College drinking linked to poor academics and mental health for those around the drinker
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

A new study led by investigators from Mass General Brigham, Harvard T.H. Chan School of Public Health, and the Broad Institute of MIT and Harvard suggests that a Mediterranean-style diet may help reduce dementia risk. The study, published in Nature Medicine, found that people at the highest genetic risk for Alzheimer’s disease benefited more from following a Mediterranean-style diet, showing a greater reduction in dementia risk compared to those at lower genetic risk.
“One reason we wanted to study the Mediterranean diet is because it is the only dietary pattern that has been causally linked to cognitive benefits in a randomized trial,” said study first author Yuxi Liu, PhD, a research fellow in the Department of Medicine at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, and a postdoctoral fellow at the Harvard Chan School and Broad. “We wanted to see whether this benefit might be different in people with varying genetic backgrounds, and to examine the role of blood metabolites, the small molecules that reflect how the body processes food and carries out normal functions.”
Over the last few decades, researchers have learned more about the genetic and metabolic basis of Alzheimer’s disease and related dementias. These are among the most common causes of cognitive decline in older adults. Alzheimer’s disease is known to have a strong genetic component, with heritability estimated at up to 80%.
One gene in particular, apolipoprotein E (APOE), has emerged as the strongest genetic risk factor for sporadic Alzheimer’s disease — the more common type develops later in life and is not directly inherited in a predictable pattern. People who carry one copy of the APOE4 variant have a 3-to-4-fold higher risk of developing Alzheimer’s. People with two copies of the APOE4 variant (called APOE4 homozygous) have a 12-fold higher risk of Alzheimer’s than those without.
To explore how the Mediterranean diet may reduce dementia risk and influence blood metabolites linked to cognitive health, the team analyzed data from 4,215 women in the Nurses’ Health Study, following participants from 1989 to 2023 (average age 57 at baseline). To validate their findings, the researchers analyzed similar data from 1,490 men in the Health Professionals Follow-Up Study, followed from 1993 to 2023.
Researchers evaluated long-term dietary patterns using food frequency questionnaires and examined participants’ blood samples for a broad range of metabolites. Genetic data were used to assess each participant’s inherited risk for Alzheimer’s disease. Participants were then followed over time for new cases of dementia. A subset of 1,037 women underwent regular telephone-based cognitive testing.
They found that the people following a more Mediterranean-style diet had a lower risk of developing dementia and showed slower cognitive decline. The protective effect of the diet was strongest in the high-risk group with two copies of the APOE4 gene variant, suggesting that diet may help offset genetic risk.
“These findings suggest that dietary strategies, specifically the Mediterranean diet, could help reduce the risk of cognitive decline and stave off dementia by broadly influencing key metabolic pathways,” Liu said. “This recommendation applies broadly, but it may be even more important for individuals at a higher genetic risk, such as those carrying two copies of the APOE4 genetic variant.”
A study limitation was that the cohort consisted of well-educated individuals of European ancestry. More research is needed in diverse populations.
In addition, although the study reveals important associations, genetics and metabolomics are not yet part of most clinical risk prediction models for Alzheimer’s disease. People often don’t know their APOE genetics. More work is needed to translate these findings into routine medical practice.
“In future research, we hope to explore whether targeting specific metabolites through diet or other interventions could provide a more personalized approach to reducing dementia risk,” Liu said.
Reference:
Liu, Y., Gu, X., Li, Y. et al. Interplay of genetic predisposition, plasma metabolome and Mediterranean diet in dementia risk and cognitive function. Nat Med (2025). https://doi.org/10.1038/s41591-025-03891-5
Powered by WPeMatico

Recent article compares two different pain management techniques used after upper abdominal surgeries. One is called intrathecal hydromorphone (ITH), where a pain medication is injected directly into the spinal fluid. The other is called a transversus abdominis plane (TAP) block, where numbing medicine is injected into the abdominal wall. The researchers found that patients who received the ITH technique had less severe pain when moving around on the first day after surgery, compared to those who got the TAP block. This suggests the ITH was better at controlling pain during movement. However, the TAP block had some advantages. Patients who got the TAP block had less itching as a side effect, and their bowels started working again sooner after surgery. The amount of pain medication needed was also a bit lower in the TAP block group. Overall, the study suggests that ITH may provide better pain relief, especially when patients are moving around, compared to the TAP block. But the TAP block has some benefits too, like less itching and faster recovery of bowel function. The researchers think the reason for these differences is that the ITH provides longer-lasting pain relief, while the TAP block is more focused on the abdominal area. Since upper abdominal surgeries tend to be very painful, the longer-lasting pain relief from ITH may be more helpful. However, this was a retrospective study, which means the researchers looked back at medical records rather than doing a controlled experiment. So there could be other factors that influenced the results that the researchers didn’t account for. The authors recommend that doctors consider the type of surgery when choosing between ITH and TAP block for pain management. For open abdominal surgeries, ITH may be the better choice. But for less invasive laparoscopic surgeries, the TAP block may be preferable due to its benefits for recovering bowel function. Overall, this study provides helpful information to doctors on the pros and cons of these two pain management techniques for patients undergoing upper abdominal surgery. But more research, especially controlled studies, is still needed to fully understand which approach works best.
Key points –
– Intrathecal hydromorphone and transversus abdominis plane (TAP) block are commonly used analgesic techniques for upper abdominal surgeries, with intrathecal opioid injection providing prolonged analgesia with a lower dose compared to intravenous administration.
– A retrospective study aimed to compare the analgesic efficacy of intrathecal hydromorphone and TAP block in upper abdominal surgeries by assessing the primary outcome of moderate-to-severe pain during movement at 24 hours postoperatively.
– Propensity score-matching (PSM) was used to minimize baseline differences and reduce potential confounding in outcome comparisons, with 91 matched patients in each group showing evenly distributed baseline characteristics.
– The study found that intrathecal hydromorphone was superior to TAP block in reducing moderate-to-severe pain during movement on the first postoperative day after upper abdominal surgery, with a lower incidence of pain and higher comfort levels in the intrathecal group.
– Patients receiving intrathecal hydromorphone required less opioid medication, reported higher satisfaction levels, but had a higher incidence of pruritus and delayed first flatus compared to the TAP block group.
– Future research should focus on integrating the benefits of intrathecal hydromorphone into multimodal analgesia for upper abdominal surgeries and conducting well-designed randomized controlled trials to compare the most effective analgesic technique for this surgical population.
Reference –
Yue-Xin Huang et al. (2025). Intrathecal Hydromorphone Vs. Transversus Abdominis Plane Block For Upper Abdominal Surgery: A Propensity Score-Matching Study. *BMC Anesthesiology*, 25. https://doi.org/10.1186/s12871-025-03107-w.
Powered by WPeMatico

A new study published in the Endocrine journal showed that nitazoxanide lowers inflammation and oxidative stress without compromising glucose regulation in type 2 diabetes.
Hyperglycemia and anomalies in the metabolism of proteins, fats, and carbohydrates are hallmarks of diabetes mellitus (DM), a complicated metabolic disease. The majority of patients do not attain ideal glycemic control, even with the advancements in anti-diabetic medication therapy.
Using one-dimensional drug profile matching, nitazoxanide (NTZ), a broad-spectrum anti-infective medication that has efficacy against a variety of bacteria, viruses, helminthes, and protozoa, was determined to be an agonist of the peroxisome proliferative activated receptor gamma (PPARγ).
According to preclinical evidence, nitazoxanide (NTZ) may be a useful PPAR-γ agonist for type 2 diabetes. Therefore, this study was conducted by Eman Ghonaim and team with to investigate the tolerance and initial effects of NTZ as a supplement to the current metformin-vildagliptin combination on inflammatory biomarkers and glycemic control in individuals with type 2 diabetes.
In the control and NTZ groups, 88 patients (44 in each group) were examined. The combination of metformin and vildagliptin was used to treat every patient. Twice a day, 500 mg of nitazoxanide was administered orally to the NTZ group. Glycemic control, as measured by fasting blood glucose and glycated hemoglobin (HbA1c), was the main result. Fasting insulin, serum interleukin-6 (IL-6), asprosin, malondialdehyde (MDA), and high mobility group box 1 (HMGB-1) were examples of secondary outcomes. Every outcome was assessed both at baseline and three months later.
When comparing NTZ to control, a between-groups comparison showed substantially decreased levels of inflammatory markers [HMGB-1: 10.46 ng/mL (6.37–14.61) vs. 22.60 ng/mL (20.18–27.37) and IL-6: 23.64 ng/L (21.00–32.71) vs. 32.52 ng/L (29.63–36.13), P < 0.001 for both].
Insulin, asprosin, MDA, fasting blood glucose, and HbA1c did not significantly differ between the two groups. Following NTZ therapy, there were significantly decreased levels of IL-6 (P = 0.009), HMGB-1 (P < 0.001), asprosin (P = 0.002), and MDA (P < 0.001).
In contrast, the control group had a substantial rise in both HMGB-1 and IL-6 (P < 0.001 for both). There were no notable changes in any biomarkers between the two groups. Overall, despite no improvement in glycemic indices, nitazoxanide may reduce inflammation and oxidative stress in type 2 diabetes.
Source:
Ghonaim, E. M., Ibrahim, O. M., Hegazy, S. K., Farrag, W. F., & Badr, H. R. (2025). Repurposing nitazoxanide in type 2 diabetes mellitus: a randomized controlled trial. Endocrine. https://doi.org/10.1007/s12020-025-04387-5
Powered by WPeMatico

For women diagnosed with early breast cancer, the long-term risk of developing a second primary cancer is low (around 2-3% greater than women in the general population), finds a study published by The BMJ today.
The researchers say this information can help reassure many breast cancer survivors who believe their risk of a second primary cancer is much higher than these results suggest.
Breast cancer survivors are at increased risk of developing second primary cancers, but risk estimates from previous studies are inconsistent. The risk and type of a second cancer can also be affected by the initial treatment received, as well as social, lifestyle and genetic factors.
To address this uncertainty, researchers used data from the National Cancer Registration and Analysis Service for England to estimate the long-term risks of second primary cancers compared with the general population, and the various factors associated with these risks.
Their findings are based on 476,373 women diagnosed in England from 1993 to 2016 with early invasive breast cancer at ages 20-75 years who underwent surgery.
Over a follow-up period of up to 20 years, 64,747 women developed a second primary cancer, but the absolute excess risks compared with risks in the general population were small.
By 20 years, 13.6% of women had developed a non-breast cancer (mainly womb, lung or bowel cancer), 2.1% more than expected in the general population, and 5.6% had developed a contralateral breast cancer (on the other side of the body), 3.1% more than expected.
When patients were grouped by age at first breast cancer diagnosis, the excess risk of a second non-breast cancer varied little across age groups. However, the excess risk of a contralateral breast cancer was greater in younger than in older women.
For example, for a woman whose first breast cancer was diagnosed when aged 60, her estimated risks of developing a new cancer by the age of 80 are 17% for non-breast cancer and 5% for contralateral breast cancer compared to risks of 15% and 3% respectively for women of the same age in the general population.
For a woman diagnosed when aged 40, her estimated risks of developing a second cancer by the age of 60 are 6% for both non-breast and contralateral breast cancer compared to 4% and 2% respectively for women in the general population.
When patients were grouped according to other (adjuvant) treatments they received after surgery, radiotherapy was associated with higher rates of contralateral breast and lung cancers, endocrine therapy with uterine cancer (along with reduced contralateral breast cancer), and chemotherapy with acute leukaemia.
Based on these results, the researchers estimate that around 7% of excess second cancers may be due to the use of adjuvant therapies, but note that their benefits outweigh this small risk in almost all circumstances where these treatments are recommended.
The authors acknowledge that their findings may be affected by incomplete cancer registry data for some variables. What’s more, they did not have information on family history, genetic predisposition and lifestyle choices such as smoking.
However, this long-term study describes the development of second cancers according to multiple patient, tumour and treatment characteristics amongst all women with early invasive breast cancer so the findings can reliably inform breast cancer patients and the clinicians who treat and support them.
They are also relevant to clinical practice and policy, and may help inform the design of future studies to assess cancer risk.
These results are reassuring and should be shared widely, say patients in a linked opinion article, who note that finding detailed information on the risks of second cancers after breast cancer was particularly difficult.
In general, the benefits of treatments in protecting patients from recurrence of breast cancer far outweigh the potential downsides, the patients write. Such information should be available and offered by clinicians at the time that adjuvant therapies are discussed.
They acknowledge that not everyone will want all the details at diagnosis, but say it should be there for those who do want it and for those who seek it later. “Information on risks should be readily available. It helps us to plan our lives and think ahead to the future,” they conclude.
Reference:
Powered by WPeMatico
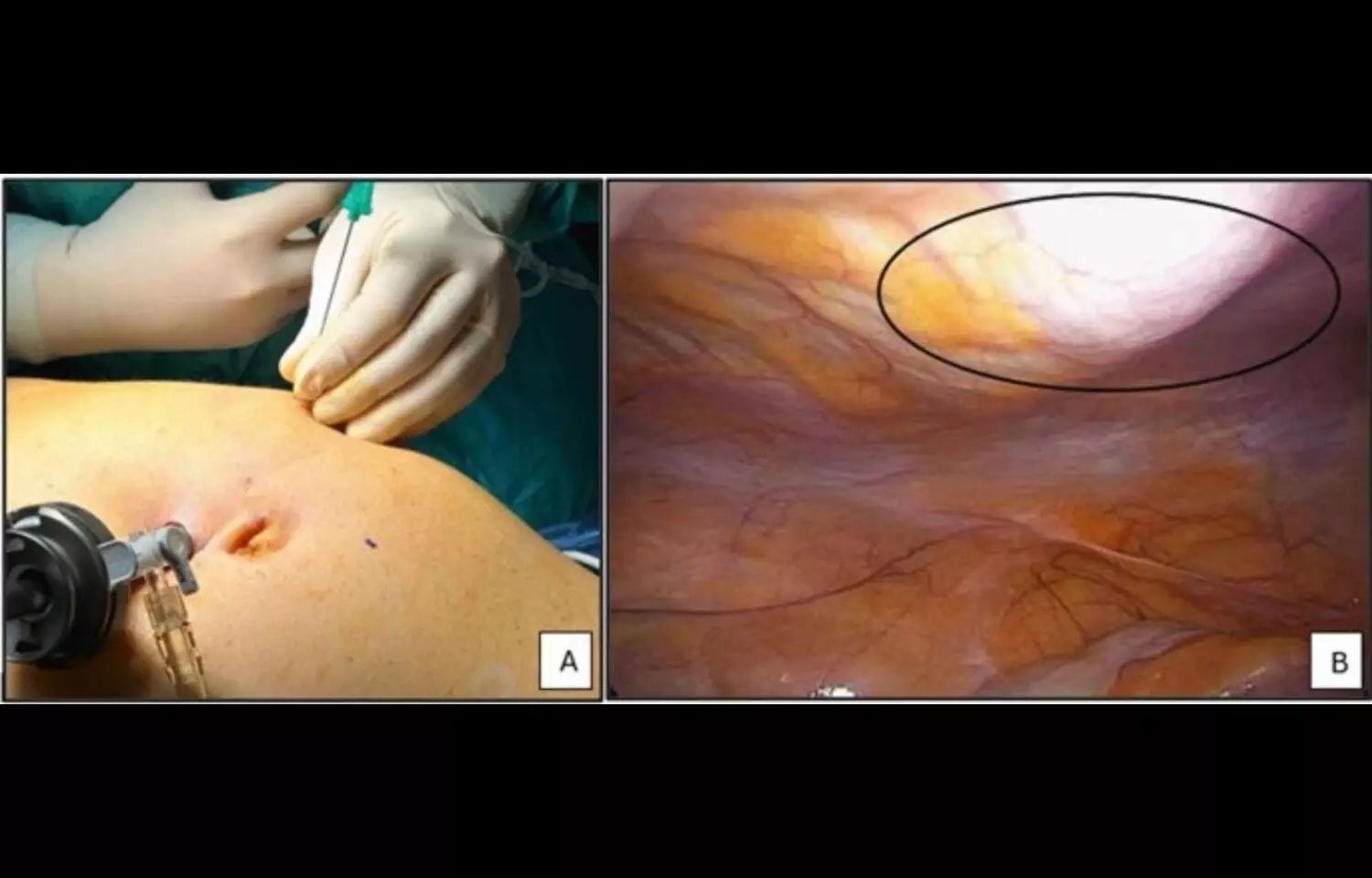
Researchers have found in new research that a single dose of dexamethasone may reduce surgical stress, as reflected by lower C-reactive protein (CRP) levels among patients undergoing laparoscopic abdominal surgery.
The randomized controlled trial, published in BMC Surgery, investigated whether perioperative dexamethasone could attenuate the systemic inflammatory response triggered by minimally invasive abdominal procedures. Surgical trauma is known to induce inflammatory changes, with CRP serving as a key biomarker of stress and recovery. Researchers evaluated adult patients undergoing elective laparoscopic abdominal surgery, who were randomized to receive either a single intravenous dose of dexamethasone or placebo before surgery. The findings showed that CRP levels were significantly lower in the dexamethasone group compared with controls, suggesting a protective effect against excessive surgical stress. Patients who received dexamethasone also demonstrated more stable postoperative recovery profiles, though the study was not powered to assess broader clinical outcomes such as complication rates or length of hospital stay. Importantly, no major adverse effects were associated with the intervention, reinforcing its potential safety for perioperative use. Authors noted that the results align with existing evidence highlighting the anti-inflammatory and immunomodulatory properties of corticosteroids. By blunting excessive inflammatory activation, dexamethasone could help reduce tissue injury, promote faster recovery, and potentially improve patient comfort. However, the researchers cautioned that further large-scale studies are needed to evaluate long-term benefits, optimal dosing, and impact on hard clinical endpoints such as infection rates or overall morbidity. The study contributes to the growing interest in enhanced recovery strategies in surgery. With laparoscopic techniques already associated with reduced trauma compared to open procedures, the addition of low-dose corticosteroid therapy could further optimize postoperative recovery. Researchers suggested that integrating dexamethasone into perioperative protocols may be a simple, cost-effective approach, though caution remains warranted until more definitive evidence is available.
Keywords: dexamethasone; laparoscopic abdominal surgery; surgical stress; C-reactive protein; randomized controlled trial; perioperative care; corticosteroids; inflammation; recovery; BMC Surgery.
Powered by WPeMatico
