Hemoglobin’s antioxidant role in brain cells points to new therapeutic avenue
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
New Delhi- The National Board of Examinations in Medical Sciences (NBEMS) is soon going to publish the answer key of the National Eligibility and Entrance Test-Postgraduate (NEET PG) exam for the academic year 2025.
NBE declared the NEET-PG 2025 exam result recently on 19th August 2025.
According to the notice issued by the NBEMS in this regard, the NEET-PG 2025 exam answer key will be published as the Hon’ble Supreme Court has directed to publish the raw scores, answer keys and normalisation formulae for transparency in multi-shift NEET-PG exams.
Therefore, as per the Supreme Court direction, NBEMS will publish the answer key of NEET-PG 2025 on its official website. Along with the correct answer key, the responses marked by the candidates to the respective questions asked in NEET-PG 2025 will also be published. The score given for each of the questions as per the scheme of evaluation detailed in the Information Bulletin of NEET-PG 2025 will be mentioned too.
After the publication of the NEET-PG 2025 exam answer key, the candidates who have appeared in the NEET-PG 2025 shall be able to access the Answer Key and his/her marked responses through their applicant login at the NEET-PG 2025 index page at the NBEMS website.
Meanwhile, the notice also added that since the sequence of questions asked within a section are shuffled for different candidates and the order of four distractors of a question are also shuffled for different candidates appearing in NEET-PG 2025, the question ID Numbers, correct answer key and responses marked shall be displayed as per Master set of Question Paper used for NEET-PG 2025.
Moreover, NBEMS is in the process of developing an online portal to display the answer keys and responses marked. The same shall be made live at the earliest possible time.
To view the notice, click the link below
Powered by WPeMatico

Lucknow: Fortis Healthcare has signed a collaboration agreement with Ekana Group, Lucknow, for operations and management of a 550-bedded greenfield super speciality hospital to be constructed near Gomti Nagar, Lucknow by the Ekana Group.
Once completed, the facility will be positioned as Centre of Excellence for tertiary care services, bringing advanced medical infrastructure and global best practices to the state capital of Uttar Pradesh.
Speaking on the collaboration, Dr Ashutosh Raghuvanshi, MD & CEO, Fortis Healthcare, said, “We are delighted to partner with Ekana Group to bring a state-of-the-art tertiary healthcare facility to the heart of Lucknow.
Also Read:Fortis acquires Shrimann Superspecialty Hospital in Jalandhar for Rs 462 crore
Once operational, this new 550‑bed super‑specialty hospital near Gomti Nagar will significantly enhance access to advanced medical care for the city and its surrounding regions.
This collaboration marks Fortis Healthcare’s third major presence in Uttar Pradesh, joining our network hospitals in Noida and Greater Noida and underscores our steadfast commitment to expanding high‑quality healthcare across the state.”
Mr. Uday Sinha, Promoter of Ekana Group, said, “We are happy to join hands with one of the leading healthcare chains in India – Fortis Healthcare to develop a leading-edge tertiary care hospital, one that will significantly enhance access to advanced medical services and deliver patient care where it’s most needed.”
Medical Dialogues had earlier reported that in yet another clinical milestone, Fortis Hospital, Bannerghatta Road, Bengaluru, has advanced its robot-aided infrastructure with the launch of the TREAT program (Total Robot Enabled and Assisted Transplant) – a pioneering initiative in robot-assisted kidney transplantation. This state-of-the-art initiative marks a major leap forward in surgical excellence and patient care, especially with its historic milestone: the successful execution of simultaneous robotic surgeries for both donor and recipient — a first-of-its-kind clinical achievement in India.
Powered by WPeMatico

Researchers have found in a new study that an AI-based personalized lifestyle management system could help patients with type 2 diabetes lower HbA1c levels and reduce dependence on glucose-lowering medications, offering a scalable and affordable approach to diabetes care. The study was published in the NEJM Catalyst Innovations in Care Delivery by Kevin M. and colleagues.
Even with significant progress in pharmacological treatments and digital health technologies, optimal glycemic control in T2D is still a worldwide challenge to reach and maintain. Lifestyle interventions are successful but hard to sustain in everyday clinical practice. Artificial intelligence (AI) and machine learning (ML) now offer the possibility of providing highly personalized and pragmatic advice that fills the gap between doctor’s recommendations and patient behavior.
The Twin Precision Treatment system combines wearables with Bluetooth-enabled devices (such as continuous glucose monitors), focused laboratory data, Internet of Things, AI-ML algorithms, and human guidance to deliver real-time, patient-specific advice.
This single-center randomized controlled trial recruited 150 adults with T2D with a body mass index (BMI) of ≥27. Participants were randomly assigned in a 2:1 ratio to the intervention group (INT, N=100) or the usual care group (UC, N=50). The main endpoint was to reach HbA1c <6.5% (<48 mmol/mol) off glucose-lowering therapy (other than metformin) at 12 months.
Secondary endpoints were:
• Maintenance of HbA1c <6.5% off medications for ≥90 days before 12 months
• Reaching HbA1c <6.5% off any glucose-lowering medications at 12 months and maintained ≥90 days
• HbA1c and weight change at 12 months
• Post hoc analyses of medication usage and quality-of-life scores.
Key Findings
Primary endpoint:
• Attained by 71.0% of INT participants (95% CI, 60.1–80.0)
• Attained by just 2.4% of UC participants (95% CI, 0.5–11.6)
• P<0.001
Glycemic target sustained ≥90 days before 12 months (except metformin):
• 52.5% in INT vs. 2.8% in UC (P<0.001)
Reduction in HbA1c at 12 months:
• INT: −1.3%
• UC: −0.3%
• P<0.001
Weight loss at 12 months:
• INT: −8.6%
• UC: −4.6%
• P<0.001
Medication use:
• Significant reduction in glucose-lowering pharmacotherapy in INT group
• No change of significance in UC group
• Quality of life and treatment satisfaction
• Mean improvement in INT group (exploratory analysis)
• No improvement in UC group
In this randomized trial of 150 adults with T2D, an AI-supported bundled system of sensors and coaching resulted in much more improved glycemic control, weight loss, and quality of life compared to standard care. Most importantly, it enabled huge de-escalation of glucose-lowering drugs, with 71% attaining HbA1c <6.5% off all medications except metformin versus 2.4% in controls. These findings demonstrate the revolutionary potential of precision medicine based on AI in type 2 diabetes treatment.
Reference:
Powered by WPeMatico

Germany: A secondary analysis of the EAST-AFNET 4 randomized clinical trial, published in JAMA Cardiology, has highlighted that early rhythm control therapy remains effective and safe in patients with atrial fibrillation (AF) irrespective of the presence of obesity or diabetes. The study was conducted by Andreas Metzner and colleagues from the German Center for Cardiovascular Research, Partner Site Hamburg/Lübeck/Kiel, Hamburg, Germany.
The EAST-AFNET 4 trial, conducted across 11 European countries, evaluated whether initiating rhythm control therapy early in the course of AF could reduce major cardiovascular complications. Participants included individuals diagnosed with AF within the previous year who also had underlying cardiovascular conditions. In this prespecified secondary analysis, the investigators assessed whether body mass index (BMI) and diabetes status influenced the outcomes of early rhythm control compared to usual care.
The trial enrolled 1,086 participants with obesity (BMI ≥30) and 1,690 without obesity (BMI <30). The average age across all participants was 70 years, with nearly 47% being women.
The following were the key findings of the study:
According to the authors, these findings provide reassurance that early rhythm control strategies can be safely and effectively applied across a broad patient population, including those with metabolic risk factors such as high BMI and diabetes. This is particularly significant given the rising prevalence of both conditions worldwide and their known association with AF and adverse cardiovascular outcomes.
“The results emphasize the potential of early rhythm control as a standard approach for managing newly diagnosed AF, supporting its use even in patients with complex metabolic profiles. By demonstrating consistent benefits across different subgroups, the study strengthens the evidence base for adopting early rhythm control strategies in routine clinical practice for patients with AF and coexisting cardiovascular disease,’ the authors concluded.
Reference:
Metzner A, Willems S, Borof K, et al. Diabetes and Obesity and Treatment Effect of Early Rhythm Control vs Usual Care in Patients With Atrial Fibrillation: A Secondary Analysis of the EAST-AFNET 4 Randomized Clinical Trial. JAMA Cardiol. Published online July 30, 2025. doi:10.1001/jamacardio.2025.2374
Powered by WPeMatico
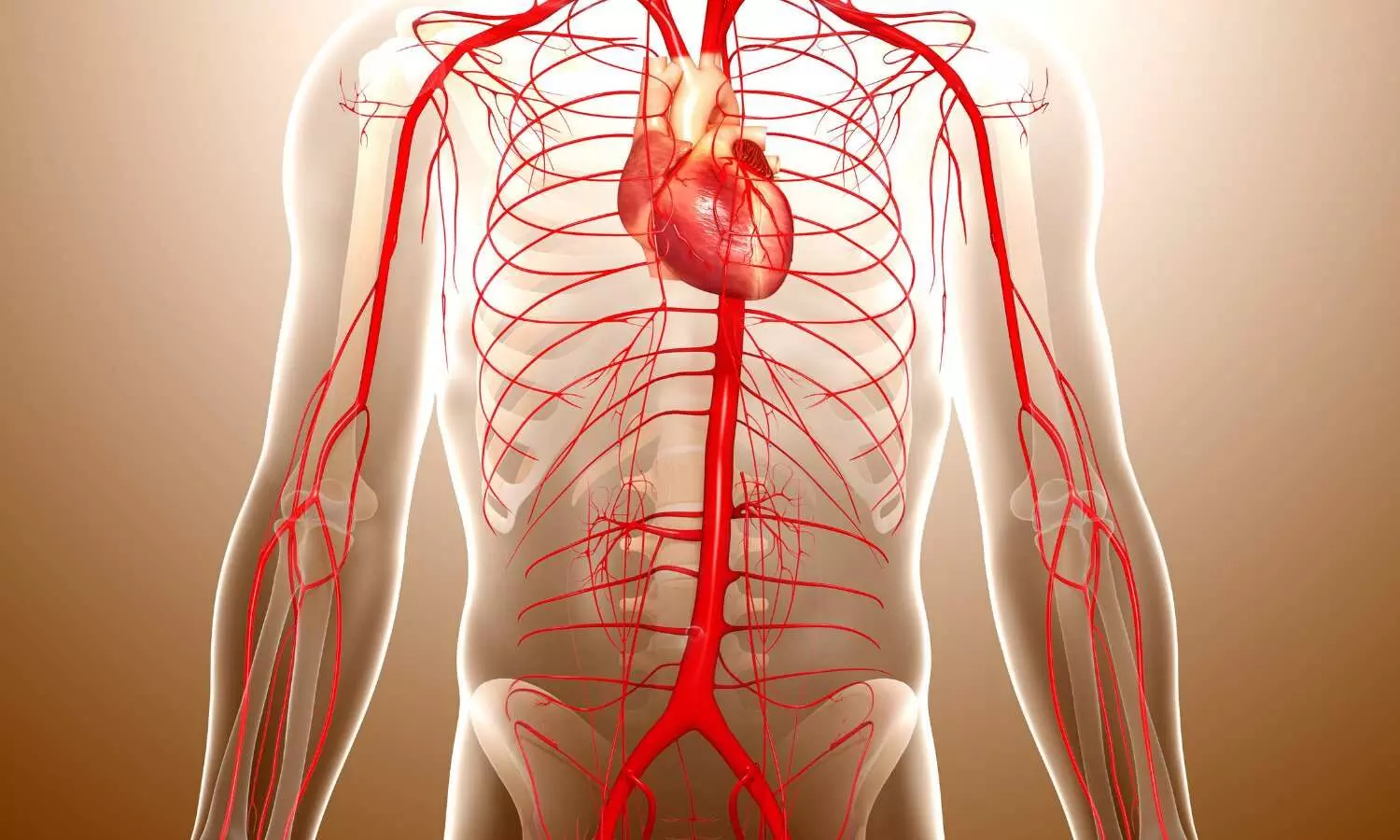
USA: Preclinical research published in Circulation suggests that hypertriglyceridemia plays a significant role in the development and rupture of abdominal aortic aneurysms (AAA).
AAA, a potentially fatal condition characterized by the dilation and rupture of the abdominal aorta, currently lacks effective pharmacological treatment. The study, led by Dr. Yaozhong Liu and colleagues from the University of Michigan Medical Center, aimed to explore the controversial and previously unclear link between triglyceride levels and AAA pathogenesis.
Using Mendelian randomization, the researchers analyzed genetic, proteomic, and metabolomic data to assess the causal role of lipid-related pathways in AAA risk. Their findings revealed a strong association between elevated triglyceride-rich lipoproteins and increased susceptibility to AAA. Experimental models involving mice with different degrees of hypertriglyceridemia—such as Lpl-deficient, Apoa5-deficient, and human APOC3 transgenic mice—provided further evidence supporting this link.
The following were the key findings of the study:
To evaluate potential therapeutic strategies, the team administered an antisense oligonucleotide (ASO) targeting angiopoietin-like protein 3 (ANGPTL3), a liver-derived regulator of triglyceride metabolism. This intervention effectively reduced triglyceride levels and significantly slowed AAA progression in both human APOC3 transgenic and Apoe-deficient mice.
The study emphasizes that managing triglyceride-rich lipoproteins may represent a viable therapeutic avenue for AAA. It also highlights the promise of ASO therapy against ANGPTL3 as a targeted approach to mitigate AAA risk, particularly in individuals with a genetic predisposition.
Despite its robust findings, the study acknowledged some limitations. The extreme hypertriglyceridemia observed in certain animal models may not fully reflect human conditions, and concurrent changes in cholesterol levels could confound interpretations. Furthermore, while palmitate’s role in LOX inhibition is clear, the direct evidence of its accumulation in the aorta is still lacking.
“The comprehensive analysis strengthens the understanding of hypertriglyceridemia as a critical factor in AAA development and rupture. The findings emphasize the need for further experimental and clinical research to develop triglyceride-lowering strategies as potential interventions for this life-threatening vascular disease,” the authors concluded.
Reference:
https://doi.org/10.1161/CIRCULATIONAHA.125.074737
Powered by WPeMatico

A new study from Emory University reveals that maintaining optimal cardiovascular health can significantly improve overall physical and psychological well-being.
Published today in the Journal of the American Heart Association, the study synthesizes findings from nearly 500 peer-reviewed studies. It confirms that the benefits of heart-healthy behaviors extend far beyond the heart, positively impacting brain function, vision, hearing, muscle strength, and even reducing the risk of chronic diseases such as cancer and dementia.
“While we recently learned that heart-health and brain health are closely tied, in this review we found that almost every organ system and bodily function from head to toe benefit from a heart-healthy lifestyle,” says Liliana Aguayo, PhD, MPH, research assistant professor at the Emory University Nell Hodgson Woodruff School of Nursing and core faculty member at Emory’s Global Diabetes Research Center, who led the study.
The review is the first of its kind to systematically examine how the American Heart Association’s Life’s Simple 7™ metrics-which include not smoking, healthy eating, regular physical activity, maintaining a healthy weight, and managing blood pressure, cholesterol, and blood sugar-influence health outcomes across multiple organ systems. The updated Life’s Essential 8™ also includes sleep as a key factor.
Among the key findings were that those with heart-healthy habits:
The study was supported in part by the American Heart Association and the National Institutes of Health. It calls for further research in underrepresented populations, including children and pregnant women, and emphasizes the need to understand how even minor lifestyle improvements yield significant health benefits.
Reference:
Liliana Aguayo, Cardiovascular Health, 2010 to 2020: A Systematic Review of a Decade of Research on Life’s Simple 7, Journal of the American Heart Association, https://doi.org/10.1161/JAHA.124.038566
Powered by WPeMatico

A new study published in the Annals of Medicine and Surgery showed that metformin use in patients with both asthma and metabolic syndrome significantly improved ACT scores, FEV₁, and FVC.
A major global health concern that affects people of all ages is asthma. Nearly 235 million people are thought to have asthma globally, with high-income nations having the highest frequency and rising incidence. More severe and frequent asthma episodes as well as worse asthma management may be linked to MetS.
As a possible therapy for MetS, metformin has been proposed; this medication may lower airway responsiveness, improve asthma management, and minimize ED visits. However, the majority of the data that is currently available focuses only on people with diabetes. Thus, this study was carried out by Hossein Mehravaran and colleagues to examine the effects of metformin in individuals who both had asthma and MetS.
Metformin hydrochloride or an identical placebo was administered to 2 groups of individuals (55 in each group) who had both asthma and MetS at the same time. After 3 months, the patients were evaluated for clinical outcomes, pulmonary function test parameters, C-reactive protein (CRP) levels, asthma control tests (ACTs), frequency of asthma episodes, emergency department visits, and hospitalization rate.
ACT score, O2 saturation, anthropometric indices, blood sugar management, CRP, and lipid profile all improved statistically significantly in the metformin group as compared to the placebo group (all P < 0.05).
Furthermore, after adjusting for the confounding effects of baseline parameters and sex, the multivariate analysis revealed that the metformin group had significantly higher forced expiratory volume in 1 second (FEV1) (P = 0.014, and effect size = 5.6%) and forced vital capacity (FVC) (P = 0.001, and effect size = 9.2%).
The metformin group showed a tendency to have lower rates of hospitalization, ED visits, and severe asthma episodes, but the effects were not statistically significant (P > 0.05).
Overall, the findings demonstrated that giving metformin to individuals who have both asthma and MetS simultaneously improves the patients’ lipid profile indices, body composition parameters, short- and long-term blood sugar management, and vital signs. Additionally, it leads to increases in ACT score, FEV1, and FVC, all of which contribute to improved pulmonary function, and it significantly lowers CRP levels, an inflammatory marker.
Source:
Mehravaran, H., Bahar, A., Hajimohammadi, F., Kashi, Z., Aliyali, M., Varshoei, F., Alizadeh-Navaei, R., Yazdani Charati, J., Kashefizadeh, A., Gheibi, M., & Ghadirzadeh, E. (2025). Metformin effects on respiratory and metabolic outcomes in asthma and metabolic syndrome: a double-blind, randomized, placebo-controlled clinical trial. Annals of Medicine and Surgery (2012), 87(8), 4861–4869. https://doi.org/10.1097/MS9.0000000000003552
Powered by WPeMatico
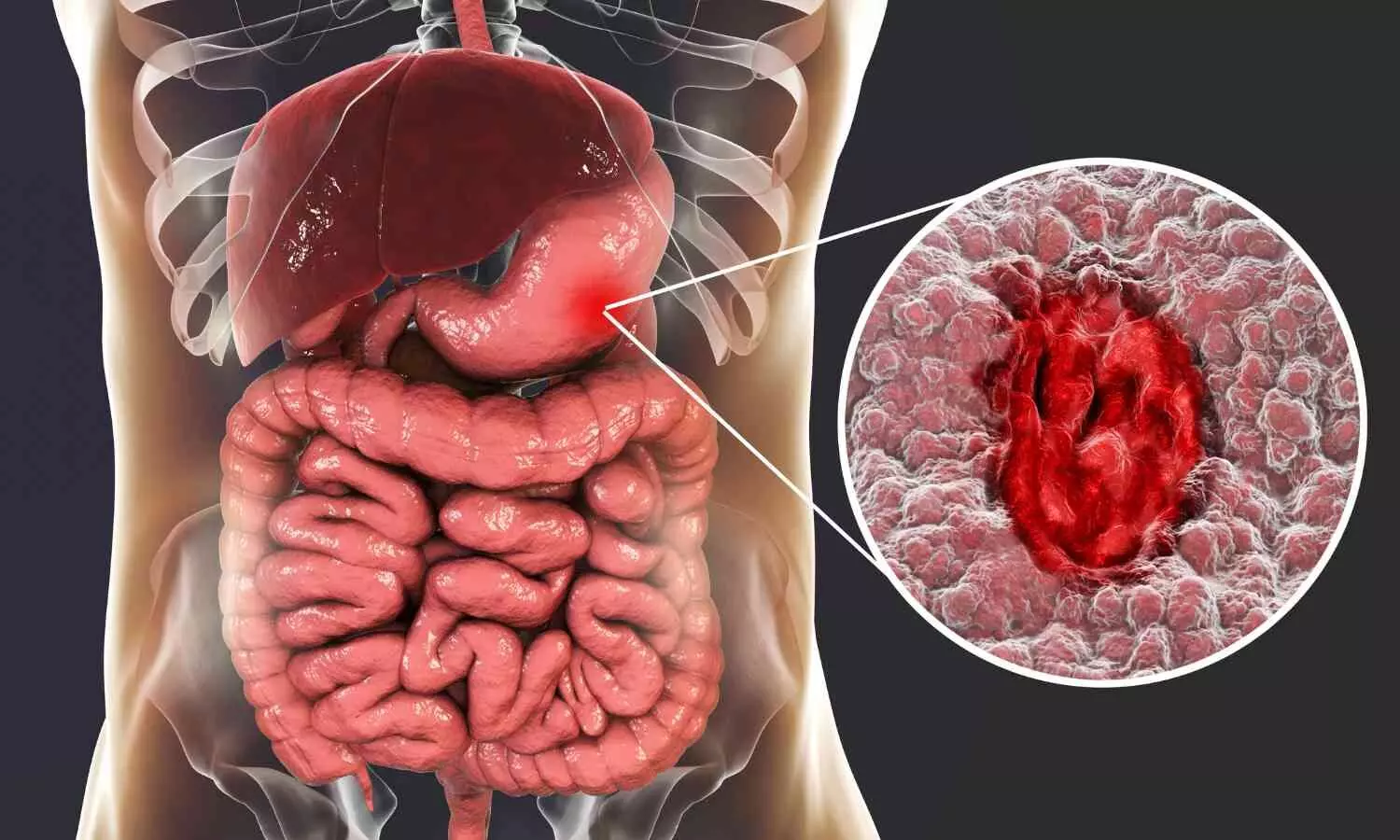
USA: A recent multicenter study published in JAMA Surgery has demonstrated the potential of an exosome-based liquid biopsy assay, Destinex, for the early and noninvasive detection of gastric cancer (GC). The study, led by Silei Sui from the Department of Molecular Diagnostics and Experimental Therapeutics, Beckman Research Institute of City of Hope, California, evaluated the clinical utility of microRNA (miRNA) signatures as biomarkers for screening and diagnosis.
Gastric cancer remains the third leading cause of cancer-related deaths globally, with late diagnosis being a key factor driving poor outcomes. Current reliance on endoscopy for screening is limited by its invasive nature and high cost, highlighting the urgent need for reliable blood-based tests. To address this gap, the DESTINEX study developed and validated a diagnostic assay using exosome-derived miRNAs to detect GC at an early stage.
The case-control study analyzed 809 specimens from 480 participants across major referral centers, including Nagoya University Hospital in Japan and three leading South Korean institutions: Ajou University Hospital, Asan Medical Center, and Samsung Medical Center. The research followed a comprehensive biomarker development pipeline, involving discovery, training, validation, and evaluation phases. Data collection spanned from 2016 to 2020, with analysis completed between 2022 and 2024.
The study revealed the following findings:
“These findings suggest that the Destinex assay could significantly strengthen existing gastric cancer screening strategies and improve early diagnosis rates,” the authors noted. With its high sensitivity and specificity, Destinex could be an important noninvasive complement to current screening protocols, potentially reducing dependence on invasive endoscopy for initial detection.
Despite the promising results, the study acknowledged certain limitations. The patient cohorts had uneven age and sex distribution, and patients with chronic atrophic gastritis and intestinal metaplasia were not included. Moreover, the validation was limited to Asian populations, highlighting the need for further multinational studies to confirm its diagnostic efficacy across diverse demographics. The authors also emphasized the necessity of expanding research to evaluate its performance in other gastrointestinal cancers.
The DESTINEX study’s findings highlight a major advancement in liquid biopsy technology for gastrointestinal oncology. By leveraging exosomal miRNAs and machine learning algorithms, the Destinex assay offers a robust, noninvasive option for early detection of gastric cancer, with the potential to transform clinical practice and significantly improve patient outcomes worldwide.
Reference:
Sui S, Xu C, Kanda M, et al. Exosomal Liquid Biopsy for the Early Detection of Gastric Cancer: The DESTINEX Multicenter Study. JAMA Surg. Published online July 30, 2025. doi:10.1001/jamasurg.2025.2493
Powered by WPeMatico
