Severe Anemia Elevates Risk of PPH During Elective Labor Induction, reveals research
According to researchers, pregnant women with severe anemia stand at a more substantial risk of experiencing postpartum hemorrhage (PPH) if labor is induced electively during late pregnancy. A new study was recently published in the Journal of Gynecology and Obstetrics conducted by Tuck S. and colleagues.
The most important cause of maternal mortality in many parts of the world is PPH. Anemia in pregnancy is a known risk factor for PPH, though the ways in which anemia severity and methods of labor induction/augmentation interact to influence risk for PPH has not been well understood. This study examines in detail how those factors interact to raise risk for PPH and provides insights that can guide clinical decision-making in obstetric care.
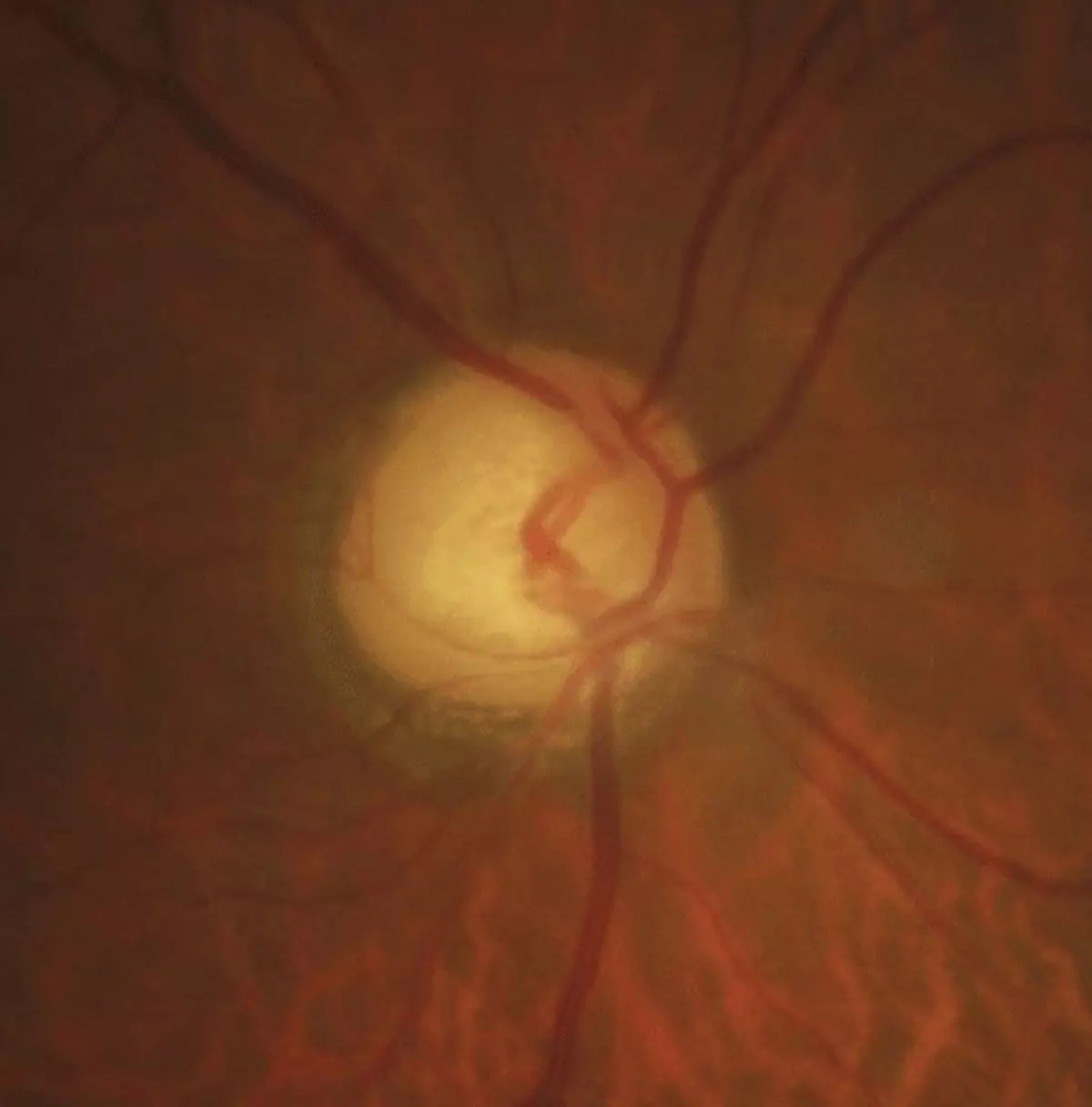
This prospective cohort study enrolled 9,420 pregnant women across India in 13 hospitals. Hemoglobin at ≥28 weeks of gestation was assessed and blood loss after delivery during follow-up. PPH was defined as blood loss ≥500 mL for vaginal births or ≥1,000 mL for cesarean sections. Anemia severity was defined by the following:
-
No/Mild: Hemoglobin ≥10 g/dL
-
Moderate: Hemoglobin 7 to 9.9 g/dL
-
Severe: Hemoglobin <7 g/dL
The indications of labor induction/augmentation were categorized as either clinically indicated or elective, and multivariable Poisson regression was used to compute associations between these factors and PPH, adjusting for confounders.
Anemia Severity and Risk of PPH:
-
Patients with severe anemia (hemoglobin <7 g/dL) were at strongly increased risk of PPH.
-
Associations were not significant at no/mild or moderate anemia levels.
Impact of Labor Induction/Augmentation:
-
Elective labor induction significantly increased the risk for PPH in women with severe anemia (adjusted risk ratio, 3.44; 95% CI: 1.29–9.18).
-
Clinically indicated inductions were not associated with a significant increase in the risk for PPH in this group (adjusted risk ratio, 1.22; 95% CI: 0.42–3.55).
Interaction Between Factors:
-
A significant interaction was found between anemia severity and type of labor induction/augmentation regarding the risk for PPH (P = 0.003).
Labor management should be stratified according to the severity of anemia. Induction/augmentation of labour is safe in most women with anemia, but elective procedures should be avoided in severe cases to minimize the risk of PPH. These findings stress the need for individualised obstetric care for better maternal outcomes.
Reference:
Powered by WPeMatico