Brain scans reveal action-based organization in people born without hands
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
India: Inhalation therapy remains a cornerstone in the treatment of obstructive, inflammatory, and infectious respiratory diseases, with inhalers often being a physician’s go-to device. However, their effectiveness is frequently compromised due to poor adherence and incorrect usage. Studies show that 30–60% of asthma patients and up to 80% of COPD patients commit at least one critical error while using inhalers. A cross-sectional study also found that 75.36% of patients made errors regardless of inhaler type, leading to poor disease control and increased risk of exacerbations.
In this context, nebulization has emerged as a valuable alternative for delivering bronchodilators and corticosteroids. Despite its clinical relevance, existing nebulization guidelines are lengthy and challenging to use in routine practice.
To address this gap, an expert panel of leading Indian pulmonologists have developed a simplified, evidence-based guidance document titled the NOVA-ER, an Expert’s Review, published in the Medical Research Archives. This document provides practical recommendations for managing Asthma, COPD, Bronchiectasis, and overlapping respiratory conditions, addressing both rescue and maintenance therapies tailored to disease severity.
The panel based their recommendations on an extensive review of recent peer-reviewed literature and clinical guidelines using databases like PubMed, MEDLINE, and the Cochrane Library. Structured discussions among pulmonology experts further refined the guidance.
The NOVA-ER article presents stepwise, disease-specific algorithms (e.g., COPD Treatment algorithm as given below) to support clinicians in selecting appropriate nebulized treatments and highlights the use of nebulizer therapy in suitable candidates, ultimately aiming to improve implementation of nebulization therapy in India’s respiratory care framework.
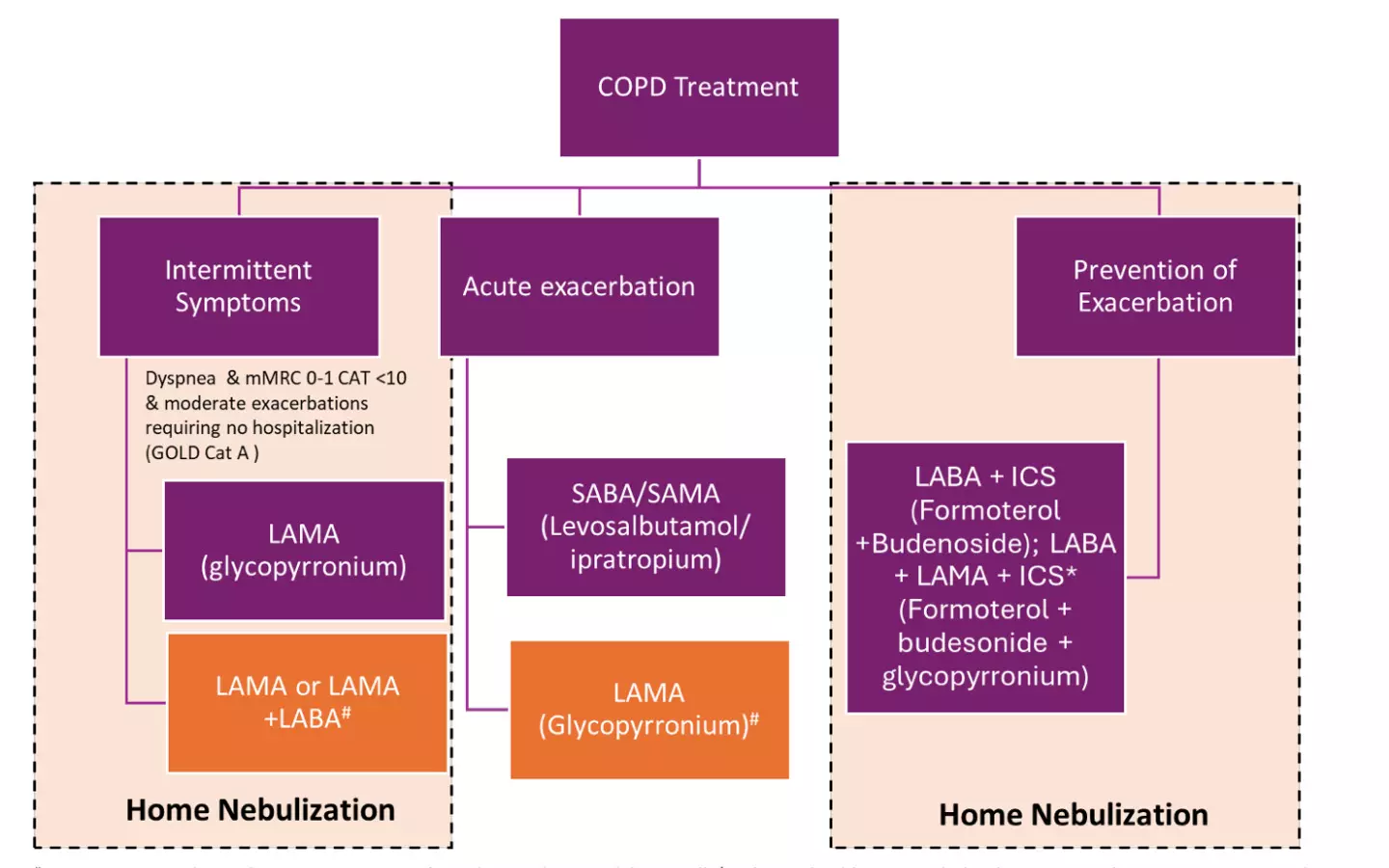
Fig 1: Algorithm for the use of nebulization and advice on home nebulization in COPD
Here are the insights from the consensus:
Experts highlight the importance of thorough patient education. Guiding patients on proper maintenance, cleaning, and disinfection of nebulizers is crucial for ensuring hygiene and effective device performance. In addition, patient counseling is vital for enhancing adherence to prescribed nebulizer therapy, which supports consistent medication use and helps achieve better long-term health outcomes.
Reference: Dhar, R., Mukhopadhyay, A., et al., 2025. Nebulization Optimization for Management of Obstructive Airway Disorders: An Expert Review (NOVA-ER). Medical Research Archives, [online]13(4).https://doi.org/10.18103/mra.v13i4.6377
Powered by WPeMatico

Thiruvananthapuram: A controversy has erupted after the Head of the Nephrology Department at Thiruvananthapuram Medical College Hospital (MCH) publicly criticised Kerala’s post-mortem organ donation programme, the Kerala Network for Organ Sharing (KNOS/K-SOTTO), calling it a “complete failure.”
In a social media post mourning the death of former nephrology head Dr Venugopal, the present HoD Dr Mohan Das said that the project had lost its success after the passing of Dr Ramdas, who played a key role in building the Mrithasanjeevani (K-SOTTO) initiative.
“It was Dr Venugopal and Dr Ramdas who made the Mrithasanjeevani project in Kerala a success. With the death of Dr Ramdas, Mrithasanjeevani has become a total failure,” he said in the post.
Also read- 3rd year female MD Medicine medico attacked by patient kin at Thiruvananthapuram Medical College
He also pointed out that not even a single cadaver transplant had taken place at Alappuzha Medical College, despite it being the base of the K-SOTTO executive director. However, Das later deleted the post.
Responding to the criticism, the Principal of Thiruvananthapuram Medical College, Dr PK Jabbar, issued a strict directive to doctors, barring them from making public statements. He warned of strict disciplinary action against violations of service rules, reports Onmanorama.
The criticism came almost two months after Dr Haris Chirakal publicly disclosed the shortage of surgical equipment and delays in surgeries at the state-run Thiruvananthapuram Medical College Hospital.
Medical Dialogues had previously reported that a social media post by a leading senior urologist disclosing a shortage of surgical equipment and delays in surgeries for months at the state-run Thiruvananthapuram Medical College Hospital has gained widespread attention and landed him in an open fight against the health department, all for the sake of his patients.
Dr Haris Chirakkal, Head of the Urology Department at Thiruvananthapuram Medical College Hospital, shared a detailed Facebook post, which is now deleted, where he highlighted the grim situation at the hospital as he could no longer stay silent as a doctor. Although Dr Chirakkal agreed to delete his Facebook post at the DME’s request, he later told reporters that the issues he raised persist.
In his post, he expressed his frustration after repeated delays in surgeries due to a lack of basic medical equipment. He pointed out that doctors are left helpless as patients wait for critical surgeries for months, only to have them cancelled due to the unavailability of essential medical equipment. As a result, poor patients and their families are left confused and hopeless, not knowing what to do next, he added.
Powered by WPeMatico

A new study published in the Journal of American Medical Association showed that although it did not decrease the incidence of new loop diuretic introduction in patients who were not on them at baseline, finerenone’s safety and effectiveness were constant across all diuretic subgroups, lowering total diuretic usage in patients with heart failure with mildly reduced or preserved ejection fraction (HFmrEF/HFpEF).
The effectiveness and safety of mineralocorticoid receptor antagonists in combination with other diuretics, as well as whether they have a so-called diuretic-sparing effect in patients with heart failure (HF), should be assessed due to their renal effects.
Thereby, to investigate the effectiveness and tolerance of finerenone in conjunction with background diuretic medication in patients with HFmrEF/HFpEF, this research was carried out.
This study is a predetermined secondary analysis of the FINEARTS-HF randomly assigned clinical trial, which was carried out among adults 40 years of age and older with HFmrEF/HFpEF across 653 sites in 37 countries. The trial was randomized between September 2020 and January 2023. Analysis of the data took place between December 1, 2024, and January 30, 2025.
The composite of all heart attacks and cardiovascular deaths was the main result. Results were compared between finerenone and placebo based on the following baseline diuretic categories: loop diuretic (≤40 mg vs. >40 mg dosage of furosemide equivalent); solely nonloop diuretic (thiazide or thiazide-like); and combination non-loop and loop diuretic treatment.
Of the 5,438 patients, the mean (SD) age was 72.1 (9.6) years, and 2496 (45.9%) were female. In all, 684 patients (12.6%) were using a nonloop diuretic, 3040 patients (55.7%) were taking less than or equal to 40 mg of furosemide equivalent, 1145 patients (21.1%) were taking 40 mg or more, and 569 patients (10.5%) were taking both nonloop and loop diuretics.
In all diuretic subgroups, finerenone decreased the risk of the primary end point when compared to placebo: rate ratios for patients in the nonloop, 40 mg or less loop, more than 40 mg loop, and combined nonloop and loop categories were 0.84 (95% CI, 0.47-1.51), 0.86 (95% CI, 0.72-1.02), 0.98 (95% CI, 0.78-1.24), and 0.54 (95% CI, 0.35-0.83), respectively.
Finerenone decreased loop diuretic dosage and dose intensification but not loop diuretic beginning when compared to a placebo. The safety of each diuretic category was the same.
Overall, all diuretic subgroups benefited equally on finerenone. Finerenone decreased the requirement for loop diuretic dosage intensification and decreased the mean loop diuretic dose, but it did not substantially lower the introduction of a loop diuretic in patients who were not receiving loop diuretics at baseline when compared to placebo.
Source:
Chimura, M., Jhund, P. S., Henderson, A. D., Yang, M., Claggett, B. L., Desai, A. S., Rohwedder, K., Lage, A., Scalise, A., Mueller, K., Schou, M., Lam, C. S. P., Senni, M., Voors, A. A., Zannad, F., Pitt, B., Vaduganathan, M., Solomon, S. D., & McMurray, J. J. V. (2025). Efficacy and tolerability of finerenone according to the use and dosage of diuretics: A prespecified analysis of the FINEARTS-HF randomized clinical trial. JAMA Cardiology. https://doi.org/10.1001/jamacardio.2025.2551
Powered by WPeMatico

Denmark: Women diagnosed with gestational diabetes mellitus (GDM) often share significant cardiometabolic health risks with their partners, highlighting an opportunity for couple-based preventive strategies, according to a recent study published in Diabetes, Obesity and Metabolism.
The research led by Majken Lillholm Pico, MSc, from the Department of Prevention, Health Promotion and Community Care at Copenhagen University Hospital – Steno Diabetes Center Copenhagen, assessed 196 couples 12 weeks after a GDM-affected pregnancy. Health examinations and questionnaires evaluated overweight or obesity, waist circumference, metabolic syndrome, impaired fasting glucose, stage 1 or higher hypertension, as well as dietary quality and physical activity.
The study led to the following findings:
The authors noted that detecting GDM could serve as an early warning sign for identifying partners at risk, paving the way for family-focused interventions targeting diet, exercise, and weight control.
However, several limitations were acknowledged. The cross-sectional design restricts conclusions about causality, and the timing—just 12 weeks postpartum—may overestimate overweight prevalence in women. Lifestyle behaviours at this stage may also not reflect long-term patterns. Furthermore, the cut-offs used for overweight, obesity, and waist circumference were based on European standards, potentially misclassifying participants of non-European origin (around 10% of the sample).
The researchers also pointed out that physical activity measures might have been overestimated due to the questionnaire method, and the absence of a comparison group without GDM made it difficult to determine whether these risks are unique to such couples. Additionally, couples participating in the study tended to have more favourable socioeconomic profiles, which may limit generalizability.
Despite these constraints, the findings highlight the need for couple-oriented prevention strategies in the aftermath of GDM. “The high prevalence and concordance of cardiometabolic markers suggest that interventions involving both partners could amplify health benefits,” the authors noted. Such approaches, integrated into broader diabetes prevention programs, could support early risk detection and sustained lifestyle improvements.
“Further research is warranted to determine how effectively couple-based programs can reduce cardiometabolic risks in families affected by GDM and improve long-term health outcomes for both partners,” they concluded.
Reference:
Pico ML, Maindal HT, Grunnet LG, Damm P, Jensen DM, Ovesen P, Dahl-Petersen IK, Vinter CA, Kampmann U, Mathiesen ER, Nielsen KK; Face‐it Study Group. Prevalence and concordance of cardiometabolic risk markers and health behaviour among couples after a gestational diabetes mellitus-affected pregnancy. Diabetes Obes Metab. 2025 Aug 8. doi: 10.1111/dom.70017. Epub ahead of print. PMID: 40776803.
Powered by WPeMatico

A prospective cohort study examined the associations of different physical activity patterns with all-cause, cardiovascular (CV) and cancer mortality among adults with diabetes. The study found that weekend warrior and regular activity patterns meeting current physical activity recommendations were associated with similarly reduced risks for all-cause and cardiovascular mortality compared to physical inactivity, demonstrating the importance of any physical activity for people with diabetes. The results are published in Annals of Internal Medicine.
Researchers from Harvard T.H. Chan School of Public Health, Boston University School of Public Health, Vanderbilt University Medical Center, Capital Medical University, and colleagues studied data from 51,650 adults with self-reported diabetes who participated in the National Health Interview Survey (NHIS) between 1997 and 2018. Current guidelines recommend at least 150 minutes per week of moderate-to-vigorous physical activity (MVPA) distributed across a minimum of three days.
Participants were categorized into four activity patterns: inactive (no reported MVPA); insufficiently active (MVPA less than 150 minutes per week); weekend warrior (MVPA 150 or more minutes per week across one to two sessions); and regularly active (MVPA 150 or more minutes per week across at least three sessions).
The researchers found that insufficiently active, weekend warrior, and regularly active participants had lower risks for all-cause and cardiovascular mortality compared to inactive participants. Weekend warriors and regularly active participants had a 21% and 17% lower all-cause mortality risk and 33% and 19% lower risks of cardiovascular mortality, respectively, compared with inactive participants. There were fewer differences by cancer mortality compared with physical inactivity.
Reference:
Zhiyuan Wu, Association of Weekend Warrior and Other Physical Activity Patterns With Mortality Among Adults With Diabetes: A Cohort Study, Annals of Internal Medicine, https://doi.org/10.7326/ANNALS-25-00640
Powered by WPeMatico
