Dupilumab Outperforms Omalizumab in First Head-to-Head Trial for Severe CRSwNP with Asthma: Study
The EVEREST trial directly compared biologics in severe chronic rhinosinusitis with nasal polyps (CRSwNP) and coexisting asthma, and found that dupilumab (Dupixent) was superior to omalizumab (Xolair). At week 24, dupilumab achieved better results across all primary and secondary efficacy endpoints. The findings were published in the recent issue Lancet Respiratory Medicine.
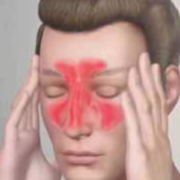
CRSwNP is a chronic inflammatory condition primarily driven by type 2 inflammation, often leading to nasal obstruction, loss of smell, and significant impairment of quality of life. Biologics like dupilumab, which targets interleukin (IL)-4 and IL-13 signaling, and omalizumab, which targets immunoglobulin E (IgE), have each been shown to reduce symptoms. Until now, however, no trial had directly compared their performance.
This phase 4 trial enrolled 360 participants across 17 countries between 2021 and 2024. The patients included were adults with severe, uncontrolled CRSwNP (nasal polyp score ≥5, with congestion and smell loss lasting at least 8 weeks) and physician-diagnosed asthma. They were randomly assigned to receive either dupilumab (300 mg every two weeks) or omalizumab (dose adjusted by weight and IgE levels) for 24 weeks, along with standard mometasone furoate nasal spray.
The main goals of this study were improvement in nasal polyp size, measured endoscopically, and improvement in smell, tested using the University of Pennsylvania Smell Identification Test (UPSIT). Out of 819 screened patients, 360 were enrolled, where 181 received dupilumab and 179 received omalizumab. The participants were predominantly middle-aged (mean age 52 years), with 55% male and 45% female representation.
At 24 weeks, dupilumab outperformed omalizumab across all primary and secondary measures. Patients on dupilumab saw a greater reduction in nasal polyp size, with an average decrease of –1.6 points when compared with omalizumab. Smell recovery was also significantly better, with UPSIT scores improving by an average of 8 points in the dupilumab group versus the omalizumab group. Both results were statistically highly significant (p<0.0001).
When safety was assessed, 64% of dupilumab recipients and 67% of omalizumab recipients reported events. The most frequent were nasopharyngitis, accidental overdose, headache, upper respiratory infections, and cough. No deaths were reported during the trial. Overall, the findings establish dupilumab as a more effective option for patients struggling with severe nasal polyps and asthma, which reinfored its role as a first-choice biologic in type 2 inflammatory respiratory disease.
Source:
De Corso, E., Canonica, G. W., Heffler, E., Springer, M., Grzegorzek, T., Viana, M., Horváth, Z., Mullol, J., Gevaert, P., Michel, J., Peters, A. T., Wagenmann, M., Zaghloul, S., Zhang, M., Corbett, M., Nash, S., Angello, J. T., Radwan, A., Deniz, Y., … Hellings, P. W. (2025). Dupilumab versus omalizumab in patients with chronic rhinosinusitis with nasal polyps and coexisting asthma (EVEREST): a multicentre, randomised, double-blind, head-to-head phase 4 trial. The Lancet. Respiratory Medicine. https://doi.org/10.1016/s2213-2600(25)00287-5
Powered by WPeMatico