Healthy lifestyle behaviors, such as good nutrition, smoking cessation and being physically active, along with routine health screenings and managing risk factors for cardiovascular disease and stroke with medication, can help prevent individuals from having a first stroke. Screening for stroke risk and educating people on how to lower their chances of having a stroke ideally begin with their primary care professional and include evidence-based recommendations, according to a new clinical guideline from the American Stroke Association, a division of the American Heart Association, and published today in the Association’s journal Stroke.
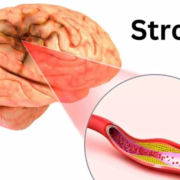
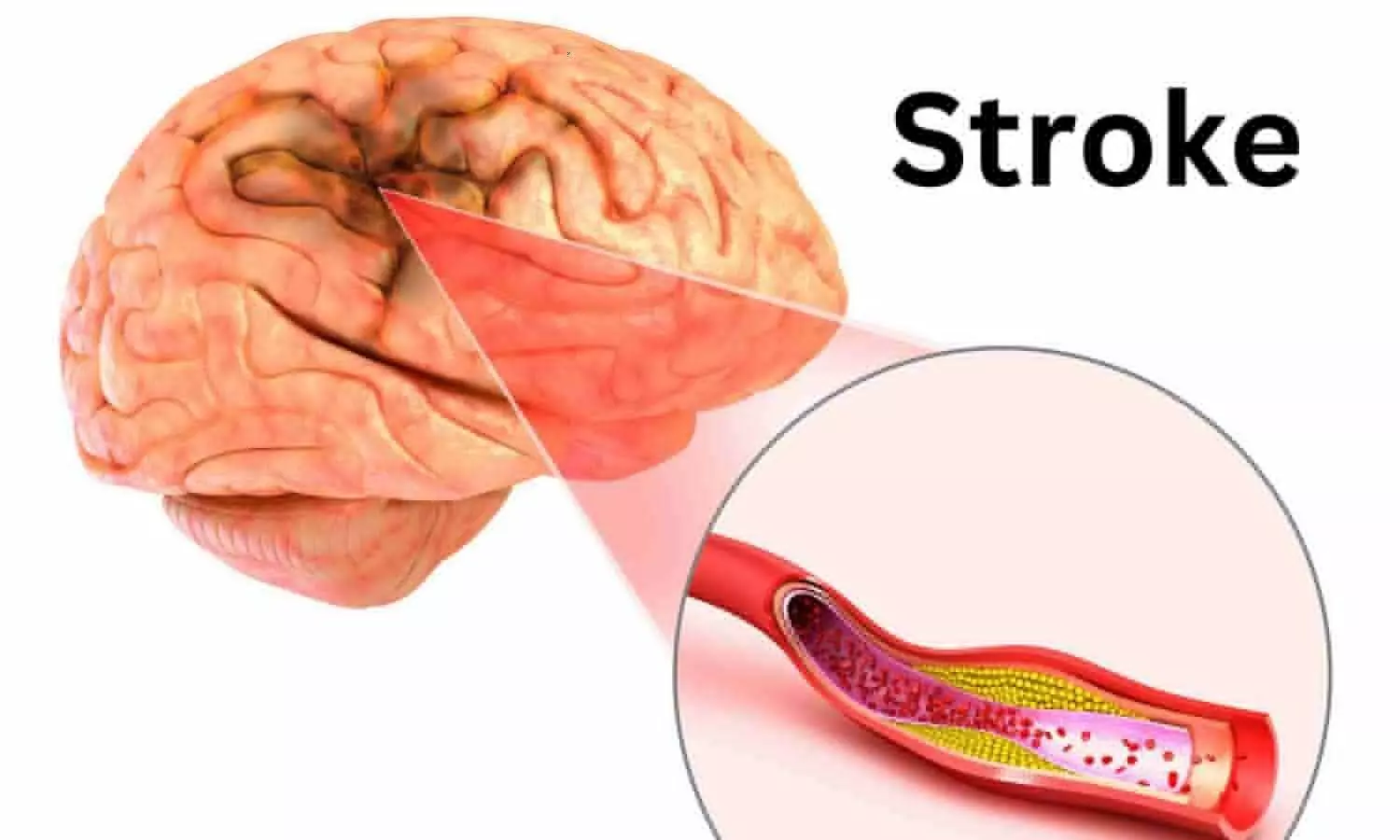
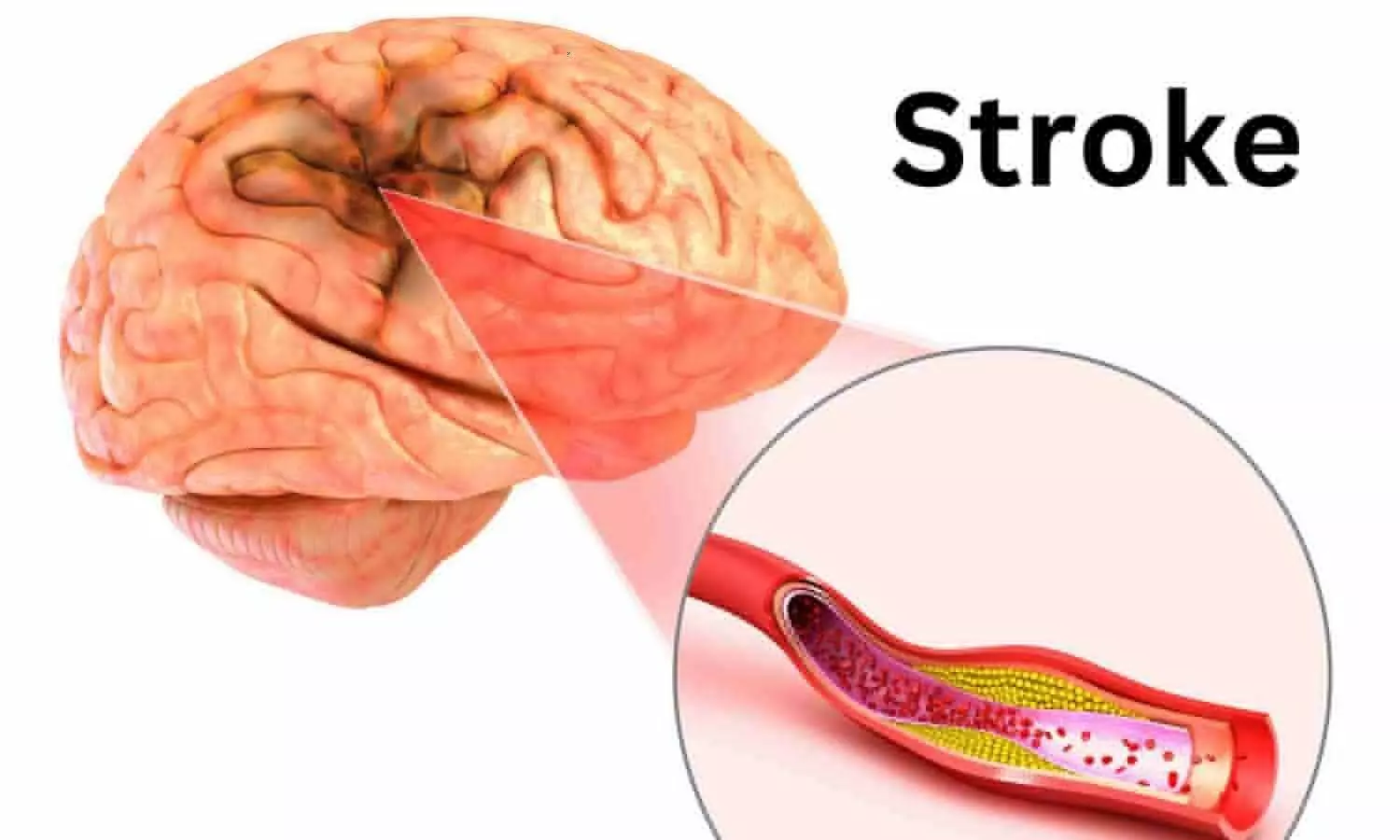
A stroke occurs when blood flow to the brain is interrupted after a blood vessel becomes blocked by a blood clot or ruptures. The result is the brain does not receive the oxygen it needs to properly function. Stroke causes brain damage that can lead to significant disability, including difficulty thinking, talking, walking and interacting with one’s environment. In the U.S., stroke is currently the fifth leading cause of death, resulting in nearly 160,000 deaths annually. Every year, more than 600,000 people in the U.S. have a first stroke, even though up to 80% of strokes are preventable.
“The most effective way to reduce the occurrence of a stroke and stroke-related death is to prevent the first stroke—referred to as primary prevention,” said Chair of the guideline writing group, Cheryl D. Bushnell, M.D., M.H.S., FAHA, professor and vice chair of research in the department of neurology at Wake Forest University School of Medicine in Winston-Salem, North Carolina. “Some populations have an elevated risk of stroke, whether it be due to genetics, lifestyle, biological factors and/or social determinants of health, and in some cases, people do not receive appropriate screening to identify their risk.”
The “2024 Guideline for the Primary Prevention of Stroke” replaces the 2014 version and is a resource for clinicians in implementing a variety of prevention strategies for individuals with no prior history of stroke. The new guideline provides evidence-based recommendations for strategies to support brain health and prevent stroke throughout a person’s lifespan by improving healthy lifestyle behaviors and getting preventive care.
“This guideline is important because new discoveries have been made since the last update 10 years ago. Understanding which people are at increased risk of a first stroke and providing support to preserve heart and brain health can help prevent a first stroke,” said Bushnell.
Key stroke prevention recommendations include regular health screenings, identifying risk factors, lifestyle interventions and medications, when indicated.
Identifying and Managing Risk Factors
Unidentified and unmanaged cardiovascular disease risk factors can cause damage to arteries, the brain and the heart years before cardiovascular disease and stroke occur. Primary care health professionals should promote brain health for patients through stroke prevention education, screenings and addressing risk factors from birth to old age.
Modifiable risk factors for stroke, such as high blood pressure, overweight and obesity, elevated cholesterol and elevated blood sugar, can be identified with physical exams and blood tests. These conditions should be addressed with healthy lifestyle and behavioral changes and may include medications for select patients. Antihypertensive medications to reduce blood pressure and statin medications to lower cholesterol can help to reduce the risk of first stroke in adults with increased cardiovascular disease risk and those receiving CVD care. A new recommendation is consideration of glucagon-like protein-1 (GLP-1) receptor agonist medications, which are FDA-approved to reduce the risk of cardiovascular disease in people with overweight or obesity and/or Type 2 diabetes.
Healthy Lifestyle Behaviors
The most common, treatable lifestyle behaviors that can help reduce stroke risk are detailed in the Association’s Life’s Essential 8 cardiovascular health metrics. They include healthy nutrition, regular physical activity, avoiding tobacco, healthy sleep and weight, controlling cholesterol, and managing blood pressure and blood sugar. The guideline recommends that adults with no prior cardiovascular disease, as well as those with increased risk, follow a Mediterranean dietary pattern. Mediterranean dietary programs have been shown to reduce the risk of stroke, especially when supplemented with nuts and olive oil.
Physical activity is also essential for stroke risk reduction and overall heart health. Physical activity can help to improve important health measures such as blood pressure, cholesterol, inflammatory markers, insulin resistance, endothelial function and weight. The guideline urges health care professionals to routinely screen patients for sedentary behavior, a confirmed risk factor for stroke, and counsel them to engage in regular physical activity. The Association reinforces the U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion’s recommendation that adults get at least 150 minutes per week of moderate-intensity aerobic activity or 75 minutes per week of vigorous aerobic activity, or a combination of both, preferably spread throughout the week.
Health Equity and Stroke Risk
New to the guideline is an emphasis on social determinants of health and the impact they have on stroke risk. Social determinants of health are non-medical factors, including education, economic stability, access to care, discrimination, structural racism and neighborhood factors (such as the lack of walkability, lower availability of healthy food and fewer health resources), that contribute to inequities in care and influence overall health. Health care professionals should ensure patient education is available for various educational and language levels, and advocate for their patients by choosing treatments and medications that are effective and affordable.
Health care professionals are also encouraged to connect patients to resources that help address health-related social needs such as food and housing insecurity, refer them to programs that support healthy lifestyle changes and direct them to support programs that may help defray health care costs including medication expenses.
New Sex- and Gender-Specific Recommendations
The guideline also includes some new gender- and sex-specific recommendations for women. Health professionals should screen for conditions that can increase a woman’s risk of stroke, including use of oral contraceptives, high blood pressure during pregnancy, other pregnancy complications such as premature birth, endometriosis, premature ovarian failure and early onset menopause. Treatment of elevated blood pressure during pregnancy and within six weeks of delivery is recommended to reduce the risk of maternal intracerebral hemorrhage.
Transgender women and gender-diverse individuals taking estrogens for gender affirmation may also be at an increased risk of stroke. Evaluation and modification of any existing risk factors are needed to reduce the risk of stroke for these individuals.
“Implementing the recommendations in this guideline would make it possible to significantly reduce the risk of people having a first stroke. Most strategies that we recommend for preventing stroke will also help reduce the risk of dementia, another serious health condition related to vascular issues in the brain,” said Bushnell.
The writing group notes that writing recommendations focused on preventing a first stroke was challenging. There are limitations to some of the evidence that informed the guideline, including that many clinical trials enrolled adults who have already had a cardiovascular event that may include a stroke. The writing group also identified knowledge gaps to help inform topics for future research.
The guideline highlights the need for risk assessment in primary stroke prevention and includes the use of risk prediction tools to estimate risk for atherosclerotic cardiovascular disease so that patients receive timely prevention and treatment strategies. The Association has recently developed a new Predicting Risk of Cardiovascular Disease Events (PREVENT) risk calculator as a screening tool that can help inform preventive treatment decisions. The PREVENT calculator can estimate 10-year and 30-year stroke and heart disease risk in individuals starting at age 30—a decade earlier than the Pooled Cohort Equations, another CVD risk calculator.
According to the American Stroke Association, learning the warning signs of stroke and preventative measures are the best way to avoid strokes and keep them from happening again. The abbreviation F.A.S.T.-for face drooping, arm weakness, speech difficulty, time to call 911 — is a useful tool to recognize the warning signs of stroke and when to call for help.
This guideline was prepared by the volunteer writing group on behalf of the American Stroke Association and is endorsed by the Preventive Cardiovascular Nurses Association and the Society for Vascular Surgery. The American College of Obstetricians and Gynecologists supports the clinical value of this document as an educational tool.
Since 1990, the American Stroke Association has translated scientific evidence into clinical practice guidelines with recommendations to improve cerebrovascular health. The “2024 Guideline for the Primary Prevention of Stroke” replaces the 2014 “Guidelines for the Primary Prevention of Stroke.” This updated guideline is intended to be a resource for clinicians to use to guide various prevention strategies for individuals with no history of stroke. The Association supports the development and publication of clinical practice guidelines without commercial support, and members volunteer their time to the writing and review efforts.
Reference:
Cheryl Bushnell, Walter N. Kernan, Anjail Z. Sharrief, Seemant Chaturvedi, John W. Cole, William K. Cornwell III, Christine Cosby-Gaither, 2024 Guideline for the Primary Prevention of Stroke: A Guideline From the American Heart Association/American Stroke Association, Stroke, https://doi.org/10.1161/STR.0000000000000475