Increased mortality and complication rates observed in women following TAVR, suggests study
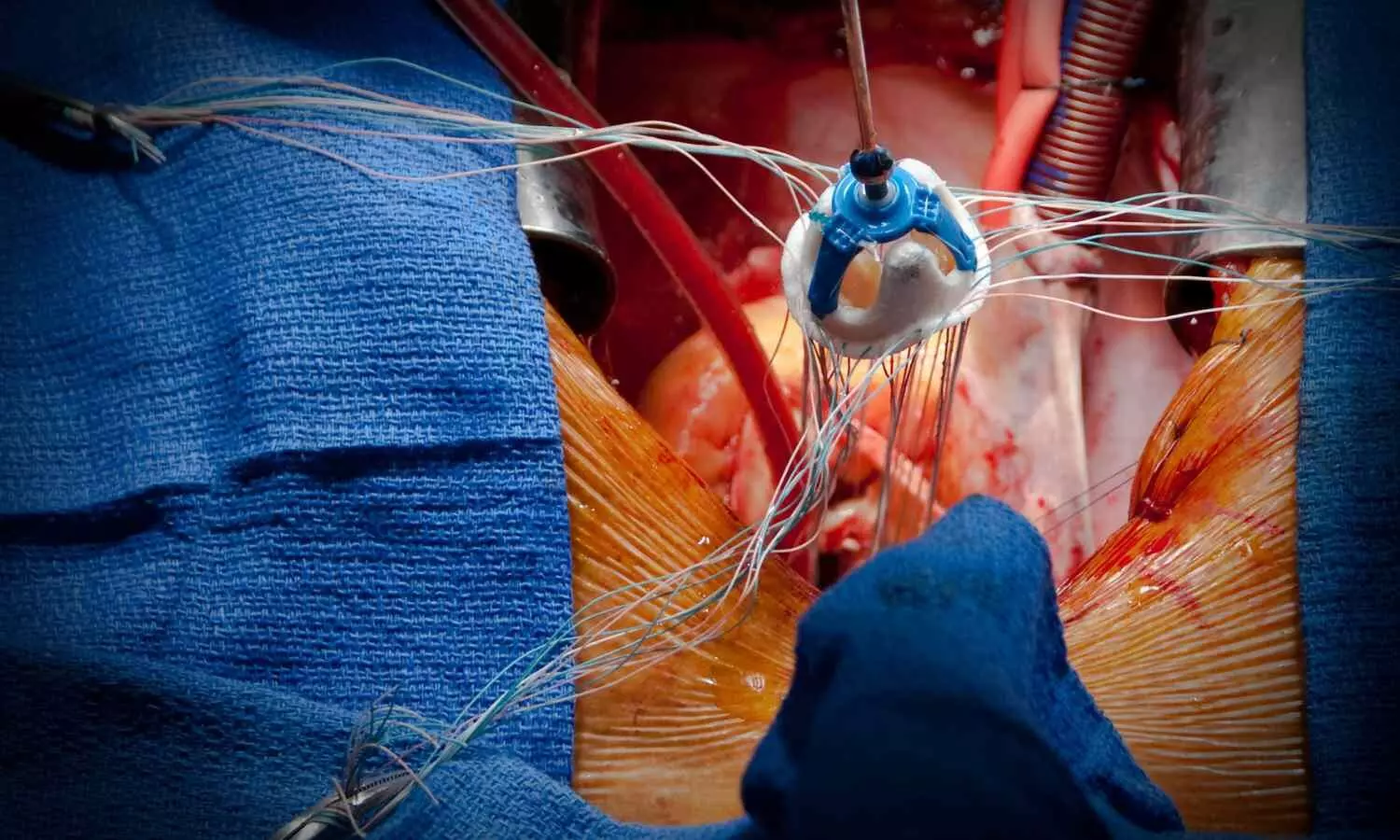
A new study published in the International Journal of Cardiology showed that regardless of sex, there are still prominent differences in Transcatheter Aortic Valve Implantation (TAVI) outcomes. TAVR offers helpful therapeutic choices to individuals who would not have been considered for valve replacement, despite the fact that it is not risk-free. In terms of recuperation, the experience of a person with a TAVR operation can resemble that of a coronary angiography. The treatment of severe aortic stenosis (AS) has been transformed by transcatheter aortic valve implantation, yet, it is still unknown how sex difference affects TAVI results. Thereby, Manoj Kumar and his colleagues looked at how post-procedural outcomes of TAVI, such as readmission rates and healthcare burden, differed for men and women.
To find hospitalizations for TAVI, the Nationwide Readmissions Database (2016–2020) was utilized. Males and females were matched using a propensity score matching (PSM) algorithm. Pearson’s chi-squared test was employed to analyze the results. A total of 1,42,054 (44.3%) of the 3,20,324 TAVI hospitalizations involved surgical procedures on the female patients.
In-hospital mortality, stroke, post-procedural hemorrhage, vascular complications, acute respiratory failure (ARF), pericardial complications, transfusion requirement, vasopressor need, and major adverse cardiac and cerebrovascular events (MACCE) were all greater among women after propensity matching.
Acute kidney damage (AKI), sudden cardiac arrest (SCA), cardiogenic shock, and the need for mechanical circulatory support (MCS) were all considerably less common in women. At 30 and 90 days, readmission rates were greater for males than for women. Following TAVI, there was no discernible difference in the 180-day readmission rates for men and women. Also, procedure-related mortality declined for both sexes and hospitalization expenses and recuperation durations fell between 2016 and 2020.
Overall, men experienced greater rates of readmission, cardiogenic shock, AKI, and the requirement for mechanical circulatory support, whereas women saw higher rates of death and post-procedural complications. Despite improvements in procedure-related mortality and TAVI resource utilization from 2016 to 2020, regardless of sex, the results of this show notable differences in TAVI outcomes.
Reference:
Kumar, M., Hu, J.-R., Ali, S., Khlidj, Y., Upreti, P., Ati, L., Kumar, S., Shaka, H., Zheng, S., Bae, J. Y., Alraies, M. C., Mba, B., Yadav, N., Vora, A. N., & Davila, C. D. (2025). Sex disparities in outcomes of transcatheter aortic valve implantation- a multi-year propensity-matched nationwide study. In International Journal of Cardiology (Vol. 418, p. 132619). Elsevier BV. https://doi.org/10.1016/j.ijcard.2024.132619
Powered by WPeMatico