Tailoring Pain Management: Study Sheds Light on Enhancing Living Liver Donor Outcomes Through Innovative Analgesia
HEADING: Tailoring Pain Management: Study Sheds Light on Enhancing Living Liver Donor Outcomes Through Innovative Analgesia
India: A recent review published online in Apollo Medicine has shed light on the evolving strategies for pain management in living liver donors undergoing hepatectomy.
The review emphasizes the need for tailored analgesic approaches that consider individual patient characteristics and requirements. It highlights the potential advantages of adopting innovative methods to improve pain management, decrease opioid use, and ultimately enhance outcomes and satisfaction for living liver donors undergoing hepatectomy.
Speaking on the study’s relevance in the current medical landscape, the lead author, Dr. Ashish Malik, the Department of Anaesthesia and Critical Care at Indraprastha Apollo Hospital in New Delhi, India, shared his insights with Medical Dialogues:
“Donor analgesia has been of paramount importance for the development of the living donor liver transplant program, serving as the cornerstone for motivating donation. Multiple methods for providing pain relief have been adopted. This article contributes to discussing the merits and demerits of various techniques and explores how a multimodal approach can be formulated to ensure donor safety.
Dr. Malik also highlighted the unique aspects of the study, stating, “This review article provides in-depth knowledge about all available methods for donor analgesia, based on which a blended approach can be formulated.” His insights emphasize the comprehensive nature of the research, which aims to enhance pain management strategies for living liver donors.
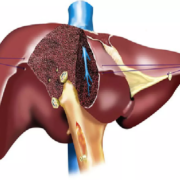
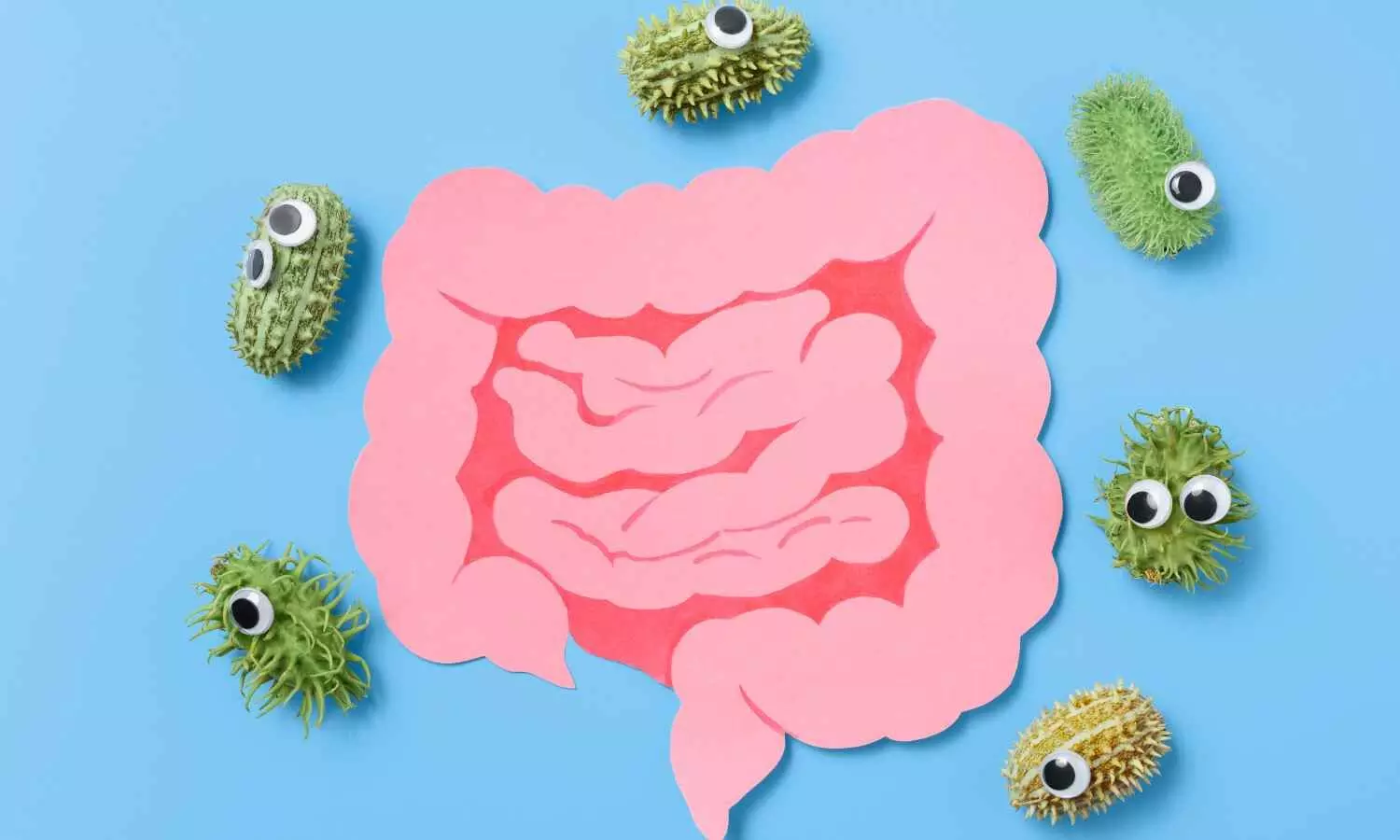
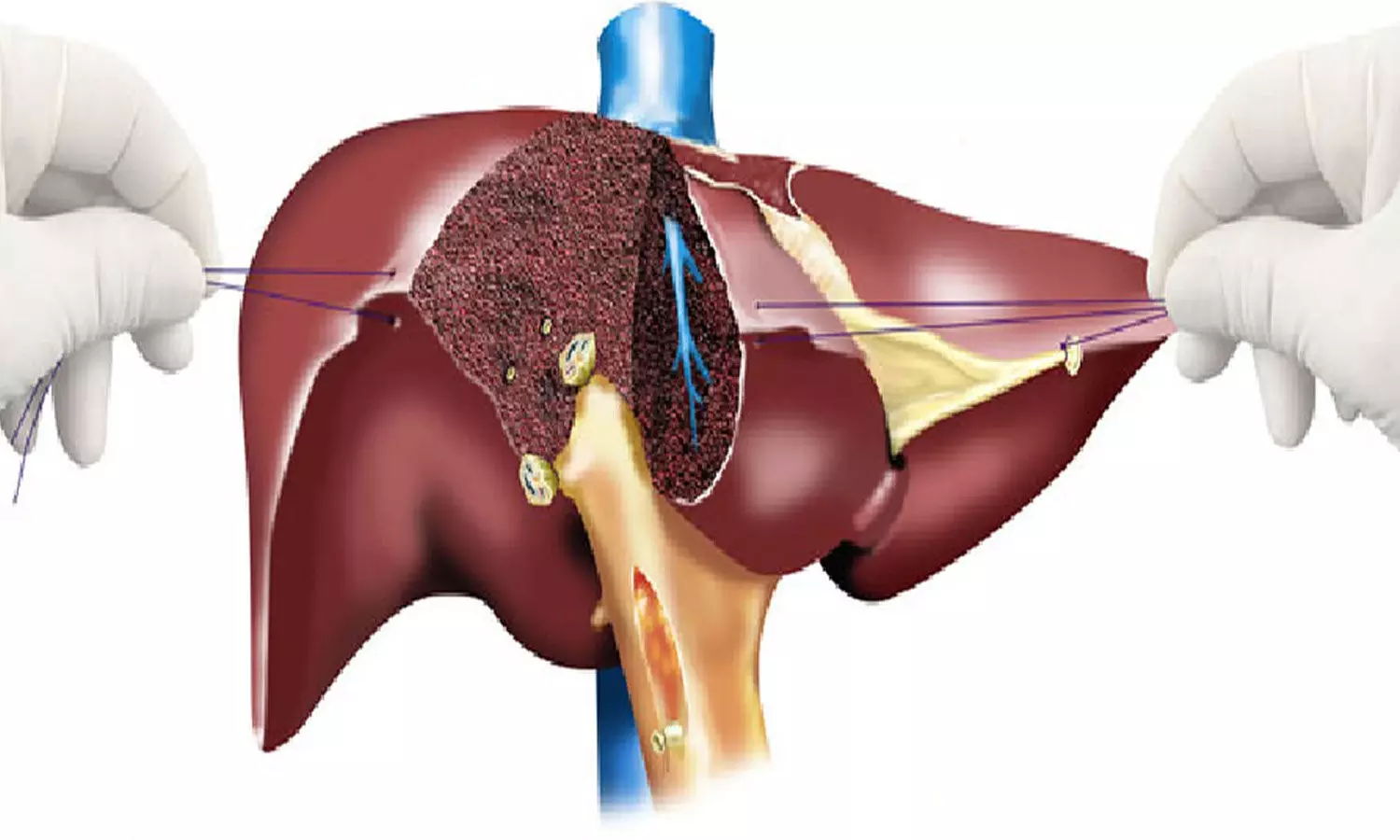
The study authors note that donor hepatectomy is a complex surgical procedure that often leads to considerable postoperative pain, affecting both short-term recovery and long-term outcomes. Effective pain management is essential for the well-being of living liver donors and for optimizing their overall experience. The review by Dr. Malik and the team seeks to offer a thorough overview of current practices and emerging strategies in analgesic management for donor hepatectomy.
For this purpose, the team conducted searches on PubMed and Google Scholar to identify relevant materials. Their evaluation included review articles, clinical trials, retrospective studies, observational studies, and case-control studies. The review explores recent advancements in pain management, including enhanced recovery after surgery protocols, personalized analgesic regimens, and innovative pharmaceutical agents. Additionally, it examines the role of psychological factors and patient-centered care in shaping postoperative pain experiences.
The review revealed the following findings:
- The traditional approach to pain management employs a multimodal strategy that combines opioids, non-steroidal anti-inflammatory drugs, and regional anesthesia techniques.
- Concerns about opioid-related side effects and potential complications have led to a re-evaluation of analgesic protocols.
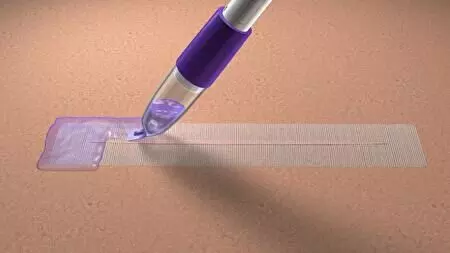
- Alternative methods, such as thoracic epidural analgesia, transversus abdominis plane blocks, and continuous wound infusion systems, are gaining attention for their ability to reduce opioid use and improve recovery outcomes.
Dr. Malik highlighted the implications and key findings of the review, stating that the article aims to enhance recovery after surgery by establishing a standardized approach to pain management. He emphasized the significance of regional anesthesia techniques and the use of novel pharmaceutical agents such as magnesium, dexmedetomidine, gabapentin, and ketamine, all of which can help reduce opioid consumption during these procedures. As surgical methods evolve from open donor hepatectomies to laparoscopic and robotic techniques, these strategies are becoming increasingly relevant.
However, Dr. Malik noted that there is still limited research data in the field of donor analgesia. Randomized controlled trials involving large patient populations are necessary to determine the most effective techniques for managing donor pain. He stressed the importance of focusing future research on acute and chronic pain scores in living donors, as these factors directly influence the quality of life for donors.
Reference:
Malik, A., & Pal, A. (2024). Analgesia for Donor Hepatectomy: Recent Perspectives. Apollo Medicine.https://doi.org/10.1177/09760016241248310
Powered by WPeMatico