‘Inflammatory’ diet during pregnancy may raise child’s diabetes type 1 risk
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Bangalore: AstraZeneca Pharma India Limited has received permission from the Central
Drugs Standard Control Organisation (CDSCO), Directorate General of Health Services, Government of India to
import for sale and distribution of Durvalumab Solution for Infusion 120 mg/2.4 ml and 500 mg/10 ml
(Brand name: Imfinzi) for an additional indication.
Through this approval, Durvalumab in combination with carboplatin and paclitaxel is indicated for the
first-line treatment of adults with primary advanced or recurrent endometrial cancer who are candidates
for systemic therapy, followed by maintenance treatment with Durvalumab in combination with
olaparib in endometrial cancer that is mismatch repair proficient (pMMR).
The receipt of this permission paves way for the marketing of Durvalumab Solution for Infusion 120
mg/2.4 ml and 500 mg/10 ml (Brand name: Imfinzi) in India for the specified additional indication,
subject to the receipt of related statutory approvals, if any.
In March this year, AstraZeneca Pharma India received CDSCO approval to import for sale and distribution of Imfinzi for patients with limited-stage small cell lung cancer (LS-SCLC) whose disease has not progressed following platinum-based chemoradiation therapy.
Additionally, earlier in the same month, the company obtained permission for Durvalumab in combination with Tremelimumab for patients with unresectable hepatocellular carcinoma (uHCC). Hepatocellular carcinoma (HCC) is a type of liver cancer. Because symptoms often don’t appear until the advanced stages, getting diagnosed with liver cancer like HCC can come as a shock.
Read also: AstraZeneca Pharma India secures CDSCO nod to import, sell Durvalumab for small cell lung cancer
AstraZeneca India was established in 1979 and is headquartered at Bengaluru, Karnataka. AstraZeneca Pharma India Limited is the operating company and covers manufacturing, sales and marketing activities of the company in India.
It is a listed company and is a subsidiary of AstraZeneca Plc, UK.
Read also: AstraZeneca Pharma India names Praveen Rao Akkinepally as new MD, succeeding Dr Sanjeev Panchal
Powered by WPeMatico

Lucknow: Criticising the poor state of medical facilities in Uttar Pradesh, Samajwadi Party president Akhilesh Yadav launched a scathing attack on the BJP government.
He said, “The healthcare of the state is in ICU. The condition of the hospitals is pathetic and most of the facilities are only on paper. The poor are being treated miserably while the medical infrastructure given by the SP government is being wasted instead of improving it, “he alleged, news agency UNI reported.
On the eve of his 52nd birthday, Akhilesh Yadav made these comment in the voluntary blood donation camp held at Shatabdi Hospital here.
Also Read:UP govt slams Akhilesh Yadav for insulting doctor in Kannauj
The event was organised by Maurya, Shakya, Kushwaha and Saini Samaj (PDA Samaj) at the hospital on the eve of Akhilesh Yadav’s birthday tomorrow.
Akhilesh Yadav himself reached the camp and encouraged the workers. A large number of youth and activists donated blood in the camp. Akhilesh Yadav described it as the real picture of socialism.
According to an UNI report, the SP President said, “The BJP government has not cleaned the rivers but minted money on it. The result is that Gomti is dirty. KGMU is not just the country but the world’s ingredient institution, and if the SP government is formed, then we will give all the resources to create the best institution in the world. “
Akhilesh Yadav said, “I want to thank all our dedicated workers of the PDA family who have joined the blood donation camp today.”
He also said that his birthday becomes a symbol of service, dedication and socialism for party workers.
Medical Dialogues had earlier reported that Uttar Pradesh Deputy Chief Minister and Health Minister Brajesh Pathak announced significant changes in the designation and recruitment criteria for nursing staff within the state’s health department. The changes align with the central government’s health department norms and aim to upgrade the status and recognition of nurses.
Also Read:Akhilesh demands CBI probe into Gorakhpur hospital death
Powered by WPeMatico
Dapagliflozin reduced the risk of all-cause mortality or worsening heart failure by 28% in patients with aortic stenosis undergoing transcatheter aortic valve implantation (TAVI), a new study has reported.
The DapaTAVI trial, a multicenter randomized controlled study published in The New England Journal of Medicine, assessed dapagliflozin 10 mg once daily in 1222 high-risk patients undergoing TAVI across 39 centers in Spain. Participants had severe aortic stenosis, prior heart failure, and at least one additional risk factor—moderate renal impairment (eGFR 25–75 ml/min/1.73 m²), type 2 diabetes, or LVEF ≤40%; the mean age was 82.4 years, with 72% aged ≥80 years. The primary endpoint was a composite of all-cause mortality or worsening heart failure at one year. The trial’s primary endpoint was a composite of all-cause mortality or worsening heart failure (hospitalization or urgent visits requiring IV diuretics) at one-year follow-up.
Key findings of the study include
At one year, dapagliflozin reduced the primary composite outcome of all-cause mortality or worsening heart failure by 28% relative risk reduction (15.0% dapagliflozin vs 20.1% standard care; HR 0.72; 95% CI, 0.55–0.95; P = 0.02).
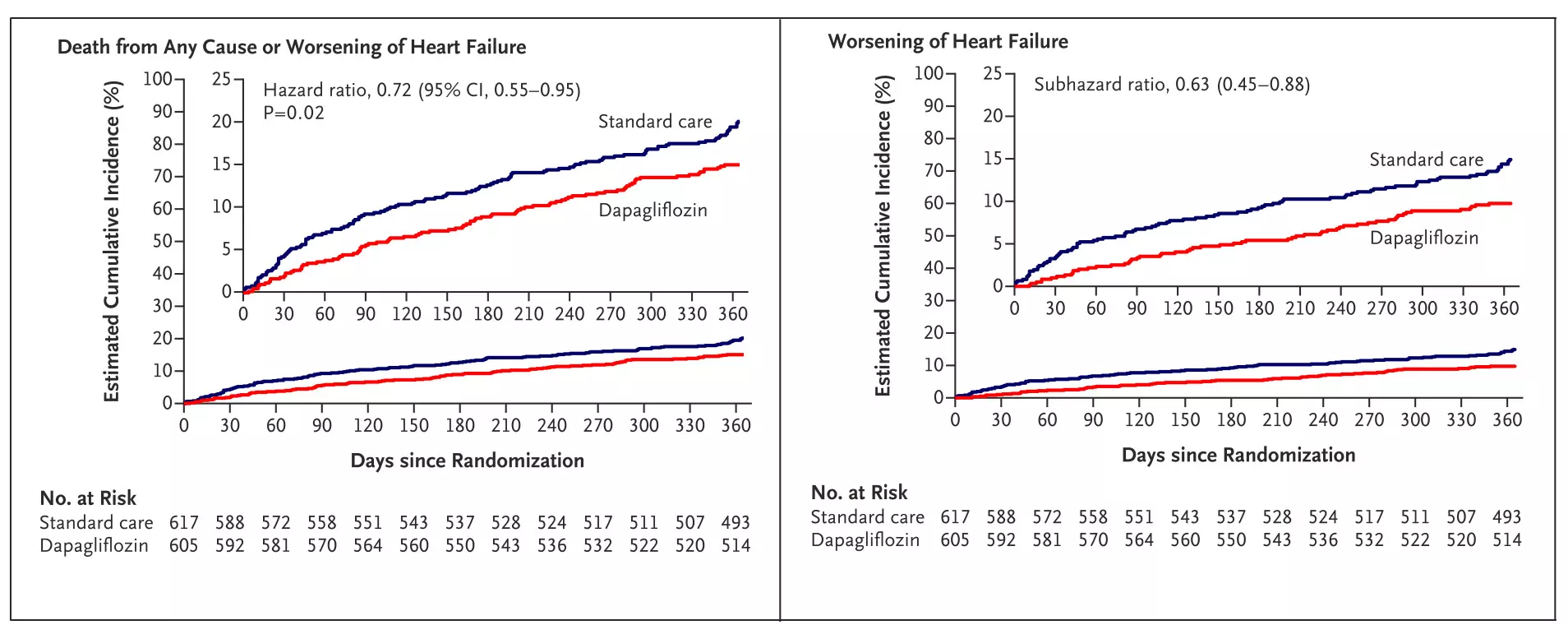
Figure: Kaplan–Meier curve showing time to primary composite outcome (death or worsening of heart failure) post-TAVI.Adapted from Raposeiras-Roubín S, et al. Dapagliflozin in Patients Undergoing Transcatheter Aortic-Valve Implantation. N Engl J Med. 2025; DOI: 10.1056/NEJMoa2500366.
Worsening heart failure was reduced by 37% (9.4% vs 14.4%; subHR 0.63; 95% CI, 0.45–0.88), hospitalizations for heart failure by 32% (7.4% vs 10.7%; subHR 0.68; 95% CI, 0.46–0.99), and urgent heart failure visits requiring IV diuretics by 54% (2.8% vs 6.0%; subHR 0.46; 95% CI, 0.26–0.82).
Dapagliflozin also reduced the secondary outcome of cardiovascular death or heart failure hospitalization by 29% (10.1% vs 13.8%; subHR 0.71; 95% CI, 0.51–0.98). The total number of recurrent events—cardiovascular deaths and heart failure hospitalizations—was reduced by 33% (79 vs 121 events; rate ratio 0.67; 95% CI, 0.47–0.95).
A prespecified subgroup analysis was performed to assess the consistency of treatment effect, with key results summarized below.
Benefit in Patients with CV Risk Factors: In patients with type 2 diabetes, dapagliflozin reduced the primary outcome by 33% (15.2% vs 22.7%; HR, 0.63; 95% CI, 0.42–0.94). In those with hypertension, the primary endpoint outcome reduction was 24% (15.3% vs 20.2%; HR 0.73; 95% CI, 0.54–0.97).
Outcome in Patients with Cardiac Co-Morbidities: In patients with preserved left ventricular ejection fraction (LVEF >40%), dapagliflozin reduced primary outcome by 33% (14.1% vs 21.2%; HR 0.67; 95% CI, 0.50–0.91). Those with mild or no left ventricular hypertrophy also benefited, with a 29% event reduction (11.8% vs 16.1%; HR 0.72; 95% CI, 0.52–1.00).
Patients with atrial fibrillation had a 33% relative risk reduction (19.6% vs 29.2%; HR 0.63; 95% CI, 0.44–0.90).
Renal Function: In patients with impaired renal function (eGFR <60 ml/min/1.73 m²), dapagliflozin reduced primary outcome by 28% (17.3% vs 22.9%; HR 0.71; 95% CI, 0.49–1.03). Among those with preserved kidney function (eGFR ≥60), the risk was reduced by 26% (12.7% vs 17.3%; HR 0.72; 95% CI, 0.45–1.16).
Background Cardiovascular Therapy: Dapagliflozin reduced the composite outcome of death or worsening heart failure by 30% in patients receiving RAS inhibitors (12.4% vs 17.6%; HR 0.68; 95% CI, 0.47–0.99). While not statistically significant, similar trends were observed in patients on beta-blockers (19.2% vs 24.9%; HR 0.74; 95% CI, 0.50–1.10) and diuretics (16.8% vs 21.6%; HR 0.75; 95% CI, 0.56–1.02), indicating a consistent treatment effect across therapies.
The results of DapaTAVI trial highlight a promising role for the SGLT2 inhibitor, dapagliflozin, in patients undergoing TAVI, particularly those with coexisting heart failure or renal dysfunction.
Reference: Díez-Villanueva, Pablo, et al. “Dapagliflozin in Patients Undergoing Transcatheter Aortic Valve Implantation.” The New England Journal of Medicine, vol. 390, no. 13, 2025, pp. 1234–1245. DOI: 10.1056/NEJMoa2500366.
Abbreviations: TAVI – Transcatheter Aortic Valve Implantation, DapaTAVI – Dapagliflozin in Patients Undergoing Transcatheter Aortic Valve Implantation, HR – Hazard Ratio, subHR – Subdistribution Hazard Ratio, CI – Confidence Interval, eGFR – Estimated Glomerular Filtration Rate, LVEF – Left Ventricular Ejection Fraction, IV – Intravenous, SGLT2 – Sodium-Glucose Cotransporter 2, RAS – Renin-Angiotensin System
Powered by WPeMatico
Israel: A new study published in JAMA Network Open highlights a key safety insight for patients with type 2 diabetes taking sodium-glucose cotransporter 2 inhibitors (SGLT2is). While these medications are linked to a higher risk of developing erythrocytosis, they do not appear to raise the likelihood of thrombotic events such as heart attacks, strokes, or blood clots.
The study, led by Dr. Maor Lewis from the Department of Family Medicine at Meuhedet Health Maintenance Organization in Tel-Aviv, Israel, analyzed data from over 269,000 adult patients with type 2 diabetes using records from Israel’s largest healthcare system. The research aimed to assess how frequently SGLT2is causes erythrocytosis—a condition characterized by elevated red blood cell levels—and whether this condition is associated with an increased risk of arterial or venous thrombosis.
Using a propensity score-matched design, the researchers compared new users of SGLT2is to those initiating either dipeptidyl peptidase 4 inhibitors (DPP-4is) or glucagon-like peptide 1 receptor agonists (GLP-1RAs). After matching, the final analysis included 68,776 patients in both the SGLT2i and DPP-4i groups and 65,756 in each of the SGLT2i and GLP-1RA groups.
Based on the study, the researchers reported the following findings:
The authors noted that these findings provide significant reassurance about the clinical use of SGLT2 inhibitors. While these medications may cause a measurable increase in red blood cell counts, this effect does not appear to elevate the risk of clot-related complications. They further emphasized that the results add to the expanding body of evidence supporting the favorable cardiovascular safety profile of SGLT2 inhibitors.
According to the authors, ongoing monitoring of hematologic parameters in patients receiving SGLT2is may be advisable, particularly in those with other risk factors for erythrocytosis. However, the absence of a thrombotic signal should ease concerns among prescribers and patients alike.
Reference:
Lewis M, Burrack N, Heymann A, Grossman A, Neuman T, Abuhasira R. Sodium-Glucose Cotransporter 2 Inhibitors, Erythrocytosis, and Thrombosis in Adults With Type 2 Diabetes. JAMA Netw Open. 2025;8(6):e2517086. doi:10.1001/jamanetworkopen.2025.17086
Powered by WPeMatico

Sepsis is when the immune system overshoots its inflammatory reaction to an infection, so strongly that the vital organs begin to shut down. It is life-threatening: each year in the US alone, approximately 750,000 patients are hospitalized for sepsis, of which approximately 27% die. In about 15% of cases, sepsis worsens into septic shock, characterized by dangerously low blood pressure and reduced blood flow to tissues. The risk of death from septic shock is even higher, between 30% and 40%.
The earlier patients with sepsis are treated, the better their prospects. Typically, they receive antibiotics, intravenous fluids, and vasopressors to raise blood pressure. But now, a large cohort study in Frontiers in Immunology has shown for the first time that supplementary treatment with statins could boost their chances of survival.
“Our large, matched cohort study found that treatment with statins was associated with a 39% lower death rate for critically ill patients with sepsis, when measured over 28 days after hospital admission,” said Dr Caifeng Li, the study’s corresponding author and an associate professor at Tianjin Medical University General Hospital in China.
Statins are best known as a protective treatment against cardiovascular disease, which function by lowering ‘bad’ LDL cholesterol and triglycerides, and raising ‘good’ HDL cholesterol. But they have been shown to bring a plethora of further benefits, which explains the burgeoning interest in their use as a supplementary therapy for inflammatory disorders, including sepsis.
Not just lowering cholesterol
“Statins have anti-inflammatory, immunomodulatory, antioxidative, and antithrombotic properties. They may help mitigate excessive inflammatory response, restore endothelial function, and show potential antimicrobial activities,” said Li.
The authors sourced their data from the public Medical Information Mart for Intensive Care-IV (MIMIC-IV) database, which holds the anonymized e-health records of 265,000 patients admitted to the emergency department and the intensive care unit of the Beth Israel Deaconess Medical Center of Boston between 2008 and 2019. Only adults with a diagnosis of sepsis hospitalized for longer than 24 hours were included here.
The authors compared outcomes between patients who received or didn’t receive any statins during their stay besides standard of care, regardless of the type of statin. Unlike in randomized clinical trials – the gold standard among clinical studies – the allocation of treatments is not determined by random in observational studies like the present cohort study. This means that it is in principle hard to rule out that an unknown underlying variable affected allocation, for example if physicians unconsciously or on purpose were prone to give statins to those patients most likely to benefit from them.
However, Li and colleagues used a technique called ‘propensity score matching’ to minimize the risk of such bias: they built a statistical model to determine a likelihood score that a given patient would receive statins, based on their medical records, and then found a matching patient with a similar score, but who didn’t receive statins. In the final sample, 6,070 critical patients received statins while another 6,070 did not.
The primary analysis focused on 28-day all-cause mortality, while supplementary analyses examined outcomes such as the duration of the hospital stay, of mechanical ventilation, and of continuous renal replacement therapy.
The results showed that the 28-day all-cause mortality rate was 14.3% in the statin group and 23.4% in the no statin group, indicating a relative reduction by 39% [9.1 percentage points]. However, the duration of mechanical ventilation (MV) or continuous renal replacement therapy (CRRT) increased by an average of 3 hours and 26 hours, respectively, in the group receiving statins. This prolonged duration of MV and CRRT in the statin group may be attributed to a tradeoff between 28-day all-cause mortality and the duration of MV or CRRT.
“These results strongly suggest that statins may provide a protective effect and improve clinical outcomes for patients with sepsis,” concluded Li.
Supplementary analyses confirmed these results separately for patients with a normal, overweight, or obese body mass index, but not for underweight patients.
Larger randomized clinical trial needed
Why haven’t previous randomized controlled trials, which are in theory more powerful, found any benefit of statins? Li and colleagues speculated that this might be due to poor design. Randomized controlled trials are expensive, and hence are often ‘underpowered’, with too few patients enrolled to show any significant effect.
“Previous randomized controlled trial may not have found a benefit of statins in patients with sepsis due to underreporting of sepsis diagnoses, small sample sizes, and failure to account for the complex interactions between statin use and patient characteristics,” suggested Li.
“An ideal randomized controlled trial to confirm or reject our results should include a large sample size of sepsis patients, with detailed information on statin types, doses, and treatment duration. It should also carefully consider the timing of statin initiation and control for potential confounders,” said Li.
Reference:
Caifeng Li, Statin use during intensive care unit stay is associated with improved clinical outcomes in critically ill patients with sepsis: a cohort study,Frontiers in Immunology,doi.org/10.3389/fimmu.2025.1537172.
Powered by WPeMatico

A recent study published in The Annals of Thoracic Surgery suggests that despite strong clinical guidelines, the use of surgical ablation during coronary artery bypass grafting (CABG) in patients with atrial fibrillation (AF) remains low and potentially life-shortening.
The study reviewed data from over 87,000 Medicare beneficiaries who had preexisting atrial fibrillation and underwent CABG between 2008 and 2019. This revealed that only 22.2% received concomitant surgical ablation. This technique targets the abnormal electrical signals causing AF and was associated with significantly improved long-term survival.
This study found that patients who received surgical ablation during CABG lived a median of 4.4 months longer than those who did not. Also, risk-adjusted median survival was 7.82 years in the ablation group when compared to 7.46 years in the non-ablation group (P < .001).
The survival benefit was even more pronounced when looked at the surgeon practice patterns. The patients operated on by surgeons who frequently perform ablation (defined as doing so in ≥40% of their CABG cases) had a median survival advantage of nearly 5 months (4.96 months) when compared to the patients treated by infrequent ablation surgeons (<5% of cases). Median survival in this analysis was 7.03 years versus 6.62 years, respectively (P < .001).
While the survival gains may appear modest on paper, the public health impact is substantial, given the high volume of CABG procedures and the prevalence of atrial fibrillation in older adults. This study argues that the findings support current guideline recommendations advocating for surgical ablation in AF patients undergoing CABG and spotlight a significant gap between evidence-based guidance and real-world practice.
In a detail examination, 652 surgeons (frequent ablation) performed the procedure in ≥40% of their CABG patients, 1834 surgeons (occasional ablation) performed it in 5–40% of cases and 1193 surgeons (infrequent ablation) did so in <5% of cases. These numbers suggest that a large proportion of cardiac surgeons either rarely or inconsistently offer this beneficial procedure.
As the study brought out, improving adherence to surgical ablation guidelines could meaningfully enhance long-term outcomes for tens of thousands of cardiac surgery patients every year. Overall, while surgical ablation during CABG clearly offers survival advantages, it remains underutilized, which calls for an urgent need for practice alignment with current evidence and guidelines.
Reference:
Schaffer, J. M., Kluis, A., Squiers, J. J., George, T. J., Shih, E., Banwait, J. K., Mack, M. J., & DiMaio, J. M. (2025). Survival after surgical ablation of atrial fibrillation during coronary artery bypass in Medicare beneficiaries. The Annals of Thoracic Surgery. https://doi.org/10.1016/j.athoracsur.2025.03.044
Powered by WPeMatico
