Musculoskeletal Interventional Radiology: What Every Doctor Should Know – Dr Rajesh Botchu

Interventional radiology (IR) is a cornerstone of modern medicine, touching upon virtually every medical and surgical speciality. It plays a key role in the diagnosis and management of conditions across the breadth of clinical medicine.
Within this wider field, musculoskeletal intervention
utilises image-guided techniques to perform minimally invasive procedures diagnosing
and treating a range of conditions such as tumours, rheumatological conditions,
trauma, degenerative disease, and more.
There are numerous procedures, this
article will provide a taste of the most pertinent procedures to illustrate how
musculoskeletal IR can contribute to patient care across a range of
applications.
The overarching principle of most musculoskeletal IR
procedures is to use imaging to guide a needle to a given area. This can be
done for diagnosis, most commonly with percutaneous imaging-guided biopsy (IGB)
where a needle is introduced through the skin into a lesion under ultrasound or
CT (Computed Tomography) guidance, thereby obtaining tissue samples from
suspicious bone or soft tissue lesions.
Alternatives are either a non-guided
biopsy (suitable only for superficial lesions) or open surgical biopsies (which
are far more invasive). Percutaneous IGB is used mainly for tumours, but also
for infections and inflammatory conditions. Accurate tissue diagnosis is
essential for guiding further management, including surgery or oncologic
treatment.
Therapeutic uses employ the same principles. For
example, image-guided injections of corticosteroids, local anaesthetics,
hyaluronic acid, biologics, and blood products amongst others help pain relief
and inflammation control in chronic conditions like osteoarthritis, tendinitis,
or bursitis.
To do so, the injection is directed towards joints
(intra-articular), tendons, or soft tissue spaces. Ultrasound, fluoroscopy, and
CT are all methods which can be used to guide the needle to the correct site
with each modality having its own strengths.
Although procedures can and are
also performed without imaging by using landmark techniques, deeper sites of
injection or those near vulnerable structures (e.g. nerves and vessels)
necessitate imaging to ensure safe and accurate delivery.
Other curative treatments include the destruction of
tumours (ablation) using needle tips which generate ice balls (cryotherapy) or
heat (radiofrequency ablation).
Symptomatic relief can also provide great
patient benefit by enabling mobilisation, such as introducing cement into
spinal fractures via a needle (vertebroplasty) or blocking pain sensation from
nerves (nerve block).
These are only some examples of the wide range of
procedures seen in musculoskeletal IR. Almost every clinician will encounter
patients who benefit from such procedures and will benefit from an awareness of
the basic principles of using imaging to perform minimally-invasive procedures
to facilitate treatment and diagnosis across a range of conditions.
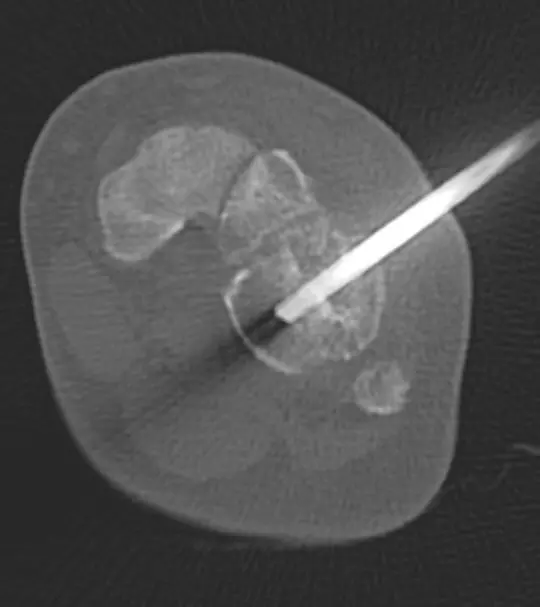
Image showing CT guided bone biopsy of tumour

Images showing radiofrequency ablation of osteoid osteoma of tibia
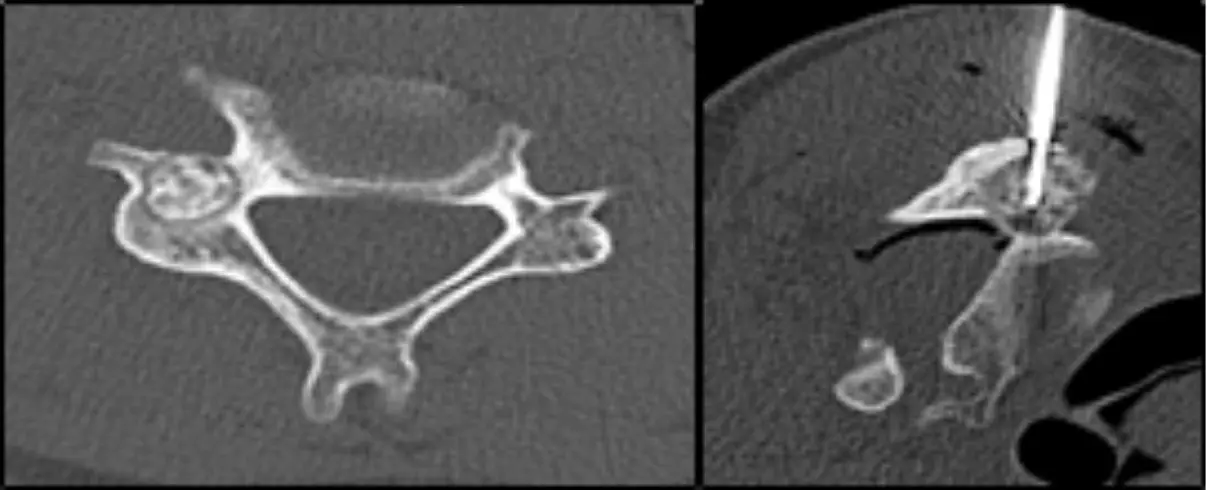
Images showing radiofrequency ablation of osteoid osteoma of cervical spine
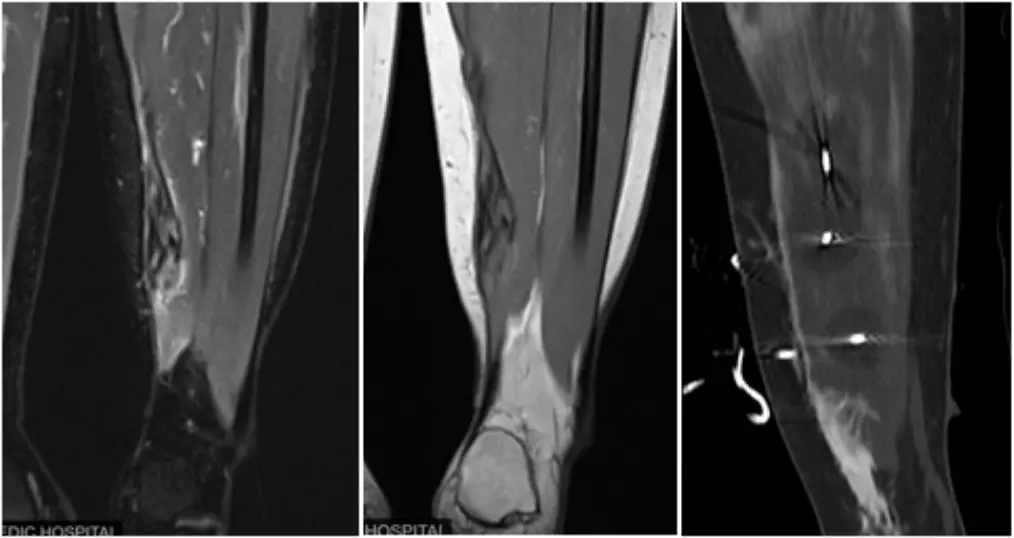
Images showing cryotherapy of fibromatosis
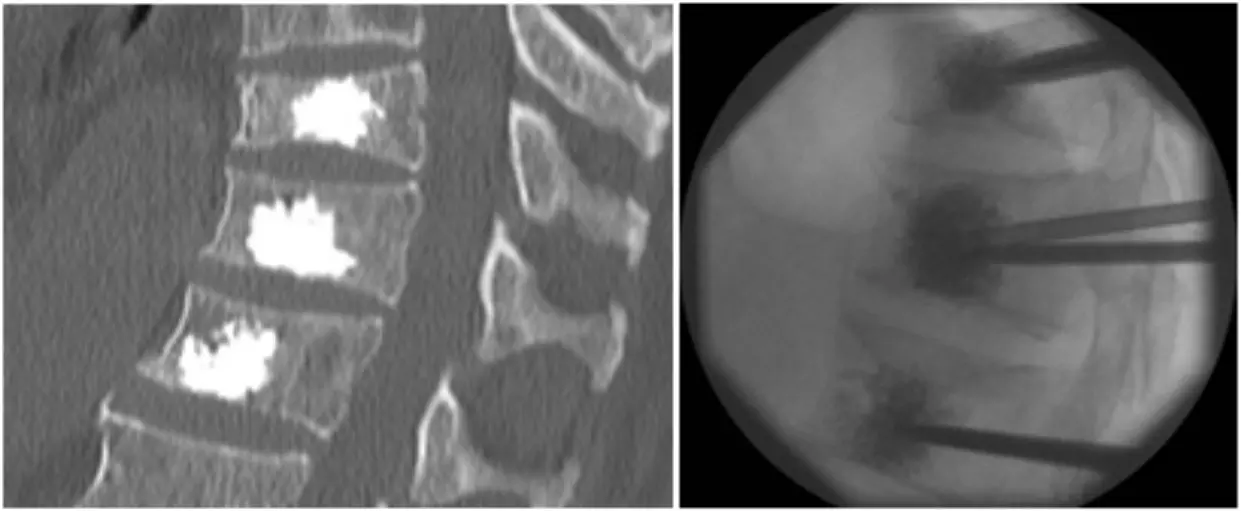
Images showing three level vertebroplasty for osteoporotic fractures
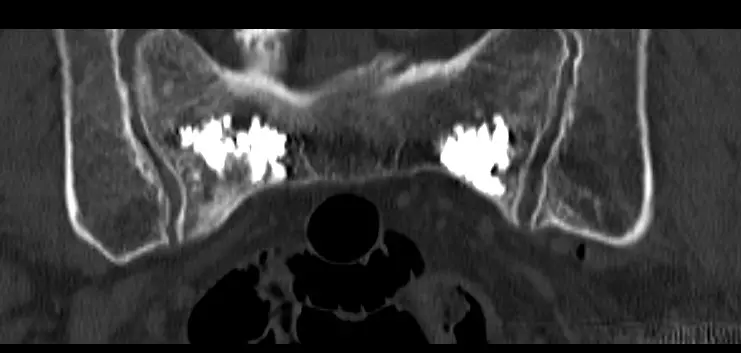
Image showing sacroplasty for osteoporotic fractures
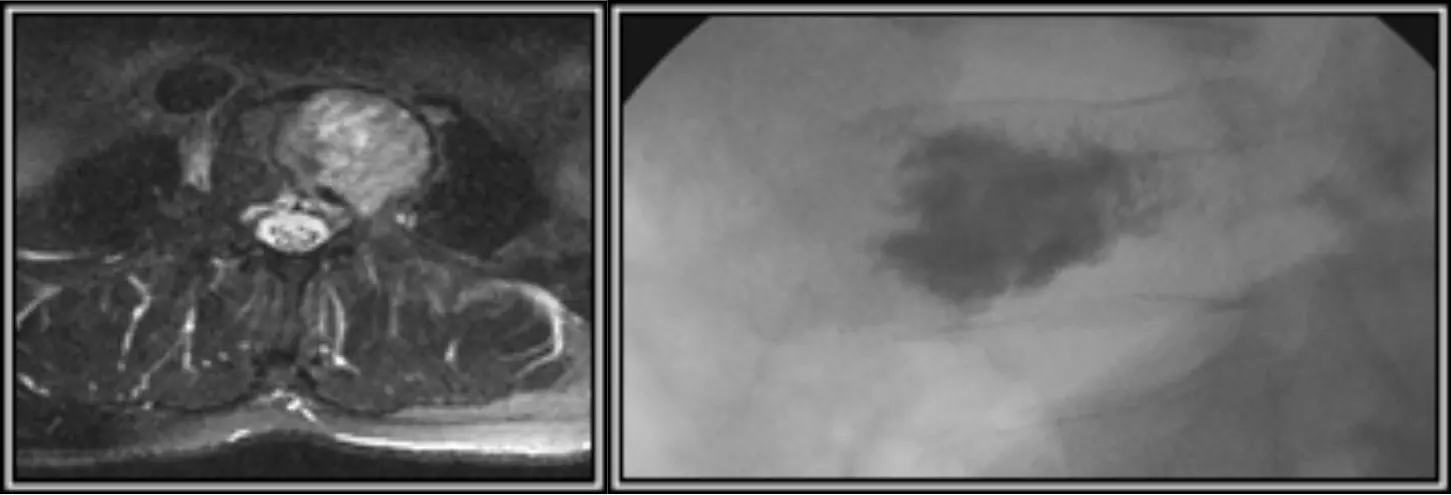
Image showing cementoplasty for spinal metastasis
Disclaimer: The views expressed in this article are of the author and not of Medical Dialogues. The Editorial/Content team of Medical Dialogues has not contributed to the writing/editing/packaging of this article
Powered by WPeMatico









