Minimally Invasive tissue-selecting therapy Effective and Safe for Severe Hemorrhoids, reveals research
Researchers have found in a new study that minimally invasive tissue-selecting therapy (TST) is effective in managing severe hemorrhoids, significantly enhances anorectal motility, and demonstrates a low rate of postoperative complications, indicating a high level of safety.
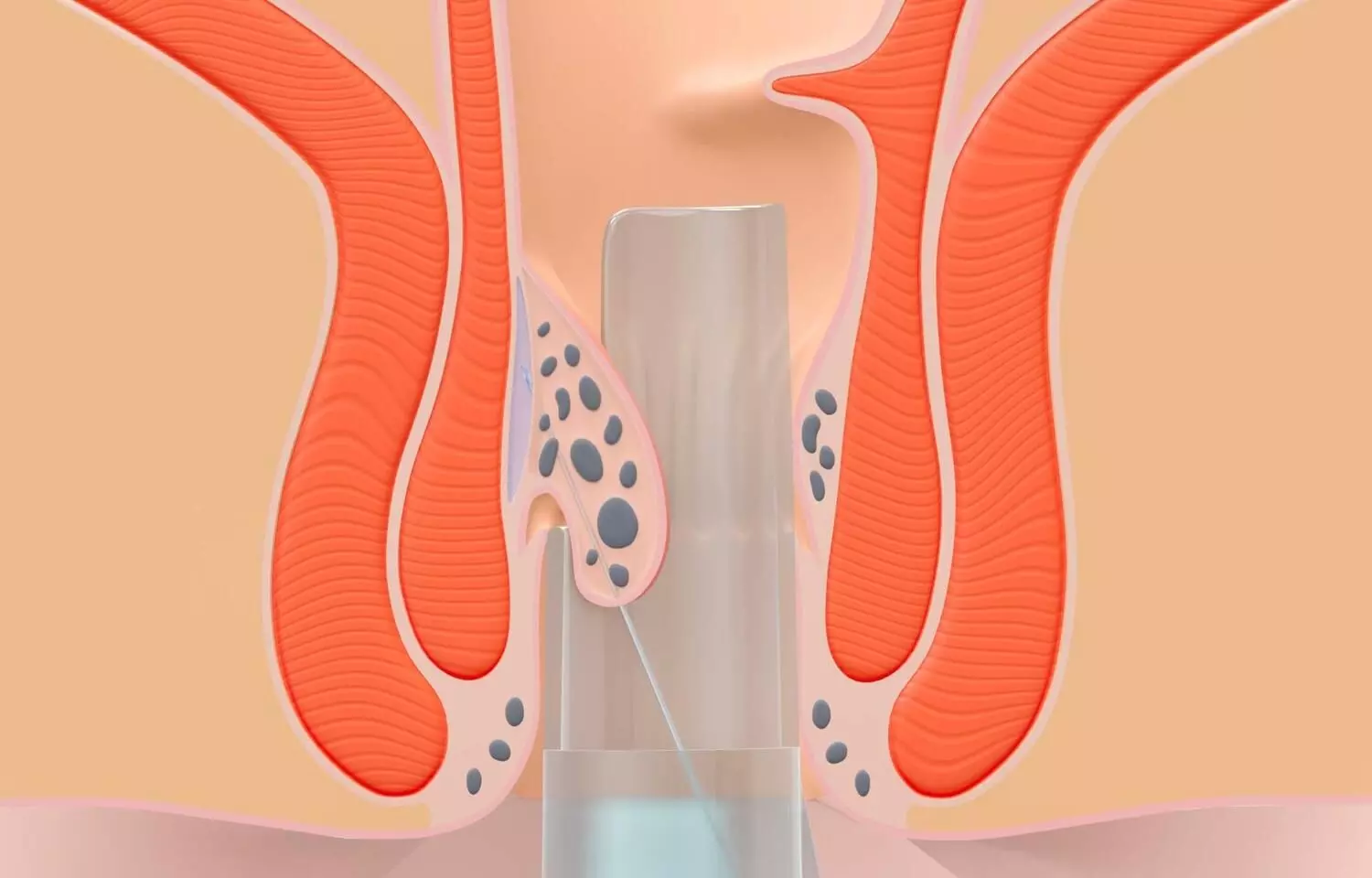
Severe hemorrhoids have a serious impact on patients’ quality of life. At present, the main method for treating severe hemorrhoids is surgery, but surgical treatment causes greater trauma to patients and has a high degree of complications. There is an urgent need to find new surgical methods to solve these problems. To assess the ability of tissue-selective therapy stapler (TST) minimally invasive surgery to treat severe hemorrhoids by studying the clinical efficacy, postoperative complications, and anal dynamics of selective supramedullary hemorrhoid stomy. In the hospital, between March 2015 and February 2018, 141 patients with severe hemorrhoids were included into three groups according to the block randomization method: the TST group, the pieces per hour the PPH group, and the eastern rubber band ligation and coincident of dislocation for prolapse and hemorrhoid (EPH)group. There were 47 patients in each group. The clinical efficacy of the three groups of patients, changes in hospital stay time, operation time, intraoperative blood loss, postoperative complications, and anal dynamic indicators (rectal resting pressure, anal resting pressure, anorectal pressure difference, rectal tolerance, rectal perception threshold and length of the anal high-pressure zone) were observed and compared. Results: The total effective rate in the TST group was 93.62%, which was higher than the 74.47% and 72.34% in the PPH and EPH groups, respectively, after treatment. Hospitalization time, operation time, and intraoperative blood loss were lower in the TST group than in the EPH and PPH groups. Three months after surgery, the rectal resting pressure, rectal tolerance, and rectal sensing thresholds of patients in the TST group were lower than those in the PPH and EPH groups, and the anal canal resting pressure, the anorectal pressure difference and the length of the anal high-pressure zone were greater than those in the PPH and EPH groups. After surgery, the complication rate in the TST group was 10.64%, which was lower than the 27.66% and 31.91% reported in the PPH and EPH groups, respectively. Minimally invasive TST is effective in treating severe hemorrhoids, can significantly improve anorectal motility, has a low incidence of postoperative complications and is highly safe.
Reference:
Huang, R., Fan, M., Lin, H. et al. Tissue selecting therapy stapler minimally invasive surgery to treat severe hemorrhoids. BMC Surg 25, 293 (2025). https://doi.org/10.1186/s12893-025-02918-5
Keywords:
1500X 600 Minimally, Invasive, tissue-selecting, therapy, Effective, Safe, Severe, Hemorrhoids, reveals, research, Huang, R., Fan, M., Lin, H, Selective suprahemorrhoidal, mucosa anastomosis, Severe hemorrhoids, Clinical efficacy, Complications, Anal dynamics
Powered by WPeMatico