About one in five people taking Ozempic, Wegovy or Mounjaro say food tastes saltier or sweeter than before
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Pennington: ZyVet Animal Health, a generic pharmaceuticals company for animals, a wholly owned subsidiary of Zydus Pharmaceuticals (USA) Inc., itself a wholly owned subsidiary of Zydus Lifesciences Ltd., a global innovation led healthcare company, has released the FDA-approved generic of phenylpropanolamine hydrochloride tablets, a treatment for managing urinary incontinence in dogs, in the United States.
Powered by WPeMatico

Noida: The Haryana health department, in collaboration with authorities in Noida, busted a long-running sex determination racket operating out of a private radiology centre in Sector 37. The raid led to the arrest of five individuals, including the doctor, and the seizure of two ultrasound machines.
Acting on a tip-off received by health authorities in Panipat, the team coordinated with Dr. Chandan Soni, Deputy Chief Medical Officer of Gautam Buddh Nagar, and conducted a sting operation on Friday.
According to the news reports, authorities executed a sting operation by sending a pregnant woman to the scanning centre after negotiating a Rs 25,000 deal with a broker.
Also Read:Meerut doctor, 3 touts held for conducting illegal sex determination test
“Of the amount, Rs 20,000 was handed over to the staff on the day of the test, while Rs 5,000 was transferred online to the account of a woman named Maryam. Soon after the woman’s ultrasound, the staff distributed the cash among themselves and placed the remaining Rs 10,000 on the doctor’s table. The note was pre-identified with a serial number and matched with those found at the centre,” deputy CMO Soni said, reports TOI.
Following the raid, five individuals were arrested, including the clinic owner, a broker, a receptionist, a money handler, and a medical store operator. Two ultrasound machines were seized, and the team recovered marked currency note. According to officials, the centre had been operational for over a decade.
Speaking to TOI, the deputy CMO said, “An FIR has been filed under BNS 318(4) (cheating) and the Pre-Conception and Pre-Natal Diagnostic Techniques Act, 1994.”
The raid comes at a time when the government in neighbouring Haryana has launched a crackdown on sex determination clinics. At a recent meeting chaired by Additional Chief Secretary (Health) Sudhir Rajpal, strategies were laid out to track and dismantle these networks using phone records, financial trails, and location data of those arrested.
Also Read:Haryana Health Dept officials told to Inspect MTP, Ultrasound Centers
Powered by WPeMatico

New Delhi: Professor Pradeep Kumar Prajapati formally assumed charge as the Director of the All India Institute of Ayurveda (AIIA), New Delhi, recently.
Prior to this appointment, Prof. Prajapati served as the Vice-Chancellor of Dr Sarvepalli Radhakrishnan Rajasthan Ayurved University, Jodhpur. He has also been associated for a long period with Gujarat Ayurved University, Jamnagar, contributing significantly to research and academic development. He began his academic career as an Assistant Professor at the National Institute of Ayurveda (NIA), Jaipur.
A formal welcome ceremony was organized at AIIA to mark the occasion. The event began with the lighting of the ceremonial lamp and a Dhanvantari Vandana. The institute’s former Executive Director, Prof. (Dr.) Manjusha Rajagopal, Dean (PhD) Prof. (Dr.) Mahesh Vyas and a large number of academic, medical, administrative, and nursing staff were present. All attendees extended a warm welcome to the new Director by presenting floral bouquets.
Also Read:AYUSH Ministry Launches Initiatives to Integrate Ayush Medicine with Allopathic System
In his first address as Director, Prof. Prajapati said:
“It is a matter of great pride and honour for me to have the opportunity to serve Ayurveda at this esteemed institution. With the government’s vision of taking Ayurveda to the masses, I am confident that, with the collective support of all, AIIA will achieve global recognition in the years to come.”
Former Executive Director Prof. (Dr.) Manjusha Rajagopal, in her welcome remarks, expressed gratitude to all and reaffirmed her commitment to team spirit and collaborative work. Dean Prof. (Dr.) Mahesh Vyas highlighted that Prof. Prajapati’s experience with premier institutions in the country will help take AIIA to new heights.
Immediately after assuming charge, Prof. Prajapati participated in the valedictory session of a Continuing Medical Education (CME) program organized for faculty at the institute, where he also performed the ceremonial lamp lighting.
Prof. Prajapati holds a BAMS degree from Gurukul Kangri University and obtained his MD and PhD from Banaras Hindu University (BHU).
It is noteworthy that his appointment as Director of AIIA was approved by the Union Cabinet. As per the terms, he will serve for a period of five years from the date of assuming charge or until the age of superannuation, whichever is earlier.
Powered by WPeMatico
A higher weekly dose of semaglutide (7.2 mg) can significantly improve weight loss and related health outcomes in adults living with obesity, including those with type 2 diabetes (T2D), according to the results of two large-scale, international phase 3 clinical trials. The findings, published in The Lancet Diabetes & Endocrinology journal, suggest that a higher dose of semaglutide offers a promising new option for people with obesity, including those with T2D, who have not achieved sufficient weight loss with existing treatments.
The STEP UP and STEP UP T2D clinical trials are the first to investigate whether increasing the dose of semaglutide from the currently approved dose of 2·4 mg to 7·2 mg is safe and leads to additional weight reduction. Trial participants were randomised to receive either the higher 7·2 mg dose of semaglutide, the currently approved 2.4 mg dose, or placebo over 72 weeks. All participants-regardless of treatment group-received lifestyle interventions such as dietary counseling and increased physical activity recommendations.
In adults without diabetes, a 7·2 mg dose of semaglutide led to an average weight loss of nearly 19%, surpassing the 16% loss seen with 2·4 mg and 4% with placebo. Nearly half of the participants on the higher dose lost 20% or more of their body weight, with about one-third losing at least 25%. Participants also experienced improvements in waist circumference, blood pressure, blood sugar, and cholesterol levels, all key factors in reducing obesity-related health risks. Similarly, in adults with obesity and T2D, the 7·2 mg dose resulted in an average 13% weight loss compared to 10% with 2.4 mg and 3.9% with placebo, along with significant reductions in blood sugar levels and waist size.
Both trials reported that the higher dose of semaglutide was safe and generally well tolerated. Gastrointestinal side effects like nausea and diarrhoea, and some sensory symptoms like tingling, were the most common. However, most side effects were manageable, resolved over time, and did not lead to participants dropping out of the trial. No increase in serious adverse events or severe hypoglycaemia was observed with the higher dose.
By delivering greater weight reduction and metabolic benefits while maintaining a favourable safety profile, the authors say this higher dose could help more people reach their health goals and reduce the burden of obesity-related complications worldwide. However, they highlight that further research is needed to fully understand the long-term benefits and risks.
Reference:
Wharton, Sean et al., Once-weekly semaglutide 7·2 mg in adults with obesity (STEP UP): a randomised, controlled, phase 3b trial, The Lancet Diabetes & Endocrinology, DOI: 10.1016/S2213-8587(25)00226-8
Powered by WPeMatico
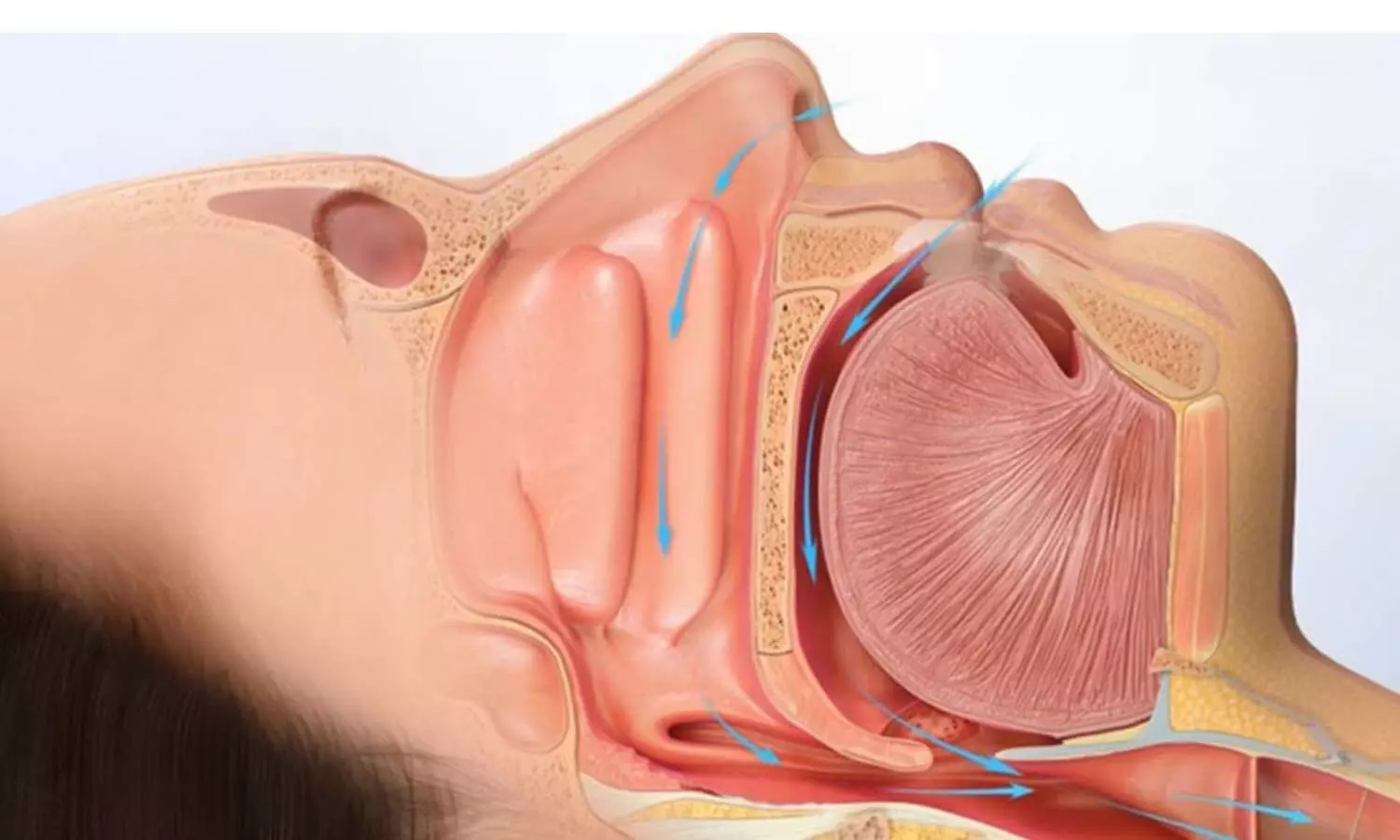
UK: Researchers have found in a new study that sleep-disordered breathing (SDB) is highly prevalent in hypertrophic cardiomyopathy (HCM) patients and is linked to adverse myocardial remodeling, greater diastolic dysfunction, and elevated troponin-T levels, indicating subclinical myocardial injury. The findings support further trials on treating SDB to improve outcomes in HCM.
Powered by WPeMatico

China: A new study has found that metabolic syndrome (MS) independently contributes to more severe and unfavorable coronary artery plaque characteristics in patients with type 2 diabetes mellitus (T2DM). These include higher rates of mixed, noncalcified, and nonobstructive plaques, as well as spotty calcification and extensive plaque burden.
Powered by WPeMatico

China: A new cardiac MRI-based workflow has shown promise in improving the prediction of sudden cardiac death (SCD) among individuals with nonischemic dilated cardiomyopathy (DCM), offering clinicians refined tools for risk stratification and personalized treatment strategies. By establishing specific cutoff values for late gadolinium enhancement (LGE) and extracellular volume fraction (ECV), the study demonstrates a more precise approach to identifying both high-risk and low-risk patient groups.
Powered by WPeMatico
