Gestational diabetes linked to cognitive decline in mothers, increased risk of neurodevelopmental disorders in children
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

A new study published in the journal of Pediatric Allergy and Immunology revealed that greater dietary diversity during pregnancy was associated with a reduced risk of atopic dermatitis in early childhood. The findings of the study emphasize on the potential protective role of maternal nutrition.
The research followed 677 mother-infant pairs from pregnancy through the children’s first 3 years, examined how maternal dietary diversity influenced the development of atopic dermatitis, while also considering the role of the infant gut microbiome.
To assess diet quality, this study used the Minimum Dietary Diversity for Women (MDD-W) guideline developed by the Food and Agriculture Organization. This measure evaluates whether a mother consumes foods from a broad range of groups, including whole grains, proteins, dairy, fruits, and vegetables, during pregnancy. Infant gut microbiota was analyzed at 2 months postpartum, and the incidence of atopic dermatitis in the children was monitored up to age three.
Also, while maternal diet did not appear to influence the overall diversity of the infant gut microbiome (alpha and beta diversity) it did alter its composition. The study highlighted 2 bacterial genera namely Rothia and Parabacteroides, both of which were linked to reduced risk of atopic dermatitis when present in greater abundance.
The analysis also revealed a connection between maternal nutrient intake and microbiome composition. Vitamin A-rich fruits and vegetables, like carrots, sweet potatoes, and leafy greens, were linked to higher levels of the Parabacteroides genus, which suggests a potential pathway through which maternal diet supports infant immune resilience.
The mothers with the lowest dietary diversity had the highest rates of children developing the condition, whereas the individuals with the broadest food group intake showed markedly lower incidence. Additional data demonstrated that while microbiome diversity metrics (alpha and beta diversity) were not significantly different across groups, shifts in microbial composition were consistently observed in association with maternal diet quality.
Overall, the findings suggest that maternal dietary diversity during pregnancy may help protect against atopic dermatitis in children, possibly through modulation of the infant gut microbiome. However, further studies are required to confirm these findings and clarify the biological mechanisms involved.
Source:
Huynh, L. B. P., Fan, H.-Y., Huang, S.-Y., Nam, N. N., Nguyen, T. T., & Chen, Y.-C. (2025). Influence of maternal dietary diversity during pregnancy on infant atopic dermatitis: Exploring the microbiome link in a Taiwanese birth cohort. Pediatric Allergy and Immunology: Official Publication of the European Society of Pediatric Allergy and Immunology, 36(9),. https://doi.org/10.1111/pai.70200
Powered by WPeMatico
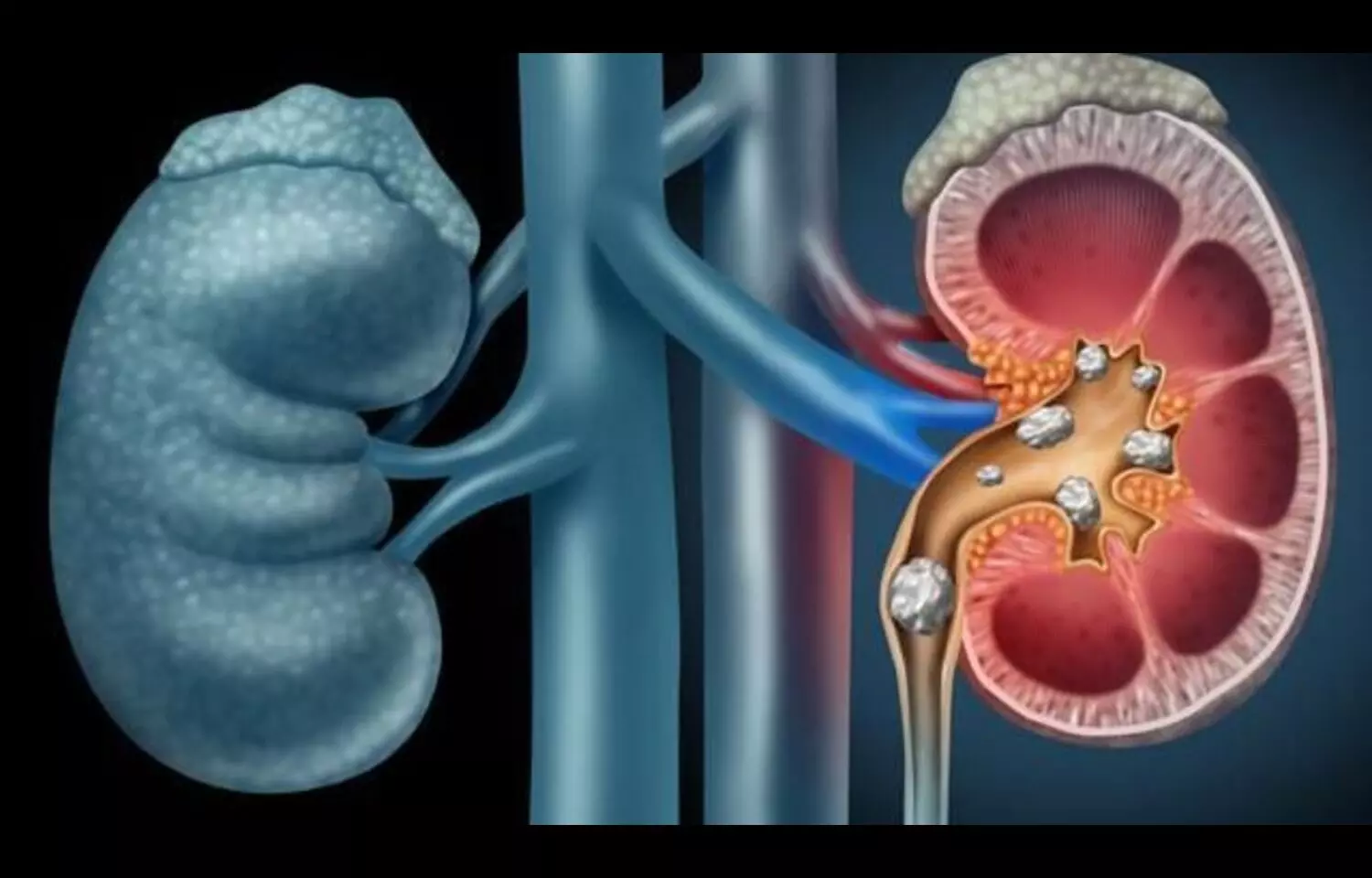
Kidney stone disease remains a growing health concern worldwide, with metabolic, inflammatory, and lifestyle factors all contributing to risk. New research now suggests that individuals with rheumatoid arthritis (RA) may be particularly vulnerable.
In a large population-based study involving nearly 20,000 participants, researchers found that patients with RA experienced more than double the incidence of kidney stones compared to those without the condition. The association persisted even after adjusting for common risk factors such as age, sex, and comorbidities, highlighting a potential link between systemic inflammation and stone formation. Rheumatoid arthritis is a chronic autoimmune disease characterized by persistent joint inflammation and systemic immune dysregulation. Researchers propose several possible mechanisms that could explain the elevated risk of nephrolithiasis in RA patients. Chronic inflammation may alter calcium and uric acid metabolism, leading to increased urinary excretion and crystal deposition. Additionally, medications frequently used in RA management—such as corticosteroids and diuretics—may contribute to stone formation by influencing fluid balance and renal handling of minerals. Reduced physical activity and dietary modifications in RA patients could also indirectly affect risk. Importantly, the study’s design limited causal inference. While the findings underscore a significant association, they do not establish that RA directly causes kidney stones. Instead, the results suggest that RA may act as a clinical marker of increased susceptibility, requiring further mechanistic and longitudinal research to clarify causality. Clinically, these findings carry important implications. Physicians caring for RA patients should be aware of the heightened risk of nephrolithiasis and consider proactive monitoring, especially in individuals with additional metabolic risk factors. Lifestyle strategies such as hydration, balanced diets, and metabolic screening may help mitigate risks. Overall, the study highlights the broader systemic burden of RA beyond joint disease, adding kidney stones to the list of potential comorbidities requiring integrated care.
Reference:
Yue, G., Yan, Y., Zeng, X. et al. Association between rheumatoid arthritis and kidney stones: A cross-sectional study of NHANES 2007–2020. Arthritis Res Ther 27, 141 (2025). https://doi.org/10.1186/s13075-025-03604-w
Powered by WPeMatico

A recent study published in the Journal of the American Medical Association found biparametric MRI to performs just as well as the current gold-standard multiparametric MRI in detecting clinically significant prostate cancer. The findings could reshape global diagnostic practices, particularly in health systems struggling with capacity and cost constraints.
Multiparametric MRI has long been considered the standard for diagnosing prostate cancer, combining T2-weighted, diffusion-weighted, and dynamic contrast–enhanced (DCE) sequences. While highly effective, this approach is resource-intensive and relies on gadolinium-based contrast, raising both logistical and financial barriers. Biparametric MRI excludes the DCE sequence and offers a faster and less costly alternative.
From April 2022 to September 2023, this trial enrolled 555 biopsy-naive men with elevated prostate-specific antigen (PSA) levels or abnormal digital rectal exams. Conducted across 22 centers in 12 countries, the study analyzed data from 490 participants after exclusions. The men, with a median age of 65 years and median PSA of 5.6 ng/mL, underwent both biparametric and multiparametric MRI. The radiologists first reported on biparametric scans without access to DCE data, then assessed the full multiparametric images.
If either imaging modality suggested clinically significant cancer, patients received targeted biopsies, with or without additional systematic sampling. The trial was designed to test whether biparametric MRI was “noninferior” to multiparametric MRI, with a 5% margin set for acceptable difference.
The study found biparametric MRI help identify cancer in 29.2% of men (143 out of 490) while multiparametric MRI detected it in 29.6% (145 out of 490). The difference was a mere −0.4 percentage points, statistically insignificant and well within the noninferiority margin.
Detection rates of clinically insignificant cancers were also nearly identical. Biparametric MRI flagged 9.2% of men, when compared with 9.6% for multiparametric scans. Also, central quality control showed that 99% of all scans were diagnostically adequate, highlighting the reliability of the abbreviated technique.
With approximately 4 million prostate MRIs performed worldwide each year, the shift to biparametric imaging could free up scanner time, shorten waiting lists, and reduce costs without compromising care. Overall, the findings suggest that, provided imaging quality is maintained, biparametric MRI has the potential to become the new global standard in prostate cancer diagnosis.
Reference:
Ng, A. B. C. D., Asif, A., Agarwal, R., Panebianco, V., Girometti, R., Ghai, S., Gómez-Gómez, E., Budäus, L., Barrett, T., Radtke, J. P., Kesch, C., De Cobelli, F., Pham, T., Taneja, S. S., Hu, J. C., Tewari, A., Rodríguez Cabello, M. Á., Dias, A. B., Mynderse, L. A., … PRIME Study Group Collaborators. (2025). Biparametric vs multiparametric MRI for prostate cancer diagnosis: The PRIME diagnostic clinical trial. JAMA: The Journal of the American Medical Association. https://doi.org/10.1001/jama.2025.13722
Powered by WPeMatico
A recent study published in the journal of Eye revealed that low hemoglobin levels may significantly raise the risk of developing diabetic retinopathy (DR). The findings highlight hemoglobin as an overlooked but potentially modifiable risk factor in managing type 2 diabetes.
The research used the TriNetX network from 2010 to 2022 and analysed data from over 57,000 adults aged 45 years and older with type 2 diabetes. The participants were divided into a low hemoglobin (LHB) group, defined as 8–12 g/dL, and a control group with levels ≥12 g/dL. To ensure balanced comparisons, propensity score matching was employed to account for confounding factors such as age, sex, and comorbidities.
The study tracked the onset of new DR cases within a 6 to 36 month follow-up period. The results showed a striking increase in risk among the individuals with lower hemoglobin. Specifically, the LHB group underwent a 33% higher risk of developing overall DR when compared with controls. When broken down into subtypes, the risk of proliferative DR was nearly doubled (HR: 1.95). Non-proliferative DR, a less severe but still concerning stage, also showed a modest yet significant risk increase of 19% (HR: 1.19).
The study found that even mild reductions in hemoglobin (10–12 g/dL) were enough to elevate DR risk, suggesting that attention should not be limited to only severe anemia cases. Subgroup analysis shed further light on this relationship. The association between low hemoglobin and DR was stronger in patients without hypertension (HR: 1.58 vs. 1.21 in hypertensive individuals).
It also remained consistent regardless of blood sugar control, as measured by HbA1c, highlighting hemoglobin as an independent factor. Also, men appeared more vulnerable than women, showing a more pronounced association.
Overall, these findings have important implications for clinical practice. While blood glucose and blood pressure management remain cornerstones of diabetes care, the study suggests that routine monitoring and optimisation of hemoglobin levels could play a critical role in preventing sight-threatening complications.
Source:
Hung, K.-C., Chang, L.-C., Chang, Y.-J., Hsu, C.-W., Yew, M., Wu, J.-Y., & Chen, I.-W. (2025). Association between haemoglobin levels and the risk of diabetic retinopathy in adults with type 2 diabetes: a retrospective cohort study using the TriNetX network. Eye, 1–8. https://doi.org/10.1038/s41433-025-03982-0
Powered by WPeMatico

A simple fitness tracker might hold the key to revolutionizing maternal healthcare. Scientists at Scripps Research have found preliminary evidence suggesting that common wearable devices such as the Apple Watch, Garmin and Fitbit could remotely monitor pregnancy-related health changes by tracking physiological patterns-like heart rate-that correlate with hormonal fluctuations.
“Wearable devices offer a unique opportunity to develop innovative solutions that address the high number of adverse pregnancy outcomes in the U.S.,” says co-senior author Giorgio Quer, the director of artificial intelligence and assistant professor of Digital Medicine at Scripps Research. “Our results show that signals collected via wearable sensors follow the expected changes in hormone levels and can detect unique patterns specific to live birth pregnancies, potentially allowing the monitoring of maternal health throughout the pregnancy and postpartum.”
The findings, released in the Lancet eBioMedicine on August 28, 2025, come at a crucial time for maternal health in the U.S. More than 2 million women of childbearing age live in maternal care deserts, or areas with severely limited access to obstetric care. Pregnancy complications, including miscarriage and preterm birth, continue to pose significant risks to maternal and child health, demanding more effective ways to monitor and address these outcomes.
To gather the data, the team used PowerMom , a bilingual digital research platform, which allowed participants to voluntarily report real-world data from their personal wearable devices after providing informed consent—capturing valuable information beyond the traditional prenatal clinic visits. The researchers enrolled over 5,600 participants who explicitly agreed to share their data and selected 108 individuals who had consented to provide data from three months before their pregnancy through six months after delivery. Using sophisticated statistical methods to identify population-level patterns, the team could account for individual differences and device variations.
From this data, the scientists were able to identify physiological patterns that aligned with the fluctuation of key pregnancy hormones such as estrogen, progesterone and human chorionic gonadotropin (hCG). The fluctuations of these hormones are critical to healthy pregnancy outcomes and provide insight into the pregnancy’s progression.
The heart rate data was particularly compelling. During early pregnancy, researchers found that the individual’s heart rate initially decreased around weeks five to nine, then steadily increased until about eight or nine weeks before delivery, reaching peaks up to 9.4 beats per minute above pre-pregnancy levels. After birth, the heart rate dropped below baseline levels before stabilizing around six months postpartum. The researchers also tracked sleep and activity patterns throughout pregnancy.
To validate this correlation, the team compared wearable sensor patterns with published hormone-level data from previous pregnancy studies, creating detailed models that predicted heart rate changes based on expected hormonal fluctuations throughout pregnancy. While these findings are still early, they demonstrate that wearables could potentially enhance prenatal care, particularly for women living in maternal care deserts.
“Hormones play a key role in pregnancy outcomes,” explains co-senior author Tolúwalàṣẹ Àjàyí, co-senior author and principal investigator of PowerMom. “Discovering the association between heart rate and hormone changes could unlock new ways to predict the beginning of pregnancy or identify signs of adverse outcomes such as gestational diabetes or preeclampsia.”
In an exploratory analysis of a small number of cases, pregnancies ending in adverse outcomes like miscarriage or stillbirth showed different heart rate patterns compared to healthy pregnancies, though more research with larger sample sizes is needed to validate these observations.
This research represents a significant step toward making pregnancy monitoring more accessible through technology that many individuals already own and use. By transforming consumer devices into medical monitoring tools, the approach could help bridge healthcare gaps and provide continuous oversight for high-risk pregnancies.
The digital approach builds on growing evidence that wearable devices can detect meaningful health changes much earlier.Previous work has shown their role in identifying COVID-19 infections and other health conditions through physiological pattern recognition.
The researchers plan to expand their analysis with a focus on understanding how patterns may vary across different demographic groups, geographic regions and socioeconomic backgrounds. They hope to eventually develop models that could identify birthing individuals who might benefit from additional monitoring or support.
“We want to understand if these patterns are consistent across subgroups based on age and access to care,” says first author and UC San Diego graduate student, Giulia Milan, who conducted this study in collaboration with Scripps Research. “Our goal is to determine whether this approach could eventually contribute to more personalized pregnancy care.”
Future studies will need to investigate whether physiological changes captured by wearables could potentially support clinical decision-making and patient care. The team also plans to collect both wearable data and blood samples from the same participants to directly validate the hormone-heart rate associations observed in this preliminary analysis.
Powered by WPeMatico

In a new study, artificial intelligence matched and potentially exceeded the performance of gastroenterologists and conventional scoring in evaluating endoscopies of Crohn’s disease patients.
The results, published in Clinical Gastroenterology and Hepatology, show a computer vision model identified mucosal ulceration as accurately as physician reviewing videos, while also being strongly correlated with the most common endoscopic scoring system.
“A clinician has a gestalt of whether someone’s Crohn’s is mild or severe, if it’s improving or worsening,” said Ryan W. Stidham, M.D., M.S., associate professor of internal medicine at the University of Michigan Medical School and senior author of the paper.
“But the manual tools to quantify that expert opinion with objectivity and reproducibly are poor. AI image analysis can provide better solutions for more precise measurements and descriptions of what we are seeing on the screen during colonoscopy.”
In the study, two gastroenterologists annotated ulcer areas in 4,487 still images from endoscopic videos. The computer vision AI model reviewed the same images, from previous clinical trials.
The AI model’s results had a higher overall DICE similarity score with ground truth (.591) than when comparing the agreement between two gastroenterologists (.462).
Computer vision assessments of the colonoscopy videos were also strongly correlated with Simple Endoscopic Score for Crohn’s Disease (SES-CD) values. SES-CD is a metric that attempts to manually quantify various characteristics of a patient’s ulceration.
While study authors note the importance of SES-CD for Crohn’s disease research and assessing the effectiveness of treatment, they also highlight its limitations, including variability among observers and inability to capture certain ulcer features.
Researchers hope that AI-powered metrics will not only improve consistency between providers but more importantly may offer more quantitative detail to describe disease.
“It can be hard to justify decisions, particularly if you’re talking about expensive drugs or riskier therapies,” Stidham said.
“One of the reasons for this research is to one day provide more objective evidence for an experienced clinician’s impression.”
Researchers identify several other potential advantages to more consistent endoscopy metrics. In areas without IBD specialists AI endoscopy interpretation may be used to guide treatment change based on expert decision making. For more experienced providers, the information can help them understand their own decision-making process.
They also highlight possible implications for education and drug development.
“This paper is really the first step, and I hope that it gets the entire field thinking of better ways to quantify IBD that more completely describe an individual patient,” Stidham said.
“It’s very early, but computer vision tools like this may provide an important component for the future of automated care, where AI and experts work together in treating patients.”
Reference:
Cai, Lingrui et al., Artificial Intelligence for Quantifying Endoscopic Mucosal Ulceration in Crohn’s Disease, Clinical Gastroenterology and Hepatology, DOI:10.1016/j.cgh.2025.05.026
Powered by WPeMatico

Australia: Children born to mothers with hypertensive disorders of pregnancy face a heightened risk of cognitive and developmental challenges, according to a large systematic review and meta-analysis published in PLOS Medicine. The research shows that while links to autism and global developmental delay diminish when factors such as birthweight and gestational age are considered, a measurable reduction in average IQ persists, underscoring the importance of early monitoring and support for these children.
Powered by WPeMatico

Chronic diabetic wounds, including diabetic foot ulcers, are a significant burden for patients, as impaired blood vessel growth hinders the healing process. A recent breakthrough offers hope by combining small extracellular vesicles (sEVs) loaded with miR-221-3p and a GelMA hydrogel to target thrombospondin-1 (TSP-1), a protein that suppresses angiogenesis. This new bioactive wound dressing not only accelerates healing but also promotes blood vessel formation, offering a promising new approach to treating one of the most challenging complications of diabetes.
Diabetic wounds, particularly foot ulcers, are notorious for their slow and often incomplete healing due to reduced blood flow and endothelial cell dysfunction. One of the major contributors to this issue is thrombospondin-1 (TSP-1), which inhibits the growth of new blood vessels, a process crucial for tissue repair. Despite various existing treatments, the challenge of addressing this barrier to healing remains unmet. With the global rise in diabetes cases, new treatments targeting the underlying causes of delayed wound healing have become a critical area of research. In light of these ongoing challenges, this study explores a new approach to stimulate angiogenesis and speed up the healing process.
In a new study (DOI: 10.1093/burnst/tkaf036) published in Burns & Trauma, a team of researchers from leading Chinese institutions has unveiled a novel therapeutic solution for diabetic wound healing. The study introduces an innovative wound dressing that combines miR-221OE-sEVs—engineered extracellular vesicles that target and reduce TSP-1 levels—with a GelMA hydrogel to create a sustained-release system. This cutting-edge approach has shown to significantly enhance wound healing and blood vessel formation in diabetic mice, offering hope for more effective treatments in the future.
In their study, the researchers discovered that high glucose conditions commonly found in diabetic wounds lead to increased levels of TSP-1 in endothelial cells, impairing their ability to proliferate and migrate—key processes for angiogenesis. By utilizing miR-221-3p, a microRNA that targets and downregulates TSP-1 expression, they restored endothelial cell function. The engineered miR-221OE-sEVs were encapsulated within a GelMA hydrogel, ensuring a controlled release at the wound site, mimicking the extracellular matrix. In animal trials, this composite dressing dramatically accelerated wound healing, with a notable increase in vascularization and a 90% wound closure rate within just 12 days, compared to slower healing in control groups.
Dr. Chuan’an Shen, a key researcher in the study, shared his excitement about the potential impact of this innovation: “Our results demonstrate the power of combining advanced tissue engineering with molecular biology. By targeting TSP-1 with miR-221OE-sEVs encapsulated in GelMA, we’ve not only improved endothelial cell function but also ensured a sustained and localized therapeutic effect. This breakthrough could revolutionize how we approach diabetic wound care, with the potential to improve patients’ quality of life significantly.”
The success of this engineered hydrogel in diabetic wound healing opens up several exciting possibilities. Beyond diabetic foot ulcers, the technology could be adapted for use in treating other chronic wounds, such as those caused by vascular diseases, or even in regenerating tissues like bone and cartilage. As further research and clinical trials progress, the promise of combining miRNA-based therapies with biocompatible hydrogels could become a cornerstone in regenerative medicine, offering patients more efficient and lasting wound healing solutions.
Reference:
Yan Cong, Sheng Meng, Xiaoye Xie, Yiqi Chen, Yucong Li, Yingqian Zhou, Wandi Li, Lipeng Zhang, Guoqing Yang, Qian Wei, Chuan’an Shen, Engineered sEVs encapsulated in GelMA facilitated diabetic wound healing by promoting angiogenesis via targeting thrombospondin-1, Burns & Trauma, 2025;, tkaf036, https://doi.org/10.1093/burnst/tkaf036
Powered by WPeMatico
