Liver transplantation utilizing grafts donated after euthanasia is feasible, study suggests
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
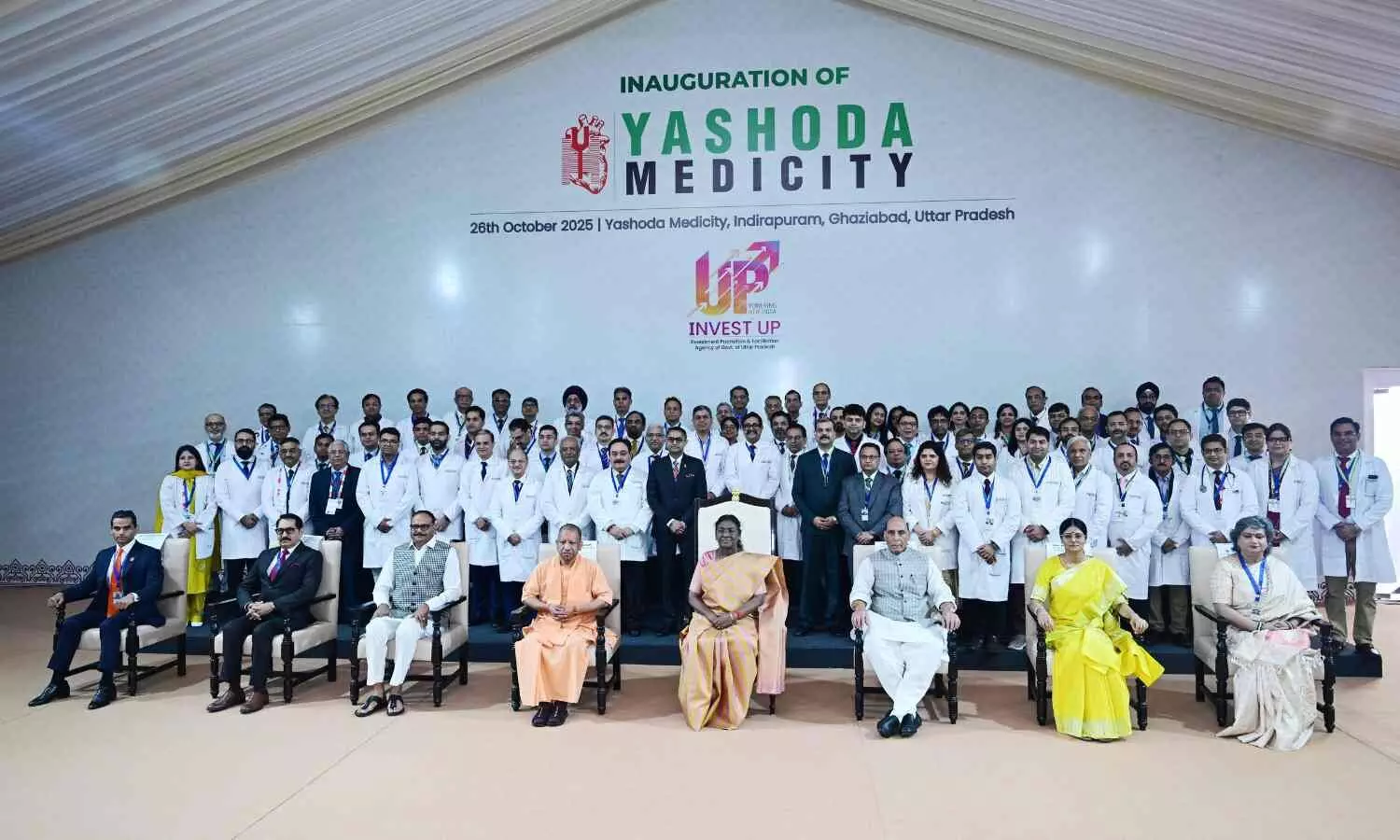
Ghaziabad: The President of India, Smt. Droupadi Murmu inaugurated Yashoda Medicity at Indirapuram, Ghaziabad, Uttar Pradesh, on October 26, 2025.
Speaking on the occasion, the President said that healthcare is an integral part of nation-building. Protecting people from disease and improving their health is a priority for the government. For this purpose, health and medical infrastructure, institutions, and services are being continuously expanded across the country. She stated that all such efforts will certainly contribute to building a healthy and developed India. Apart from the government, all other stakeholders will also play a crucial role in these efforts. Therefore, it is the responsibility of all stakeholders to expand healthcare services and ensure that quality services are available in all areas of the country and that no citizen is deprived of effective healthcare. Good private sector healthcare institutions can make an invaluable contribution to achieving this goal. She expressed confidence that Yashoda Medicity will bring about transformative work in the healthcare sector.
Also Read:Yashoda Medicity opens Robotic Surgery Training Centre in Ghaziabad

The President was happy to note that during the global pandemic of COVID-19, the Yashoda Hospital treated a large number of people, and that it has diligently embraced national priorities such as the National TB Elimination Program. She urged the institution to contribute its utmost to national campaigns related to sickle cell anemia. She also advised the stakeholders of the hospital to undertake research and collaborate with other institutions for the treatment of cancer, the PIB stated.
The President said that fulfilling social responsibility, along with medical responsibility, should be a priority for healthcare institutions. She was confident that Yashoda Medicity would realize its mission of ‘Affordable World Class Healthcare Services to All.’ She stated that with the support of excellent healthcare institutions in both the private and government sectors, India will gain more recognition as a global healthcare destination.
Also Read:Dr JB Sharma takes over as Head of Obstetrics and Gynaecology at Yashoda Medicity
Powered by WPeMatico

Chandigarh: Amid overcrowding and rising health concerns in Punjab’s prisons, the state government is now planning to establish Aam Aadmi Clinics (AACs) in all ten central jails to provide inmates with better medical care.
The state health department has reportedly begun identifying suitable spaces within the jails to implement the initiative.
Also Read:SC approves 300-bed Hospital on Sanganer Jail land
Punjab already has 24/7 medical officers deployed in all jails; however, the AAC model is expected to significantly expand access to medical care. The government recently floated tenders to establish 236 new AACs, which will bring the total number of functional clinics in the state to around 1,117.
A senior health department official mentioned that AACs offer 107 types of free medicines and 47 types of free diagnostic tests, which will significantly improve medical treatment for jail inmates.
According to the news reports, Punjab’s prison system has long faced challenges due to overcrowding, with inmates suffering from serious illnesses, including HIV, hepatitis C, and tuberculosis. In August, the principal secretary (jails) had written to the principal secretary (health) highlighting the strain on prison healthcare services. The letter noted inadequate medical infrastructure, vacant healthcare posts, and limited preventive care facilities.
Also Read:Delhi Government tightens leave policy for Mohalla Clinic doctors
Powered by WPeMatico

USA: A new study published in Diabetes Care revealed that automated insulin delivery (AID) systems lowered A1C levels and increased time in the glucose range for adults with type 2 diabetes, regardless of their C-peptide levels. Researchers concluded that having a low C-peptide level should not be a prerequisite for AID therapy.
Powered by WPeMatico

USA: A new retrospective cohort study published in the Annals of the American Thoracic Society suggests that acetaminophen may play a significant role in preventing delirium among critically ill patients in the Intensive Care Unit (ICU).
Powered by WPeMatico

UK: A study examining World War II-era sugar rationing in the United Kingdom found that individuals exposed to limited sugar intake from conception through early childhood had significantly lower cardiovascular risks later in life. Those who spent their first 1,000 days under sugar rationing showed a 20% lower risk of cardiovascular disease and a 25% lower risk of heart attack after age 40.
Powered by WPeMatico
