Routine heart CT scanning not warranted after stenting for left main CAD: ESC Study
Madrid: Routine coronary computed tomography (CCT)-based follow-up after percutaneous coronary intervention (PCI) of the left main coronary artery did not reduce death, myocardial infarction (MI), unstable angina or stent thrombosis compared with symptom-based follow-up, according to late-breaking research presented in a Hot Line session today at ESC Congress 2025
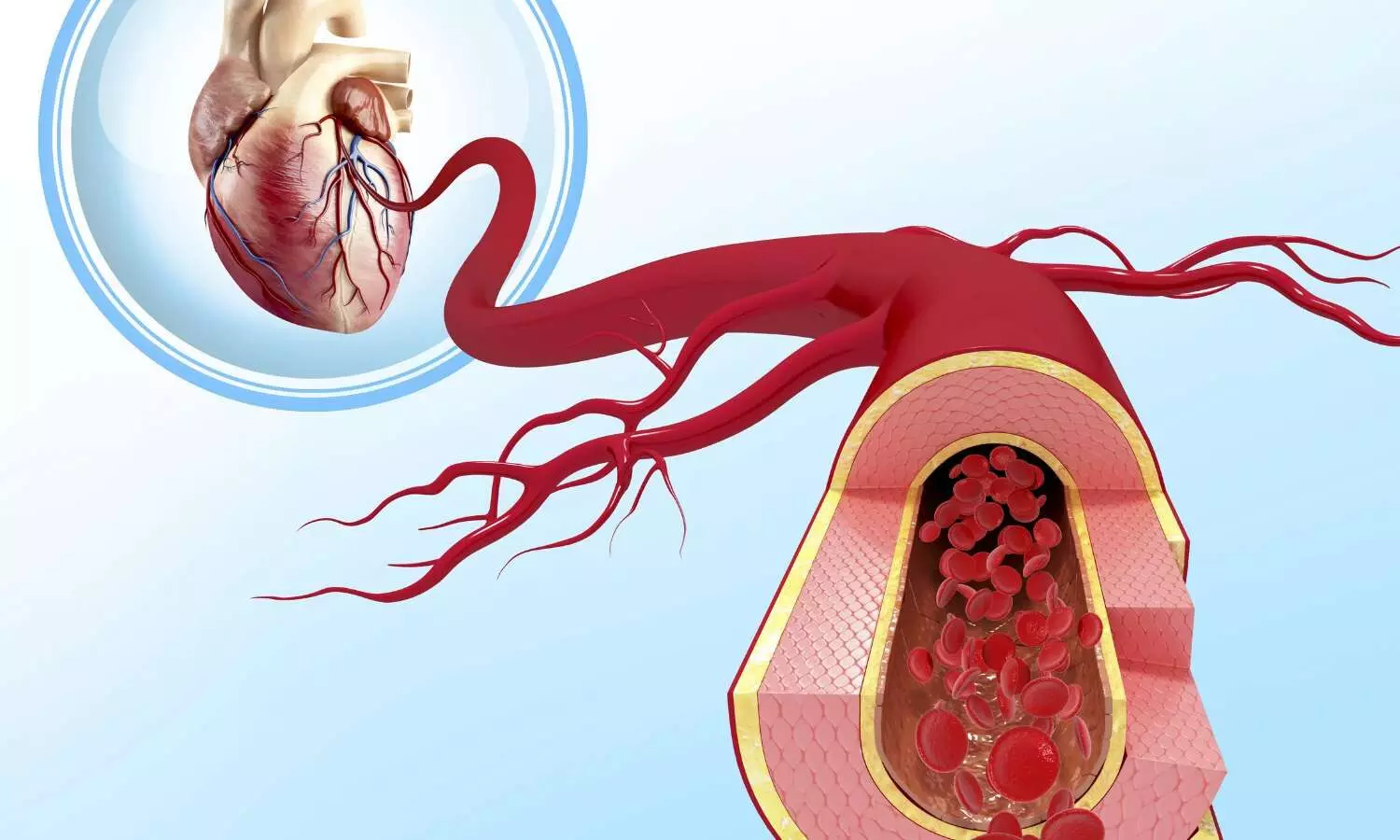
The left main coronary artery supplies a large proportion of the heart muscle and significant left main coronary artery disease is associated with high morbidity and mortality. The introduction of coronary stents along with the improvements in technology and pharmacological management has increased the use of PCI in these high-risk patients with similar results achieved compared with coronary artery bypass grafting.
“Detrimental complications, such as stent restenosis, and recurrent ischaemic events can occur after left main PCI; however, the optimal surveillance strategy remains a subject of debate,” explained trial presenter, Doctor Ovidio De Filippo from Hospital Citta Della Salute e della Scienza di Torino, Turin, Italy.
“In recent years, CCT has emerged as a valuable tool for diagnosis and monitoring, providing accuracy comparable to invasive angiography, while minimising procedural risks and reducing healthcare costs. We conducted the first randomised trial to evaluate the potential benefit of routine CCT-based follow-up at 6 months compared with standard symptom- and ischaemia-driven management in patients after PCI for left main disease.”
PULSE was an open-label, blinded-endpoint, investigator-initiated, randomised trial conducted at 15 sites in Europe and South America.
Participants were consecutive patients with critical stenosis undergoing PCI for left main coronary artery disease. Participants were randomised 1:1 to either a CCT-guided follow-up at 6 months (experimental arm) or standard symptom and ischaemia-driven management (control arm). Participants were followed for an additional 12 months (total follow-up 18 months).
In the CCT arm, if significant left main in-stent restenosis was detected, patients underwent invasive coronary angiography followed by target lesion revascularisation if in-stent restenosis was confirmed. If any significant stenosis was detected in a different site, management was conducted according to the current guidelines. In the standard-of-care arm, patients were managed per clinical guidelines and according to each centre’s standard practice. The primary endpoint was a composite of all-cause death, spontaneous MI, unstable angina or definite/probable stent thrombosis at 18 months.
A total of 606 patients were randomised who had a mean age of 69 years and 18% were female. CCT was performed in 89.8% of patients in the experimental arm at a median of 200 days.
A primary-endpoint event occurred in 11.9% of patients in the CCT arm and 12.5% of patients in the control arm at 18 months (hazard ratio [HR] 0.97; 95% confidence interval [CI] 0.76 to 1.23; p=0.80).
There was a reduced risk of spontaneous MI in the CCT arm vs. the control arm (0.9% vs. 4.9%; HR 0.26; 95% CI 0.07 to 0.91; p=0.004). An increase in imaging-triggered target-lesion revascularisation was observed in the CCT arm compared with the control arm (4.9% vs. 0.3%; HR 7.7; 95% CI 1.70 to 33.7; p=0.001); however, the incidence of clinically driven target-lesion revascularisation was similar between the arms (5.3% vs. 7.2%; HR 0.74; 95% CI 0.38 to 1.41; p=0.32).
Summing up the main findings, Principal Investigator, Professor Fabrizio D’Ascenzo, also from Hospital Citta Della Salute e della Scienza di Torino, said: “Systematic 6-month CCT-based follow-up did not result in a reduction in 18-month all-cause death, spontaneous MI, unstable angina and stent thrombosis. While universal CCT-based follow-up may not be useful, the marked reduction in spontaneous MI and identification of obstructive lesions requiring repeat PCI suggest this approach may be worth investigating further in selected patients with complex anatomies and over longer follow-up.”
Powered by WPeMatico