3, 58% of patients in the phentolamine arm had pupil reversal at 90 minutes compared with 6% in the placebo arm (P < 0.0001).
Both studies showed the reversal of early mydriasis
MIRA-2: At 60 minutes, 24.5% of patients in the phentolamine-treated group showed reversal compared with only 5.5% in the placebo group (P < 0.0003).
MIRA-3: At 60 minutes, 42% of patients in the phentolamine-treated group showed reversal compared with only 2% in the placebo group (P < 0.0001).
At 24 hours post-dilation, only 8-11% of patients in the phentolamine-treated group had residual dilation compared with 28-34% in the placebo group (P < 0.0001).
Phentolamine ophthalmic solution 0.75% reverses pharmacologically induced mydriasis within 60 to 90 minutes with faster recovery from dilation compared with placebo, and is seen to be well-tolerated. These results, as reported in MIRA-2 and MIRA-3, may provide an additional treatment for the patient who needs more rapid resolution of visual disturbances from mydriasis. Substantially effective with FDA approval, phentolamine could soon improve the quality of ophthalmology care.
Reference:
Pepose JS, Wirta D, Evans D, et al. Reversal of Pharmacologically Induced Mydriasis with Phentolamine Ophthalmic Solution. Ophthalmology. Published online September 16, 2024. doi:10.1016/j.ophtha.2024.09.010
Powered by WPeMatico
