Elevated TyG-BMI may Predict Mortality in Critically Ill Ischemic Stroke Patients: Study
A new study published in the journal of BMC Cardiovascular Diabetology showed that in patients with critically sick ischemic stroke (IS), increased triglyceride glucose-body mass index (TyG-BMI) is substantially linked to an increased risk of short-term all-cause mortality.
Focal neurological dysfunction and cerebral tissue necrosis are hallmarks of ischemic stroke, which is usually caused by insitu thrombotic events or the embolization of atherothrombos from proximal artery sources. Moreover, the most frequent causes of ischemic stroke attributable to other causes include hematological illnesses, such as essential thrombocythemia, polycythemia vera, and thrombotic thrombocytopenic purpura, which can also present as acute ischemic stroke.
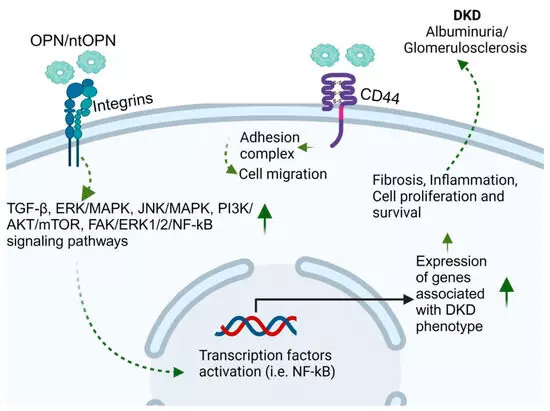
Calculated by multiplying fasting triglyceride and fasting glucose levels, the triglyceride-glucose index is a simple and accurate surrogate diagnostic for evaluating insulin resistance (IR), which is associated with IS. In order to fill up current research gaps and provide more accurate biomarker references for therapeutic applications, this study, which is based on the eICU database, examines the connection between the TyG-BMI and 28-day mortality in critically ill IS patients.
The effects of the TyG-BMI on 28-day hospital and intensive care unit mortality were examined using multivariate Cox regression models. To investigate the nonlinear association between the TyG-BMI and 28-day mortality, restricted cubic splines (RCS) were used. K-M curves were used to compare the results of the various TyG-BMI groups. Furthermore, subgroup and interaction analyses were conducted to confirm the results’ resilience.
The mean age of the 1,362 severely sick IS patients that were included was 68.41 ± 14.16 years, and 47.50% of them were male. The high TyG-BMI group had substantially greater ICU and 28-day hospital mortality, according to multivariate Cox regression analysis. The TyG-BMI and 28-day inpatient mortality had a nonlinear positive connection, according to RCS analysis.
There was a 37.3% rise in 28-day hospital mortality for every 1 standard deviation (SD) increase in TyG-BMI below the inflection point of TyG-BMI = 380.37, and an 87.9% decrease in 28-day hospital mortality for every 1 SD increase in TyG-BMI beyond 380.376. The P value for the log-likelihood ratio test is 0.004. The TyG-BMI showed a strong positive linear connection in RCS for 28-day ICU mortality. Overall, among critically sick IS patients in the US, an elevated TyG-BMI is substantially associated with a higher risk of short-term all-cause mortality.
Reference:
Ouyang, Q., Xu, L., & Yu, M. (2025). Associations of triglyceride glucose-body mass index with short-term mortality in critically ill patients with ischemic stroke. Cardiovascular Diabetology, 24(1). https://doi.org/10.1186/s12933-025-02583-1
Powered by WPeMatico