Fatty Liver Index Predicts Hepatocellular Carcinoma Risk in T2DM Without Cirrhosis: Study
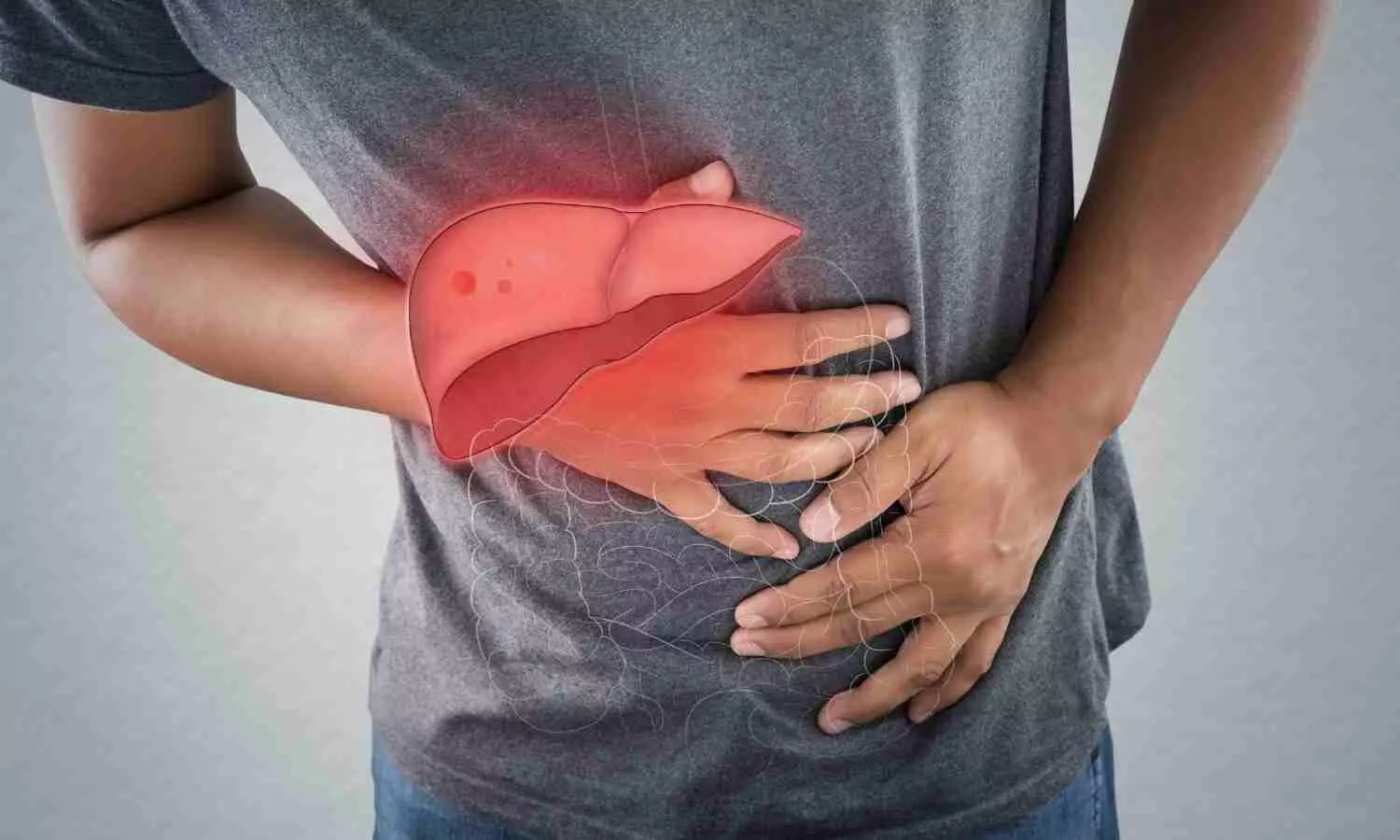
A new study has established that the follow-up of the fatty liver index (FLI), both baseline and longitudinally, is an effective predictor of the risk of hepatocellular carcinoma (HCC) in type 2 diabetes mellitus (T2DM) patients even without cirrhosis. The research points out that T2DM is a leading risk factor for HCC, especially among patients with nonalcoholic fatty liver disease (NAFLD), but existing surveillance guidelines tend to disregard non-cirrhotic patients. These results emphasize the value of adding FLI as an inexpensive yet useful instrument for early cancer risk detection and intervention. The study was published in the journal Endocrinology and Metabolism by Eun-Hee Cho and colleagues.
HCC is still among the top cancer killers globally, and T2DM plays a major role in its development, especially when it occurs with fatty liver. Although there is known association, patients with T2DM without cirrhosis are generally not considered for routine screening for liver cancer, leaving a gap for early detection. This new evidence puts the FLI, a scoring system from waist circumference, body mass index (BMI), triglyceride, and gamma-glutamyl transferase (GGT) levels as a promising solution.
In this population-based study, health screening data of 92,761 people with T2DM aged 40-79 years who had two standardized health examinations between 2012 and 2015 were investigated. FLI was computed for each participant according to validated clinical parameters. Participants were stratified by both baseline FLI and FLI change according to these scores.
To detect new cases of HCC, investigators employed International Classification of Diseases (ICD) codes and billing records gathered from 2016 through 2020. The research sought to assess how alterations in FLI values either a rise or decline between screenings influenced the eventual risk of liver cancer development.
Key Findings
The research presented robust evidence that high baseline FLI values and rising FLI over time are associated with greater risks of developing HCC among T2DM patients:
• Those with a baseline FLI of 30 to 59.9 had a 1.90-fold higher risk of developing HCC than those with FLI <30 (P < 0.01).
• Those with baseline FLI ≥60 had a yet greater risk—2.94-fold—of developing HCC (P < 0.01).
• Individuals whose FLI rose from <30 to ≥30 during the interval between the two screenings had a 2.10-fold greater risk of HCC (P < 0.01).
• On the other hand, patients whose FLI decreased from ≥30 to <30 had 36% reduced risk for developing HCC (HR = 0.64, P = 0.03).
• Significantly, the protective effect of reduced FLI became apparent only after approximately 3 years, indicating that long-term follow-up is essential.
Overall, the research shows that baseline FLI values, as well as their time-dependent variations, are strong risk predictors of hepatocellular carcinoma in type 2 diabetic patients even if without liver cirrhosis. The rising FLI intensifies HCC risk, whereas its decline is linked to a lower risk, although with several years’ delay. These observations imply that FLI monitoring at regular intervals may be particularly useful and effective as a screening tool for early detection of high-risk individuals, enabling timely intervention and a possible decrease in liver cancer mortality in T2DM patients.
Reference:
Cho EH, Kang MG, Lee CH, Oh S, Shen C, Oh HR, Park YR, Lee H, Kim JS, Park JH. Fatty Liver Index Dynamics as a Predictor of Hepatocellular Carcinoma in Patients with Type 2 Diabetes Mellitus and Non-Cirrhotic Livers. Endocrinol Metab (Seoul). 2025 May 29. doi: 10.3803/EnM.2024.2286. Epub ahead of print. PMID: 40437794.
Powered by WPeMatico