IBS Patients Face Higher Risk of Developing IBD, suggests study

Researchers have discovered in a new study that irritable bowel syndrome (IBS) patients have a much greater long-term risk of acquiring inflammatory bowel disease (IBD) than the general population. The study concluded that IBS patients, particularly those with the diarrhea-predominant subtype (IBS-D), had a higher risk of developing ulcerative colitis (UC) or Crohn’s disease (CD) in the long run. The study was published in the Journal of Gastroenterology by Huixin S. and colleagues.
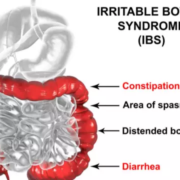
IBS and IBD are two prevalent but different gastrointestinal disorders. IBS is defined as a functional disorder in which there is abdominal pain, bloating, diarrhea, or constipation, whereas IBD, encompassing UC and CD, is a chronic inflammatory bowel disease of the gastrointestinal tract with ongoing complications. This UK Biobank large-scale study gives the strongest evidence to date that IBS patients are at a significantly increased risk of developing IBD.
The study team examined 447,631 baseline participants without IBD (2006–2010) for longitudinal cohort analysis and 76,992 participants who filled out the Digestive Health Questionnaire (2017–2018) for cross-sectional analysis. The main outcome in the cohort study was incident new cases of IBD, with Cox proportional hazards models calculating hazard ratios (HRs). In the cross-sectional design, prevalent IBD was taken as the outcome, and logistic regression calculated odds ratios (ORs).
Results
-
During a median follow-up of 14.2 years, the cohort study ascertained 2,916 new cases of IBD, including 2,097 ulcerative colitis (UC) and 1,015 Crohn’s disease (CD) cases.
In comparison with non-IBS participants, IBS patients exhibited:
-
68% increased risk of IBD (HR = 1.68, 95% CI: 1.47–1.92).
-
60% increased risk of UC (HR = 1.60, 95% CI: 1.36–1.89).
-
104% increased risk of CD (HR = 2.04, 95% CI: 1.66–2.51).
-
Notably, the risk continued to persist in the long term, with IBS patients continuing to have a 55% increased risk of IBD at 10 years (HR = 1.55, 95% CI: 1.27–1.89).
In cross-sectional analysis, IBS patients had markedly increased odds of IBD:
-
2.40-fold increased odds of overall IBD (OR = 2.40, 95% CI: 2.14–2.70).
-
2.18-fold increased odds of UC (OR = 2.18, 95% CI: 1.92–2.48).
-
3.15-fold increased odds of CD (OR = 3.15, 95% CI: 2.68–3.70).
-
Among the IBS subtypes, the IBS-D group had the highest odds with a 3.72 times higher risk of IBD (OR = 3.72, 95% CI: 3.24–4.28).
This large population study in UK Biobank produces strong evidence that IBS patients, particularly IBS-D, have a significantly higher risk of developing IBD, including UC and CD, compared to the general population. This elevated risk is maintained for more than a decade, supporting the requirement for long-term watchfulness among IBS patients. These findings suggest that IBS might not only be thought of as a functional disorder but also as an occult risk factor for the future development of inflammatory bowel diseases.
Reference:
Song, H., Zhou, Y., Liu, S. et al. Long-term risk of inflammatory bowel disease in patients with irritable bowel syndrome: the cross-sectional and longitudinal relationship. J Gastroenterol (2025). https://doi.org/10.1007/s00535-025-02304-1
Powered by WPeMatico