Why exercise could actually save your heartbeats—not waste them
Powered by WPeMatico
Powered by WPeMatico

New Delhi: A shocking video from Vardhman Mahavir Medical College (VMMC) and Safdarjung Hospital, recently posted on social media showed a portion of the ceiling in a boys’ hostel collapsed onto the floor of a medical student’s room. The doctor who uploaded the video claimed that the student sustained minor injuries.
In the video, a part of the roof is seen collapsed on the floor, with debris scattered around, some even landing on a student’s bed. The plaster and part of the ceiling suddenly fell.
The medical student present in the room at the time sustained minor injuries but was immediately given first aid. According to local media report, his condition is stable, and he did not suffer any serious injuries.
Also read- Dr Devaunshi Kaul makes history as first woman president of FORDA
The incident has highlighted the poor infrastructure and living conditions of students in the hostel at one of the country’s top medical institutions.
The roof collapse occurred on the 7th floor of the hostel building, often referred to by students as the “Bhoot Bangla.” In his post on X (formerly Twitter), the doctor stated that the condition is so poor it “could claim the life of doctors before the patient.”
Reacting to the incident on X, a doctor recalled: “In my UG days it was already on life support, we’d shifted to the new boys’ hostel by 2nd–3rd year. Looks like the OBH roof finally gave up. The funny part? It still gets “maintenance” money every third month. Classic supervisor–thekedaar nexus. The so-called paint was mostly water.”
A doctor also pointed out that the hospital’s infrastructure problems are not limited to the hostels. He wrote, “Safdarjung’s infrastructure is so bad that if it rains for half an hour, the whole H block gets flooded. In the whole Emergency building there is not a single hygienic washroom for doctors.”
While another doctor said, “It’s worse than the kafala system construction labourers face in the Middle East.”
As per Rashtriya Judgment media report, the hospital administration has assured prompt action, and steps are being taken to inspect the safety of the building.
Powered by WPeMatico

New research from Stockholm has found that individuals with a history of smoking face a significantly higher risk of all four subtypes of type 2 diabetes, with genetic susceptibility further increasing the likelihood.
The characteristics of type 2 diabetes vary from patient to patient and it has been proposed that the condition is made up of four subtypes. Now, new research being presented at the annual meeting of the European Association for the Study of Diabetes (EASD) in Vienna, Austria (15-19 September) shows that smoking increases the risk of the condition, regardless of subtype.
The researchers in Sweden, Norway and Finland also found that people with a genetic susceptibility to develop diabetes seem more vulnerable to the adverse effects of smoking.
It has previously been suggested that type 2 diabetes (T2D) can be divided into the following subtypes: SIRD (severe insulin-resistant diabetes), characterised by insulin resistance (where the body’s cells don’t respond to properly to insulin and can’t easily take up glucose from the blood); SIDD (severe insulin-deficient diabetes), characterised by a lack of insulin; MOD (mild obesity-related diabetes), associated with obesity and younger age of onset; and MARD (mild age-related diabetes) which develops later in life.
Severity, prognosis and risk of complications differ across the subtypes but it is not clear if they have different risk factors.
To find out more, Emmy Keysendal, a PhD student at Karolinska Institutet, in Stockholm, Sweden, and colleagues examined the link between smoking, which is already known to be a potent risk factor for T2D in general, and other forms of tobacco use, and the various subtypes of T2D.
The researchers used data on 3,325 individuals with T2D (495 SIDD, 477 SIRD, 693 MOD and 1660 MARD) and 3,897 controls from a long-running diabetes study in Norway (average follow-up time of 17 years) and a case-control study in Sweden.
They found that ever smokers (current and past smokers) were at higher risk of all four sub-types of T2D than those who had never smoked. The link between smoking and SIRD was particularly strong.
Ever smokers were more than twice as likely (2.15 times) as never smokers to develop SIRD. This compares with increases in risk of 20% for SIDD, 29% for MOD and 27% for MARD.
Smoking was estimated to be responsible for more than a third of SIRD cases, but less than 15% of the other diabetes subtypes (SIDD, MOD and MARD).
Smoking heavily (≥15 pack-years/20 cigarettes a day for 15 years or equivalent) further increased the risk of all four subtypes. Heavy smokers were 2.35 times more likely to develop SIRD than never smokers and 52%, 57% and 45% more likely develop SIDD, MOD and MARD, respectively.
Interestingly, the data on men in Sweden suggested that heavy use of snus, a smokeless tobacco product popular in Scandinavian countries, was linked to increased risk of the severe subtypes SIDD (19% higher risk) and SIRD (13% higher risk) compared to never users of snus.
The study also explored whether smoking further increased the risk in individuals with a genetic predisposition to T2D, insulin resistance or reduced insulin secretion.
This showed that heavy smokers with genetic predisposition to T2D or reduced insulin secretion were particularly vulnerable.
For example, those who smoked heavily and had a high genetic risk for impaired insulin secretion had more than three times the risk (3.52-fold) of developing SIRD compared to those without these risk factors.
The researchers concluded that smoking increases the risk of T2D, whatever the subtype.
Ms Keysendal adds: “It is clear that smoking increases the risk of type 2 diabetes whatever the subtype, that is, regardless, of whether the diabetes is characterised by insulin resistance, lack of insulin, obesity or old age.
“The strongest association was seen for the subtype characterised by severe insulin resistance (SIRD), which suggests that smoking may contribute to diabetes by impairing the body’s ability to respond to insulin.
“Our findings emphasise the importance of smoking cessation in the prevention of type 2 diabetes. They also indicate that genetic information may help identify individuals most likely to benefit from extra support in stopping smoking.”
Reference:
Smoking increases the risk of type 2 diabetes, regardless of its characteristics, European Association for the Study of Diabetes, Meeting: Annual Meeting of the European Association for the Study of Diabetes (EASD).
Powered by WPeMatico

France: The findings of a new study published in JAMA Cardiology suggest that an electrophysiological study (EPS) provides greater accuracy than an electrocardiogram (ECG) in identifying patients with myotonic dystrophy type 1 (DM1) who may benefit from prophylactic permanent pacing.
Powered by WPeMatico

Canada: Empagliflozin did not significantly preserve beta-cell function in women with a recent history of gestational diabetes, according to a randomized, placebo-controlled trial published in Diabetes, Obesity and Metabolism. While the study did not show a clear benefit for beta-cell health, researchers observed signals suggesting the drug might help stabilize insulin sensitivity and fasting glucose, highlighting the need for larger, longer studies.
Powered by WPeMatico
A new study published in The Lancet Infectious Diseases involving over 460,000 children and adolescents across 40 paediatric hospitals in the USA suggests that children who were infected with COVID-19 for the second time during the Omicron wave had more than double the risk of developing long COVID.
Conducted by researchers under the US National Institutes of Health (NIH)-funded RECOVER Initiative*, this is the largest study to date examining the long-term effects of COVID-19 reinfection in young people. The study analysed electronic health records from January 2022 through October 2023, a period dominated by the highly transmissible Omicron variant. Researchers compared health outcomes following children’s first and second documented COVID-19 infections to isolate the risks associated with reinfection.
They found that after a first COVID-19 infection, about 904 children per million developed long COVID within six months. Following a second infection (reinfection), this number more than doubled to approximately 1,884 children per million. The higher risk was observed across many different groups in the study, regardless of whether they were vaccinated, how serious their first illness was, their age, gender, race or ethnicity, or if they were living with overweight or obesity. The authors say this increased risk of long COVID following reinfections highlights the continued importance of preventing COVID-19 infections through vaccination and other protective measures such as masking and social distancing.
Reinfection was linked to a wide range of rare but persistent and sometimes serious conditions potentially associated with long COVID in children, including heart inflammation (myocarditis), blood clots, kidney injury, cognitive difficulties, fatigue, and respiratory problems.
The authors emphasise that while vaccines and other prevention measures may not completely eliminate the risk of contracting COVID-19, they remain the most effective way to prevent both initial infections and reinfections, thereby reducing the risk of long-lasting symptoms in children. They say the study’s findings reinforce the need to strengthen public health efforts to increase COVID-19 vaccination coverage among children and adolescents.
*The NIH’s RECOVER (Researching COVID to Enhance Recovery) Initiative is dedicated to understanding long COVID, developing better treatments, and guiding strategies to protect people of all ages from the prolonged effects of COVID-19.
Reference:
Zhang, Bingyu et al., Long COVID associated with SARS-CoV-2 reinfection among children and adolescents in the omicron era (RECOVER-EHR): a retrospective cohort study, The Lancet Infectious Diseases, DOI:10.1016/S1473-3099(25)00476-1.
Powered by WPeMatico
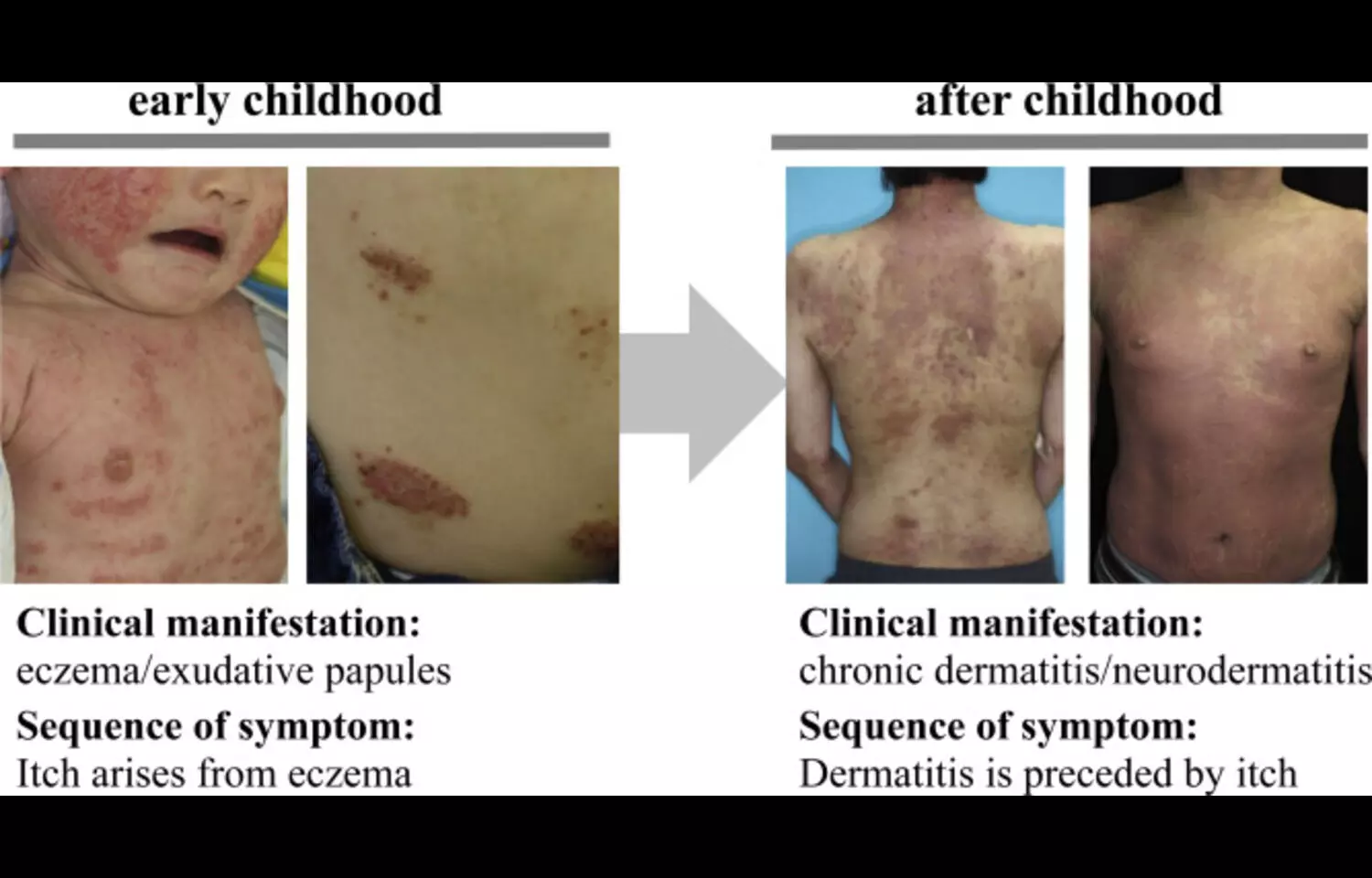
According to a new study habitual scratching was prevalent across patients of all levels of atopic dermatitis (AD) severity and was linked to greater disease severity, emphasizing the need to recognize and manage unconscious scratching as part of holistic atopic dermatitis care.
Scratching is one of the most disruptive features of atopic dermatitis. It not only worsens inflammation but also damages the protective barrier of the skin, making the condition harder to control. While scratching is often thought to be a direct response to itching, many people affected by atopic dermatitis also develop a different behavior known as habitual scratching. This form of scratching is repetitive, unconscious, and can occur even when there is no itch. Until recently, little was known about how common this behavior is among patients in Japan and how it might influence the course of the disease. A new study set out to explore this question by examining both adults and children who had been diagnosed with atopic dermatitis. Information was gathered through health records and a nationwide questionnaire that asked patients and caregivers about scratching behaviors and recent disease activity. The researchers were particularly interested in whether patients engaged in scratching without feeling itchy and whether they scratched in ways they did not even notice until it was pointed out to them. Disease severity was measured using a patient-focused tool designed to capture symptoms and their impact on daily life. The findings showed that habitual scratching was widespread in both children and adults. Many individuals described scratching even when they did not experience itch, while others reported scratching automatically without awareness. Importantly, these behaviors were more common in people whose atopic dermatitis was more severe. This suggests that unconscious scratching is not just a by-product of the disease but may be closely tied to its intensity and persistence. The researchers concluded that habitual scratching deserves more attention in the management of atopic dermatitis. Recognizing and addressing this behavior could help improve treatment outcomes, as ongoing scratching worsens inflammation and delays healing. They recommended that clinicians, patients, and caregivers work together to develop strategies for noticing and reducing unconscious scratching as part of comprehensive care.
Keywords:
Atopic dermatitis, habitual scratching, itch–scratch cycle, disease severity, pruritus, dermatology, skin barrier dysfunction, holistic care, Nakahara, T., Noto, S., Matsukawa,
Powered by WPeMatico

Researchers have found in a new randomized, triple-blinded clinical trial that silver diamine fluoride (SDF) was more effective in halting initial approximal caries lesions in adults during the first six months of treatment. This offers significant disease-control benefits for high-risk patients presenting with multiple early lesions, providing a minimally invasive option for managing dental decay.
The study, published in Journal of Conservative Dentistry and Endodontics (Jaradat et al., 2025), involved adults with early interproximal lesions who were randomly assigned to receive either SDF or a placebo. Lesions were evaluated at six- and twelve-month intervals using bitewing radiographs, digital subtraction radiography (DSR), and histogram analysis of subtraction radiographs (HA). Results showed that while over 90% of lesions in both groups were arrested over 12 months, the SDF-treated lesions performed significantly better during the first six months when assessed using DSR. By the 12-month mark, differences between the groups were no longer statistically significant, but the early benefit highlights SDF’s effectiveness in rapid intervention for lesion control.
What this really means is that SDF can serve as a simple, low-cost, and minimally invasive strategy for arresting early interproximal decay, particularly in adults at high risk for multiple lesions. By stopping the progression of early caries, dental practitioners can reduce the need for more invasive restorations and improve long-term oral health outcomes. The authors also note that while the short-term benefits are clear, further studies are needed to confirm sustained efficacy beyond a year and to explore optimized application protocols. For patients, this study reinforces the importance of early detection and treatment of interproximal lesions, which are often difficult to manage and frequently go unnoticed until more advanced decay develops. Clinicians may consider incorporating SDF into preventive care plans for high-risk adults to enhance early caries control and minimize future restorative needs.
Reference: Jaradat, M., Kolker, J., Owais, A., Guzman-Armstrong, S., Haes, A., Anamali, S., Comnick, C., Zeng, E., & Kanellis, M. (2025). Silver diamine fluoride effectiveness in arresting initial approximal caries lesions in adults: A triple-blinded, randomized controlled clinical trial. Journal of Conservative Dentistry and Endodontics, 28(9), 892–898. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12440336/
Keywords: silver diamine fluoride, approximal caries, minimal intervention, subtraction radiography, dental disease control, Jaradat, Journal of Conservative Dentistry and Endodontics.
Powered by WPeMatico
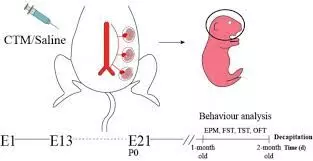
Findings from a new study show that selective serotonin reuptake inhibitor use during pregnancy and lactation may alter maternal caregiving behaviors but does not impair offspring cognition. Selective serotonin reuptake inhibitors, such as fluoxetine, are widely prescribed for the treatment of depression and anxiety in women of reproductive age, including during pregnancy. Concerns about potential risks for neurodevelopmental impairment in children have often complicated treatment decisions, leading to hesitation among patients and clinicians.
The study offers important clarification by indicating that while maternal behaviors related to caregiving may be influenced by exposure to selective serotonin reuptake inhibitors during the perinatal period, offspring cognitive abilities remain unaffected. Maternal caregiving encompasses essential interactions such as attentiveness, emotional responsiveness, and nurturing practices, all of which are critical for healthy child development.
Pharmacological modulation of serotonin systems during pregnancy may influence these behaviors, underscoring the importance of monitoring and supporting maternal-infant bonding in women undergoing pharmacological treatment. At the same time, the absence of measurable adverse effects on offspring learning, memory, and cognitive performance provides reassurance regarding long-term neurodevelopmental outcomes.
This distinction helps shift the clinical conversation from concerns about irreversible cognitive harm in children to a more practical focus on supporting maternal caregiving capacity. Untreated maternal depression itself carries significant risks, including reduced caregiving quality and poorer child outcomes, highlighting the necessity of balancing risks and benefits when considering treatment options. The findings encourage clinicians to take an integrative approach, combining pharmacological management with psychosocial support strategies that reinforce maternal caregiving behaviors. Further longitudinal research will be important to understand whether early behavioral changes in mothers translate into long-term psychosocial impacts on offspring.
Overall, the evidence suggests that selective serotonin reuptake inhibitors remain a viable therapeutic option during pregnancy, provided maternal support systems are emphasized as part of comprehensive perinatal care.
Keywords: selective serotonin reuptake inhibitors, fluoxetine, pregnancy, lactation, maternal caregiving, offspring cognition, perinatal depression, child development
Powered by WPeMatico

Jaipur: The Rajasthan Medical Services Corporation Limited (RMSCL) has imposed a ban on the distribution and use of a batch of cough syrup following reports of adverse reactions in Bharatpur and Sikar districts.
Patients reported alarming symptoms, including vomiting, drowsiness, anxiety, dizziness, restlessness, and even unconsciousness, after taking the medication.
Medical and Health Minister Gajendra Singh Khinvsar directed RMSCL to conduct an urgent probe and take immediate action upon receiving the complaints. Acting swiftly, RMSCL suspended the use of the Dextromethorphan HBr Syrup IP 13.5mg/5ml (Batch No. 440) pending test results.
Principal Secretary of the Medical and Health Department, Gayatri Rathore, confirmed that statutory samples were collected by Drug Control Officers and forwarded to the State Drug Testing Laboratory for quality analysis. She said further steps will be taken once the test results are available.
As per IANS, RMSCL has also ordered a ban on 19 other batches of the same drug supplied by the concerned manufacturer. RMSCL Managing Director Pukhraj Sain emphasised that strict quality control procedures are in place under the Chief Minister’s Free Medicine Scheme.
Every drug batch supplied is first tested in approved laboratories, and only medicines meeting prescribed standards are released for hospital use. If any batch fails, it is barred from distribution. In cases where complaints are received, drugs are retested at the State Drug Testing Laboratory to ensure public safety. Officials stressed that public health remains the government’s top priority and assured that necessary regulatory action will follow based on laboratory findings.
Patients have been advised to immediately discontinue use of the affected batches until further notice. The incident has raised concerns over drug safety standards, but authorities have reiterated their commitment to strict monitoring and swift corrective measures to protect patients.
A 5-year-old child died after reportedly consuming cough syrup supplied under the government’s free medicine scheme in Sikar district. The family alleged that the child, identified as Nityansh, stopped breathing immediately after taking the dose.
Similar incidents have surfaced in Srimadhopur and Bharatpur. In Sikar, three children reportedly fell ill after consuming the same cough syrup. In Bharatpur, even a doctor who examined the children later experienced health complications after consuming the medicine.
The most recent case occurred in Khori Brahmanan village of Sikar, where Nityansh’s family claims that the cough syrup provided at a government hospital was directly responsible for his sudden death.
Powered by WPeMatico
