What actually happens in your brain when you change your mind?
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Canada: Women entering pregnancy with multiple chronic conditions (MCC) face significantly higher risks of severe maternal complications, including morbidity and mortality, according to a large population-based study from Ontario, Canada. The study also found that emergency department visits and hospitalizations were more frequent among these women, highlighting the need for tailored, multidisciplinary care.
The research, led by Hilary K. Brown from the Department of Health and Society, University of Toronto Scarborough, along with colleagues, was published in BJOG: An International Journal of Obstetrics & Gynaecology. The study analyzed data from females aged 13–54 years with recognized pregnancies between 2012 and 2021, examining how the presence and type of chronic conditions before conception influenced maternal health outcomes up to 42 days postpartum.
Using modified Poisson regression models adjusted for age, parity, income, rurality, and immigrant or refugee status, the team assessed the impact of the number of chronic conditions, complex MCC (defined as three or more conditions affecting at least three body systems), and co-occurring cardiometabolic conditions. The outcomes measured included perinatal emergency department (ED) use, hospitalizations, and severe maternal morbidity or mortality (SMM-M).
Based on the study, the researchers reported the following findings:
• The study analyzed 1,373,193 pregnancies.
• Among these, 894,042 women had no pre-pregnancy chronic conditions, 357,398 had one condition, 94,427 had two conditions, and 27,326 had three or more conditions.
• Maternal risk increased stepwise with the number of chronic conditions.
• Adjusted relative risks (aRR) for severe maternal morbidity or mortality (SMM-M) within 42 days postpartum were:
• 1.38 for women with one chronic condition
• 1.82 for women with two chronic conditions
• 2.75 for women with three or more chronic conditions
• Women with complex MCC (three or more conditions affecting at least three body systems) had an aRR of 2.92.
• Women with three or more cardiometabolic conditions had an aRR of 5.45.
• Emergency department visits increased with the number of chronic conditions, with women having three or more conditions showing a 1.86-fold higher risk.
• Hospitalizations were also higher, with a threefold increased likelihood for women with three or more chronic conditions compared with those without chronic conditions.
These findings emphasize that MCC, particularly when complex or cardiometabolic in nature, is strongly associated with adverse maternal health outcomes. The authors suggest that multidisciplinary, patient-centered care could help mitigate these risks and improve postpartum recovery.
The study also notes that MCC is socially patterned, disproportionately affecting individuals with lower socioeconomic status, which may amplify healthcare costs and mortality risks. Future research is needed to identify which socioeconomic factors influence these associations, as well as to evaluate a broader range of perinatal and extended postpartum outcomes to better support mothers with MCC and their infants.
“Overall, this study provides important evidence for healthcare providers, underscoring the necessity of preconception risk assessment and comprehensive care planning for women with multiple chronic conditions to reduce maternal complications and improve pregnancy outcomes.
Reference:
Brown, H. K., Fung, K., Cohen, E., Dennis, L., Grandi, S. M., Rosella, L. C., Varner, C., Vigod, S. N., Wodchis, W. P., & Ray, J. G. Multiple Chronic Conditions Before Pregnancy and Risk of Adverse Maternal Health Outcomes: Population-Based Cohort Study. BJOG: An International Journal of Obstetrics & Gynaecology. https://doi.org/10.1111/1471-0528.18347
Powered by WPeMatico
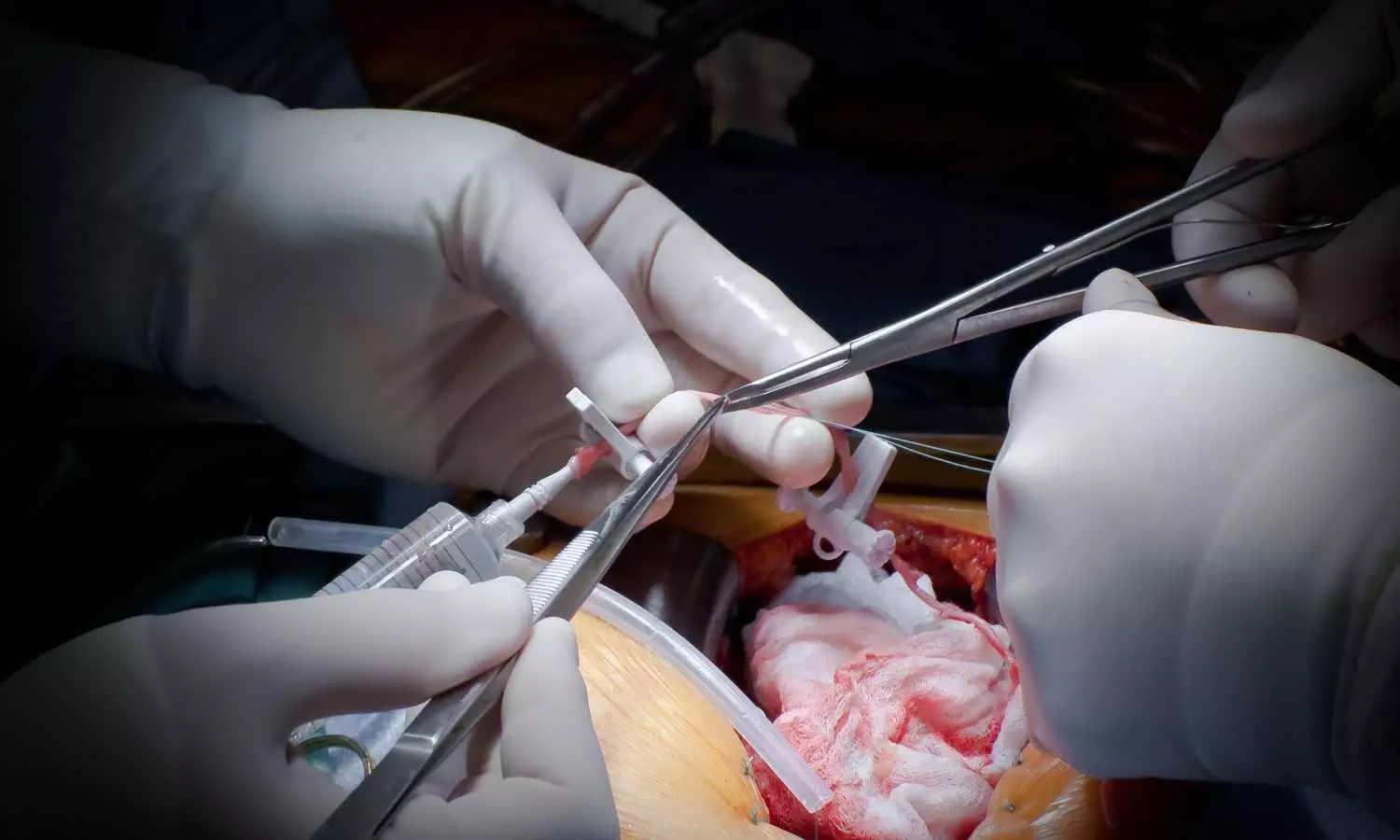
Compared with dual antiplatelet therapy (DAPT), a de-escalated DAPT strategy resulted in similar graft occlusion rates and reduced clinically relevant bleeding in patients who underwent coronary artery bypass grafting (CABG), according to late-breaking research presented in a Hot Line session today at ESC Congress 2025.
Saphenous vein grafts remain the most frequently used conduits in CABG; however, failure rates are high, with 3−12% occluding before hospital discharge and 8−25% failing at 1 year.
“After CABG, decreased risk of saphenous vein graft failure has been observed with 12 months of DAPT (aspirin plus a P2Y12 inhibitor) but this was accompanied by an increased risk of bleeding,3” explained Investigator of the TOP-CABG trial, Doctor Xin Yuan from the State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, National Center for Cardiovascular Diseases, Beijing, China.
“Rather than receiving DAPT for 12 months, a de-escalated strategy of DAPT for 1 or 3 months then aspirin monotherapy for 9 or 11 months is associated with similar ischemic benefits and better bleeding safety in patients after percutaneous coronary intervention (PCI). Mirroring PCI, the first 3 months after CABG surgery is a high-thrombotic-risk phase, but studies of de-escalated DAPT are lacking. Thus, we designed the TOP-CABG trial to compare the effects of de-escalated DAPT and DAPT on patency and bleeding events for 1 year after CABG.”
TOP-CABG trial was a double-blind, parallel-controlled randomised trial conducted at 13 hospitals in China. Patients older than 18 and younger than 80 years old were recruited if they were undergoing planned CABG for the first time with at least one saphenous vein graft. Patients were randomised 1:1 to de-escalated DAPT (ticagrelor 90 mg twice daily plus aspirin 100 mg once daily for 3 months, then placebo twice daily plus aspirin 100 mg once daily for 9 months) or to DAPT (ticagrelor 90 mg twice daily plus aspirin 100 mg once daily for 1 year).
The primary noninferior efficacy endpoint was 100% occlusion of the saphenous vein graft within 1 year after CABG at the per-graft level, with occlusion assessed by coronary computed tomography angiography or coronary angiography. The prespecified noninferiority margin was 3.5%. The primary superior safety endpoint was clinically relevant bleeding at the per-patient level (Bleeding Academic Research Consortium [BARC] classification ≥2) within 1 year.
The 2,290 patients included had a mean age of 61.5 years and 20.6% were female.
Noninferiority was demonstrated for the primary efficacy endpoint of graft occlusion, which occurred in 10.79% of patients’ grafts in the de-escalated DAPT group and 11.19% in the DAPT group (difference −0.31%; 95% confidence interval [CI] −3.13 to 2.52; p=0.008). The primary safety endpoint of clinically relevant bleeding was less frequent with de-escalated DAPT vs. DAPT (8.26% vs. 13.19% of patients; HR 0.62; 95% CI 0.48 to 0.81; p<0.001).
There was no difference between the groups for secondary outcomes including graft failure, any graft stenosis, any graft occlusion or major adverse cardiac and cerebrovascular events.
Doctor Yuan concluded: “In the largest CABG trial to date, a de-escalation strategy offered a better balance between graft patency protection and bleeding risk than DAPT. These findings may help to inform future guidelines regarding the benefits of a shorter period of DAPT during the early phase after CABG.”
Powered by WPeMatico

Taiwan: Children exposed to daily incense burning or those who had recently taken antibiotics face a significantly higher risk of developing acute bacterial paranasal sinusitis (ABPS), according to a recent study published in BMC Infectious Diseases. The research, led by Ting-Fang Chiu and colleagues from the Department of Pediatrics at Taipei City Hospital, highlights key environmental and medical factors contributing to this common pediatric infection.
Powered by WPeMatico
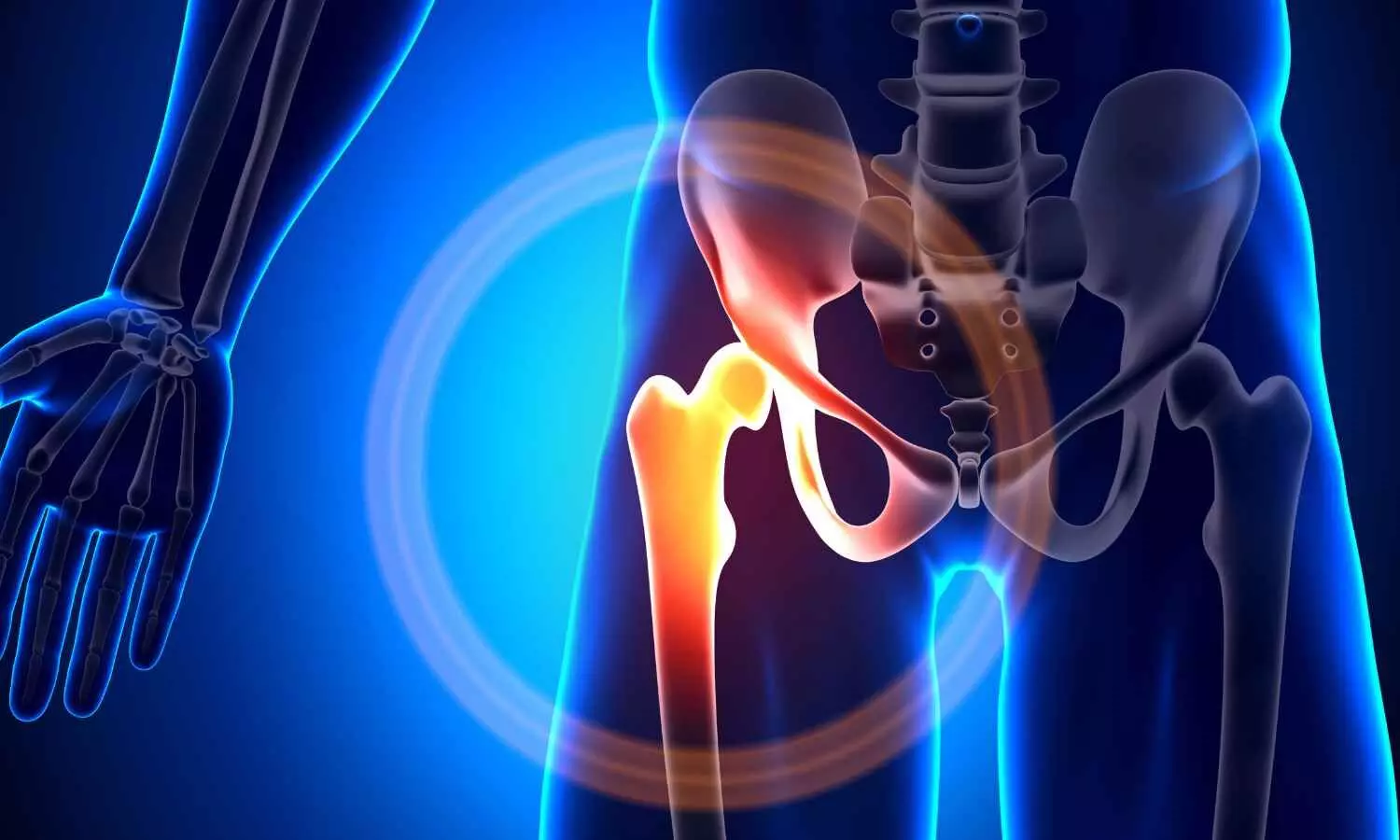
A new study published in the journal of BMC Surgery revealed that longer waiting times before hip fracture surgery were linked to higher 30-day mortality risk in elderly patients, with a threshold of around 42 hours marking significantly increased risk.
This study from the Affiliated Kunshan Hospital of Jiangsu University conducted a retrospective cohort study of 818 patients aged 65 and older who underwent surgery for hip fractures between January 2017 and July 2022. The study examined patient outcomes relative to surgical delays, highlights the importance of timely surgical intervention to improve survival chances in older individuals.
The study evaluated a broad range of clinical and demographic factors. These included patients’ age, gender, body mass index (BMI), type of hip fracture, surgical procedure performed, anesthesia risk (measured by American Society of Anesthesiologists score), operation time, month and week of hospital admission, and key laboratory test results. By controlling for these covariates through logistic regression analysis, this study isolated the independent effect of waiting time on 30-day mortality.
The analysis demonstrated a clear positive association between waiting time and the risk of death within 30 days of surgery. Specifically, the results indicated that every additional 10 hours of surgical delay was linked to a 13.6% increase in 30-day mortality (odds ratio [OR] 1.136; 95% confidence interval [CI], 1.027–1.256; P = 0.0136).
The relationship between waiting time and mortality was not linear. Statistical modeling revealed a threshold effect, when the waiting period was less than 42.4 hours, there was no detectable increase in 30-day mortality risk.
However, delays beyond 42.4 hours were associated with a sharply elevated risk of death. This nonlinear pattern emphasizes that while minor surgical delays may not be fatal, longer postponements can have serious, life-threatening consequences.
The findings carry significant implications for hospitals and healthcare policymakers. In many clinical settings, delays in hip fracture surgery occur due to resource constraints, patient stabilization needs, or scheduling bottlenecks. The evidence from this study suggests that efforts to reduce waiting times could markedly improve survival outcomes in elderly patients.
Overall, the study highlights the urgent need to treat hip fractures in older adults as a medical emergency requiring prompt surgical intervention. The identified threshold of 42 hours may serve as a clinical benchmark for prioritizing surgical scheduling and optimizing patient outcomes.
Source:
Xu, M.-Z., Lu, K., Ye, Y.-W., Xu, S.-M., Shi, Q., Gong, Y.-Q., & Li, C. (2025). Waiting time and 30-day mortality association in elderly patients having hip fracture surgery. BMC Surgery, 25(1). https://doi.org/10.1186/s12893-025-03140-z
Powered by WPeMatico

USA: A secondary analysis of the AZALEA-TIMI 71 randomized clinical trial, recently published in JAMA Cardiology, has highlighted the potential safety benefits of abelacimab, a novel factor XI inhibitor, compared with rivaroxaban in patients with atrial fibrillation (AF). The findings suggest that abelacimab may offer a more favorable bleeding profile across varying levels of kidney function, including in those with impaired renal health.
Powered by WPeMatico

Cornell researchers have uncovered the genetic triggers that cause male and female bovine embryos to develop differently, as early as seven to eight days after fertilization. The breakthrough in basic science has implications for human health – such as drug development and in vitro fertilization – and for bovine health and dairy industry sustainability.
Scientists have known since the 1990s that male embryos of multiple mammalian species, including humans, grow faster than female embryos, but until now, the underlying reasons were unclear.
In a new paper, published Aug. 27 in Cell & Bioscience, Cornell scientists grew bovine embryos in petri dishes then analyzed their genetic sex and RNA sequencing, which shows how genes are being expressed. They discovered significant sex differences in gene regulation: Male embryos prioritized genes associated with energy metabolism, causing them to grow faster than their female counterparts. Female embryos emphasized genes associated with sex differentiation, gonad development and inflammatory pathways that are important for future development.
Understanding these fundamental sex differences at the genomic and molecular levels is critically important to improving in vitro fertilization (IVF) success in humans and cows, and in developing treatments that will work for both men and women, said Jingyue “Ellie” Duan, assistant professor of functional genomics in the College of Agriculture and Life Sciences and paper co-author. Co-first authors are Meihong Shi, a postdoctoral associate, and Guangsheng Li, a Ph.D. candidate, both in Duan’s lab.
“Sex difference has been a factor ignored in a lot of studies and clinical trials. Until very recently, most mouse studies have used exclusively male mice. And most drug discovery is done with male mice,” Duan said. “And yet, we see that onset and occurrence of many diseases are different in men and women: Alzheimer’s, autoimmune diseases, heart disease. In this basic study, we found that male and female embryos are different, even at this very early stage, on the basis of genome regulation.”
At this early stage, sex-associated hormones like estrogen and testosterone – which contribute to average size differences between male and female adults – have not yet come into play. Advances in genome sequencing technology enabled researchers to revisit the question at a genome-wide level, Duan said.
“This could imply that there’s an intrinsic factor in our genome contributing to the sex-based differences we see, such as sex chromosomes (XX versus XY) or sex-linked genes, not just from hormonal change or environmental factors,” Duan said. “We’re born with this sex-specific genetic regulation that is contributing very differently to cellular behavior, disease onset and immune system development, and continues through life all the way to health and aging. That’s a very important message for people in the clinical field and people developing drugs to understand.”
Bovines are an effective animal model for human-health studies, but bovine research is also important for its role in supporting food supplies and sustainable agriculture. Understanding and optimizing bovine reproduction is especially important for the dairy industry, which relies on cattle reproduction through IVF to maintain milk supplies.
Duan’s lab collaborated in this research with the lab of Soon Hon Cheong, Ph.D. ’12, associate professor of clinical sciences in the College of Veterinary Medicine. The project would not have been possible without collaboration between Duan’s genomics-focused lab and Cheong’s group, which studies reproductive medicine and assisted reproductive techniques, Duan said.
Future research, already underway in both labs, will expand this work by studying sex differences in embryos from fertilization through day eight after fertilization.
Reference:
Shi, M., Li, G., Araujo, H.M. et al. Sex-biased transcriptome in in vitro produced bovine early embryos. Cell Biosci 15, 123 (2025). https://doi.org/10.1186/s13578-025-01459-x
Powered by WPeMatico

Beta blockers-drugs commonly prescribed for a range of cardiac conditions, including heart attacks-provide no clinical benefit for patients who have had an uncomplicated myocardial infarction with preserved heart function. Beta blockers have been the standard treatment for these patients for 40 years.
This is a breakthrough discovery from the “REBOOT Trial” with senior investigator Valentin Fuster, MD, PhD, President of Mount Sinai Fuster Heart Hospital and General Director of Spain’s Centro Nacional de Investigaciones Cardiovasculares (CNIC). The study results, which could overturn a standard treatment paradigm, were presented on Saturday, August 30, during a “Hot Line” session at the European Society of Cardiology Congress in Madrid, and simultaneously published in The New England Journal of Medicine.
Additionally, a REBOOT substudy, published Saturday, August 30, in the European Heart Journal, shows that women treated with beta blockers had a higher risk of death, heart attack, or hospitalization for heart failure compared to women not receiving the drug. Men did not have this increased risk.
“This trial will reshape all international clinical guidelines. It joins other previous landmark trials led by CNIC and Mount Sinai-such as SECURE with the polypill and DapaTAVI, with SLT2 inhibition associated to TAVI-that have already transformed some global approaches to cardiovascular disease,” says Dr. Fuster.
The SECURE trial showed a polypill, a single pill that that combines three medications – which contains aspirin, ramipril, and atorvastatin – reduces cardiovascular events by 33 percent in patients treated with this after a heart attack. The DapaTAVI trial showed both dapagliflozin and the related medication empagliflozin – drugs used to treat diabetes- improves the prognosis of patients with aortic stenosis treated by transcatheter aortic valve implantation.
“REBOOT will change clinical practice worldwide,” says Principal Investigator Borja Ibáñez, MD, CNIC’s Scientific Director, who presented the results. “Currently, more than 80 percent of patients with uncomplicated myocardial infarction are discharged on beta blockers. The REBOOT findings represent one of the most significant advances in heart attack treatment in decades.”
Although generally considered safe, beta blockers can cause side effects such as fatigue, bradycardia (low heart rate), and sexual dysfunction. For more than 40 years, beta blockers have been prescribed as a standard treatment after a heart attack, but their benefit in the context of modern treatments was unproven. The REBOOT trial, is the largest clinical trial on this subject. The international study was coordinated by CNIC in collaboration with the Mario Negri Institute for Pharmacological Research in Milan.
Researchers enrolled 8,505 patients across 109 hospitals in Spain and Italy. Participants were randomly assigned to receive or not receive beta blockers after hospital discharge. All patients otherwise received the current standard of care and were followed for a median of nearly four years. The results showed no significant differences between the two groups in rates of death, recurrent heart attack, or hospitalization for heart failure.
A REBOOT subgroup analysis found that women treated with beta blockers experienced more adverse events. Results show women treated with beta-blockers had a 2.7 percent higher absolute risk of mortality compared to those not treated with beta-blockers during the 3.7 years of follow-up of the study. The elevated risk when treated with beta-blockers was restricted to women with a complete normal cardiac function after a heart attack (left ventricular ejection fraction of 50 percent or higher). Those with a mild deterioration in cardiac function did not have an excess risk of adverse outcomes when treated with beta-blockers.
“After a heart attack, patients are typically prescribed multiple medications, which can make adherence difficult,” explains Dr. Ibáñez. “Beta blockers were added to standard treatment early on because they significantly reduced mortality at the time. Their benefits were linked to reduced cardiac oxygen demand and arrhythmia prevention. But therapies have evolved. Today, occluded coronary arteries are reopened rapidly and systematically, drastically lowering the risk of serious complications such as arrhythmias. In this new context—where the extent of heart damage is smaller-the need for beta blockers is unclear. While we often test new drugs, it’s much less common to rigorously question the continued need for older treatments.”
That was the motivation behind REBOOT.
“The trial was designed to optimize heart attack care based on solid scientific evidence and without commercial interests. These results will help streamline treatment, reduce side effects, and improve quality of life for thousands of patients every year,” Dr. Ibanez adds.
Reference:
Borja Ibanez, Roberto Latini, Xavier Rossello, Beta-Blockers after Myocardial Infarction without Reduced Ejection Fraction, New England Journal of Medicine, DOI: 10.1056/NEJMoa2504735.
Powered by WPeMatico
