Study Recommends Double-J Stent for Enhanced Outcomes in Staghorn Stone Treatment via Percutaneous Nephrolithotomy
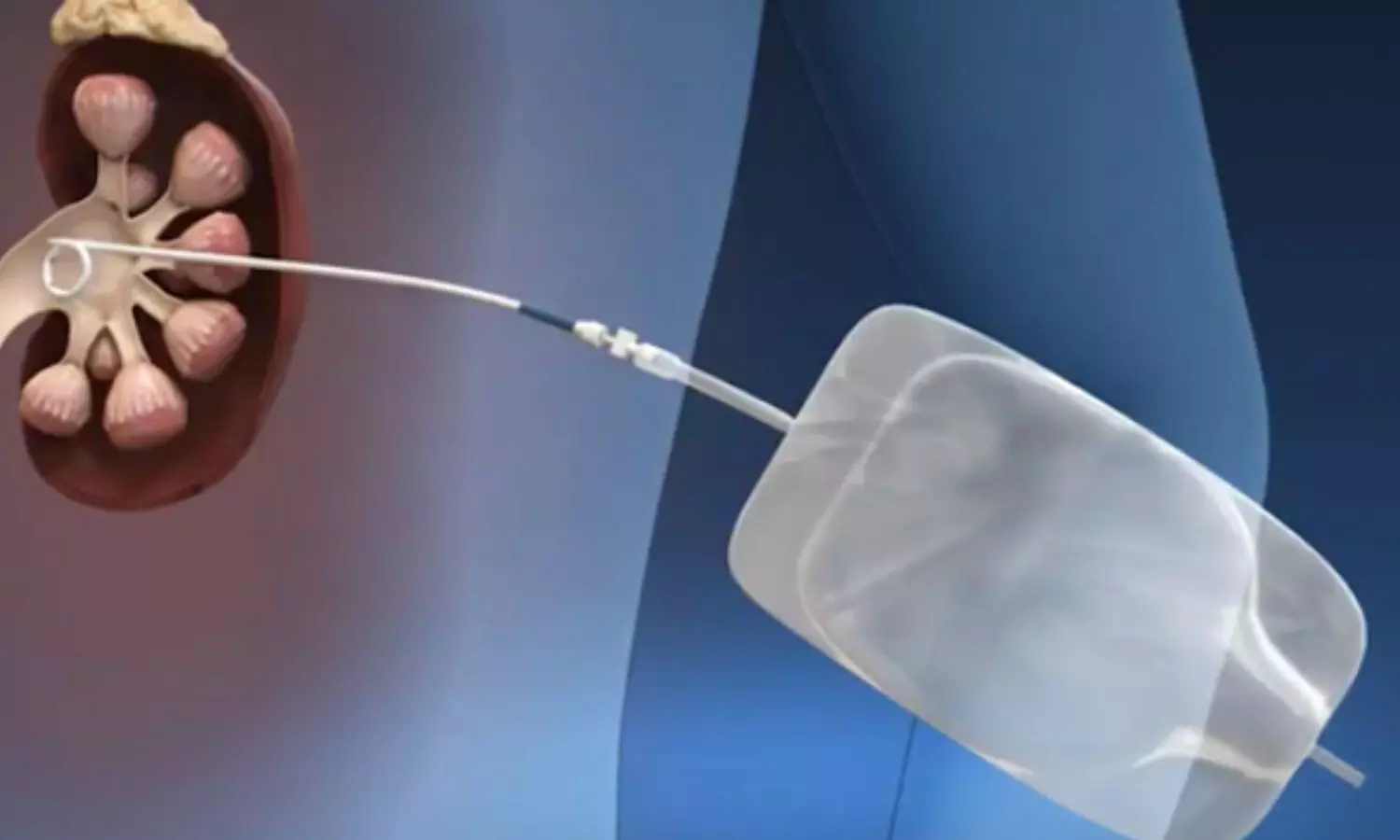
Iran: A recent study published in BMC Urology has raised important questions about the necessity of using a double-J stent (DJ stent) after complete supine percutaneous nephrolithotomy (csPCNL) in adult patients with staghorn renal stones. Staghorn stones are large, branched calculi that can significantly impair kidney function and lead to severe complications if not treated effectively.
The researchers suggest that while omitting a double-J stent after csPCNL can yield acceptable outcomes, the higher residual stone rates associated with staghorn stones lead to increased incidences of renal colic, longer hospital stays, and extended recovery periods. Therefore, they recommend the insertion of a DJ stent.
The research highlights that while csPCNL has become a popular minimally invasive technique for managing these complex stones, postoperative management remains a critical discussion topic. Traditionally, placing a DJ stent following the procedure has been standard practice. The stent maintains urinary drainage, reduces the risk of complications, and adds to patient discomfort and recovery time.
Against the above background, Samira Kazemi, Guilan University of Medical Sciences, Rasht, Iran, and colleagues compared the outcomes of ureteral catheters versus double-J stents in tubeless complete supine PCNL for staghorn stone treatment.
For this purpose, the researchers conducted an analytical cross-sectional study from May 2008 to August 2022, assessing 123 patients who underwent tubeless csPCNL. The patients were categorized into two groups: those who received a double-J (DJ) stent (Group I; n = 23) and those who had a totally tubeless approach using only a perioperative ureteral stent (Group II; n = 100). The study compared demographic characteristics, stone-related factors, and perioperative and postoperative parameters between the two groups.
The following were the key findings of the study:
- Baseline characteristics were similar across both groups. However, the operative time for Group I was significantly longer than for Group II (68.26 versus 55.25 minutes).
- In contrast, the duration of hospitalization was shorter for Group I (1.81 versus 2.37 days).
- The stone-free rate was higher in Group I (90.5% versus 79.8%), although this difference was not statistically significant.
- There were no major complications between the groups.
- Patients in Group II experienced a significantly shorter time to return to normal activities (6.48 versus 7.91 days).
- Multivariable linear regression analysis indicated that preoperative creatinine levels and stone size significantly affect operative time. However, the number of stones and underlying health conditions influenced the length of hospital stay.
“While the necessity of a DJ stent in PCNL for staghorn stones remains debated, its use is advised for these patients due to benefits such as shorter hospital stays, quicker recovery times, and improved success rates,” the researchers concluded.
Reference:
Falahatkar, S., Esmaeili, S., Kazemi, S. et al. Is double-J stent mandatory in complete supine percutaneous nephrolithotomy for adult patients with staghorn renal stones? BMC Urol 24, 216 (2024). https://doi.org/10.1186/s12894-024-01610-9
Powered by WPeMatico