Traumatic brain injuries in older adults linked to increased risk of dementia
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Taiwan: A recent study has found that the use of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) in patients with type 2 diabetes delivers body mass index (BMI)-dependent cardiovascular benefits and consistent kidney protection.
Powered by WPeMatico

Influenza is much more than just a nasty cold – it is one of the most dangerous infectious diseases worldwide, claiming around half a million lives every year.
What makes it particularly insidious is that flu viruses are contagious even before the first symptoms appear. Despite this threat, the diagnostic options available to date are far from ideal. They are often expensive, complicated to use and simply unavailable in many poorer regions of the world.
A research team led by Professor Lorenz Meinel from the University of Würzburg has developed the technology behind a new self-test for influenza, recently published in ACS Central Science.
The new principle could make flu diagnosis quicker, cheaper and easier in the future. Anyone could use it anytime, anywhere, for example in the form of chewing gum or a lollipop that reacts to flu viruses in the saliva of infected people and releases a flavouring. In the mouths of non-infected individuals, however, nothing would happen. This would allow those affected to detect an infection within minutes – without the need for a laboratory, electricity or medical personnel.
‘This strategy opens up new possibilities for the early detection and control of influenza worldwide,’ says Lorenz Meinel, who heads the Chair of Drug Formulation and Delivery at the University of Würzburg.
The new diagnostic tool consists of the sensor molecule thymol – a natural substance found in thyme, among other things – and a virus-specific sugar building block. When it comes into contact with active influenza viruses, these release the thymol, creating a clearly recognisable taste in the mouth.
‘Instead of relying on expensive and complicated testing procedures, we use the natural human sensory system – taste – as a tool for the early detection of infections,’ says Lorenz Meinel.
The principle is flexible: both the flavour carrier and the recognition component can be adapted. For example, the system can be equipped with sweet, bitter or salty flavours – even child-friendly ones. It can also be transferred to different pathogens.
‘For other infections, for example, the virus-specific sugar component could be replaced by a bacteria-specific peptide. The underlying functionality would remain the same,’ explains Lorenz Meinel. The method thus opens up new possibilities for low-threshold diagnostics of viral and bacterial infections – from influenza to future pathogens that are not yet known today.
The researchers are now working on incorporating the sensors into chewing gum or lollipops and making the diagnostic system suitable for mass production. To this end, it is collaborating with FlareOn Biotech GmbH, a start-up founded in 2024 by the University of Würzburg. The development process is expected to take around four years.
The team is convinced that such applications are particularly suitable for critical locations such as schools, nurseries and retirement homes. They could be of crucial importance in containing outbreaks of infection, especially in poorer countries.
Long-term Goal: Tracking the Spread of Influenza in Real Time
The researchers are already thinking further ahead: As soon as an application is available, they would like to ask all users to voluntarily record positive influenza test results using a smartphone app. This data could provide a previously unattainable online overview of the situation, enabling the spread of influenza viruses to be tracked in real time.
Artificial intelligence could then also be used to predict where epidemics or pandemics might develop. This would enable the World Health Organisation, governments, local authorities and even individuals to take precautionary measures at an early stage.
The Federal Ministry of Research, Technology and Space provided financial support for the work as part of the joint project ‘Influ Kau’.
The following were involved:
Dr Heinrich Jehle from the start-up FlareOn Biotech GmbH in Frickenhausen (Esslingen, Baden-Württemberg) contributed to the financing and regulatory advice.
Professors Christian Linz (University Hospital Würzburg, now University Hospital Cologne) and Stephan Hackenberg (University Hospital Würzburg) as well as their teams collected the clinical samples and determined and documented the patients’ state of health.
Professor Jürgen Seibel (Institute of Organic Chemistry, University of Würzburg) and his doctoral student Marcel Groß co-developed the synthesis of the sensor molecule.
Professor Carlos A. Guzmán (Head of the Department of Vaccinology and Applied Microbiology at the Helmholtz Centre for Infection Research in Braunschweig, HZI) conducted investigations on influenza virus particles with teams led by Dr Peggy Riese and Dr Stephanie Trittel.
Reference:
Martina Raschig, Marcus Gutmann, Josef Kehrein, Eberhard Heller, Michael Bomblies, Marcel Groß, A Viral Neuraminidase-Specific Sensor for Taste-Based Detection of Influenza, ACS Central Science, DOI: 10.1021/acscentsci.5c01179.
Powered by WPeMatico
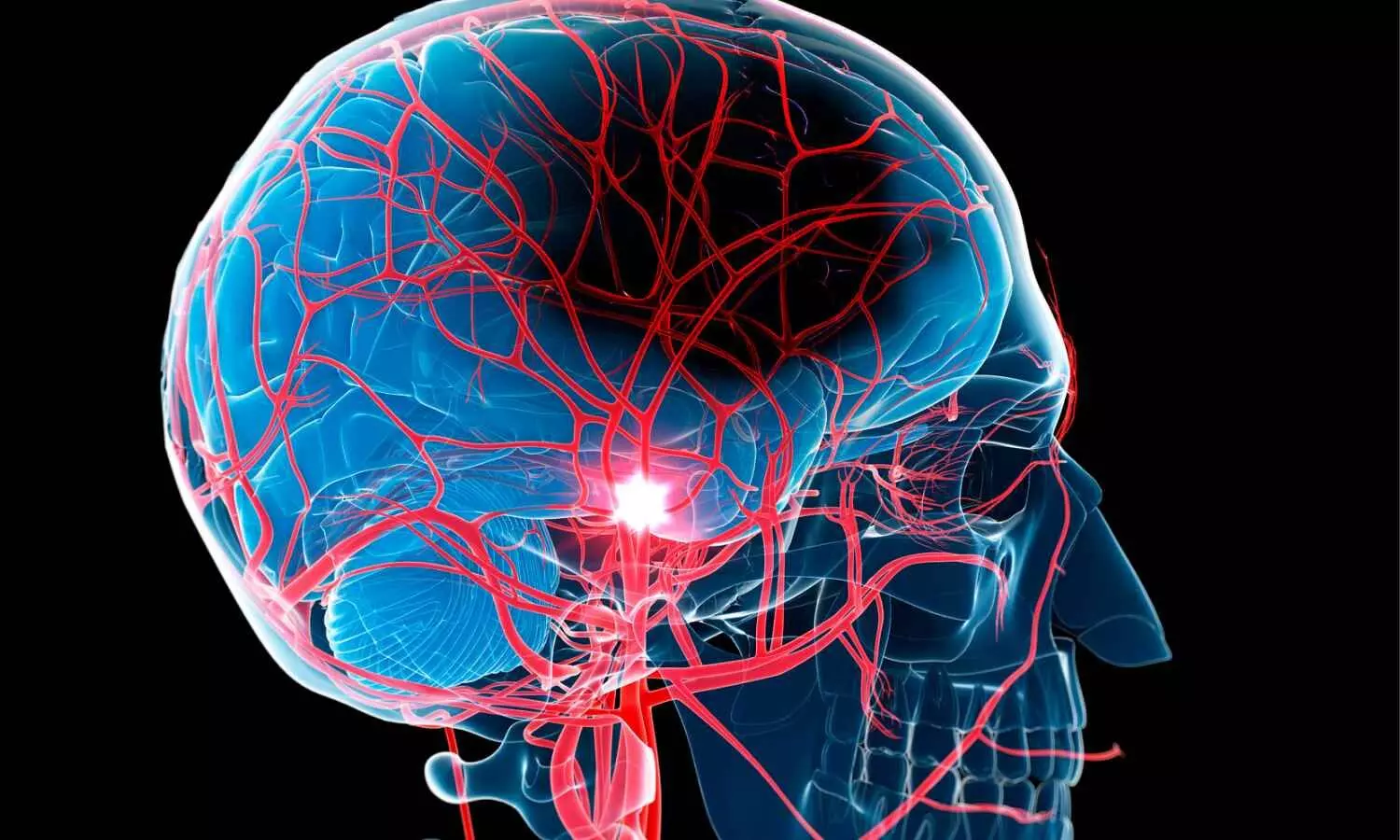
Stroke patients evaluated using telemedicine (telestroke) have higher odds of receiving essential treatment, yet it takes them significantly longer to be treated-potentially limiting the benefits, a Michigan Medicine-led study finds.
Researchers evaluated more than 3,000 patients with ischemic stroke, the most common type, who were potentially eligible for treatment with thrombolysis.
The study used data from 42 hospitals in the Paul Coverdell Michigan Stroke Registry, a program funded by the Centers for Disease Control and Prevention that measures, tracks and aims to improve the quality of care for patients with stroke.
Also called clot-busting medication, thrombolysis is highly time sensitive. National stroke guidelines from the American Heart Association recommend thrombolysis treatment within 60 minutes of a patient arriving to the hospital.
Patients seen using telestroke were 1.6 times more likely to receive clot-busting drugs. However, the time it took for telestroke patients to receive treatment after arriving to the hospital, known as “door-to-needle” time — was nearly seven minutes longer than patients evaluated in person.
Telestroke patients had 44% lower odds of being successfully treated within 60 minutes of getting to the hospital.
Results are published in JAMA Network Open.
“Telestroke care has the potential to revolutionize acute stroke treatment by improving access to lifesaving treatment, but our findings highlight clear gaps in the ability to promptly treat these patients after they are evaluated,” said Brian Stamm, M.D., M.Sc., lead author and clinical assistant professor of neurology at University of Michigan Medical School.
“This is a major opportunity for quality improvement to identify unique factors in telestroke systems that contribute to treatment delays.”
Telestroke evaluations happened more often at rural hospitals and health systems without comprehensive stroke centers.
Investigators also evaluated a subgroup of patients who required transfer to another hospital for advanced stroke treatment and found that it took telestroke patients 47 minutes longer to be transferred, compared to stroke patients evaluated in person.
Delays in hospital transfer may limit a patient’s eligibility for endovascular thrombectomy, a minimally invasive surgical procedure to remove a large blood clot causing stroke.
The American Heart Association recommends that potential candidates for endovascular therapy spend fewer than 90 minutes in the initial transferring emergency department (known as the “door-in-door-out time”), and the Joint Commission recommends this time be less than 120 minutes for all stroke patients.
Past U-M research found that nearly three-quarters of stroke patients who require a transfer wait longer than two hours.
The current study suggests these transfers may take even longer for telestroke patients.
“We know that stroke transfer times are a major problem for the entire stroke care system, but our study highlights particular challenges for telestroke patients,” said Deborah Levine, M.D., M.P.H., senior author and professor of internal medicine and neurology at U-M Medical School.
“Several barriers exist for timely transfer to comprehensive stroke centers, including lack of EMS availability and difficulty finding an accepting facility.”
Stroke providers often use the saying, “Time is brain,” to reflect the importance of speedy acute stroke treatment.
The likelihood of neurologic and functional deficits rapidly increases without timely stroke care. Patients experiencing large vessel ischemic strokes lose nearly 2 million neurons each minute.
In 2010, the AHA created the Target: Stroke program to improve national stroke treatment efficiency. A study conducted four years later found that hospitals participating in the program reduced average door-to-needle treatment times from 74 to 59 minutes.
AHA’s Target: Stroke now has a goal of treating 85% of ischemic stroke patients within 60 minutes of hospital arrival.
In the U-M study, only 60% of patients evaluated using telestroke received thrombolysis within the hour.
“Telestroke has markedly increased access to stroke care and is an essential component of stroke systems,” said co-author Mollie McDermott, M.D., M.S., director of the Stroke Division at U-M Health and clinical associate professor of neurology at U-M Medical School.
“Yet, our findings suggest there is considerable room to ‘move the needle’ on timely stroke treatment for patients evaluated by telestroke.”
Reference:
Stamm B, Whitney RT, Royan R, et al. Telestroke and Timely Treatment and Outcomes in Patients With Acute Ischemic Stroke. JAMA Netw Open. 2025;8(9):e2534275. doi:10.1001/jamanetworkopen.2025.34275
Powered by WPeMatico

Beyond the sneezing and itchy eyes, high pollen seasons are now linked to a significant increase in suicide risk.
A new University of Michigan study found a 7.4% jump in deaths, suggesting the physical discomfort of allergies may trigger a deeper, more dangerous despair, an overlooked factor in suicide prevention.
The study indicates that allergies’ physiological effects, such as poor sleep and mental distress may contribute to this increased risk.
“A small shock could have a big effect if you’re already in a vulnerable state,” said Joelle Abramowitz, associate research scientist at U-M’s Institute for Social Research. “We looked specifically at pollen from all different kinds of plants, including trees, weeds and grasses.”
The effect is incremental. Researchers divided pollen levels into four tiers and found the suicide risk rose with each group: it increased by 4.5% in the second level, 5.5% in the third and peaked at 7.4% in the fourth and highest category.
The study, funded by the American Foundation for Suicide Prevention and U-M ISR, combines daily pollen data from 186 counties of 34 metropolitan areas across the United States, with suicide data from the National Violent Death Reporting System between 2006 and 2018.
Abramowitz and co-authors Shooshan Danagoulian and Owen Fleming of Wayne State University said that while structural factors for suicide are well-researched, short-term triggers are less understood. Pollen allergies are an ideal subject for this research, considering they are an exogenous shock-meaning they are external and not caused by an individual’s mental health status.
“During our study period, there were nearly 500,000 suicides in the U.S.,” Abramowitz said. “Based on our incremental data, we estimate that pollen may have been a contributing factor in up to 12,000 of those deaths over the period, or roughly 900 to 1,200 deaths per year.”
Published in the Journal of Health Economics, the study also found that individuals with a known mental health condition or who had received prior mental health treatment had an 8.6% higher incidence of suicide on days with the highest pollen levels. White men strongly drive the effect, but the study also found an unexpectedly high vulnerability among Black individuals.
“While our study’s data comes from the U.S., our findings likely apply globally,” Abramowitz said. “This is supported by earlier research that found similar relationships in locations like Tokyo and Denmark. Our results, therefore, provide crucial new evidence that this phenomenon is a consistent, worldwide trend.”
The focus should be on public health and education, as reducing the number of pollen-producing plants isn’t a viable option, the researchers suggest. This includes more accurate pollen forecasting and better public communication. Providing people with clear, timely information about high-pollen days allows them to take proactive steps. Additional recommendations are limiting outdoor activities, wearing a mask or having antihistamines on hand.
There is also a need for a broader approach to mental health awareness, the authors said. Health care providers, particularly those in primary care, can benefit from understanding the connection between environmental factors, such as pollen, and patient well-being. This knowledge could help them tailor care more effectively, especially for vulnerable patients, and serve as a prompt to discuss mental health and stress management during high-pollen seasons or other periods of environmental stress.
“We should be more conscious of our responsiveness to small environmental changes, such as pollen, and our mental health in general,” Abramowitz said. “Given our findings, I believe medical providers should be aware of a patient’s allergy history, as other research has also established a connection between allergies and a higher risk for suicide. I hope this research can lead to more tailored care and, ultimately, save lives.”
The authors predict that as climate change extends and intensifies the pollen season, the impact of allergies on suicide rates could more than double by the end of the century.
Reference:
Joelle Abramowitz, Shooshan Danagoulian, Owen Fleming, Seasonal allergies and mental health: Do small health shocks affect suicidality?, Journal of Health Economics, https://doi.org/10.1016/j.jhealeco.2025.103069
Powered by WPeMatico

Researchers have found in a new study that exposure to air pollution is linked with higher risks of mortality, graft failure, and rejection, labelling it as a modifiable environmental factor affecting long-term transplant outcomes. The findings, published in the Clinical Kidney Journal by Kamal Kant Kohli and colleagues, suggest that even after successful kidney transplantation, external environmental exposures may significantly determine patient health.
This shifts focus beyond traditional medical and immunological considerations to broader public health measures that could influence transplant survival. The authors stress that while improvements in surgical techniques and post-transplant medications have enhanced patient outcomes, environmental risk factors such as air quality remain largely overlooked in clinical guidance and long-term care strategies.
The systematic review and meta-analysis evaluated available studies examining the association between ambient air pollution and kidney transplant outcomes. Researchers observed consistent links between poor air quality and higher risks of rejection, graft failure, and all-cause mortality.
These associations highlight the potential biological pathways through which air pollutants, including particulate matter and nitrogen oxides, may trigger systemic inflammation, oxidative stress, and impaired immune function, ultimately affecting the transplanted organ. By synthesizing evidence across multiple studies, the analysis demonstrates that the impact of environmental exposure is not a localized issue but a global health challenge that may compromise the durability of kidney transplants in diverse settings. Importantly, the findings reinforce the need for clinicians to consider environmental health in patient counselling and post-transplant follow-up.
The study concludes that reducing air pollution exposure could serve as an important preventive strategy for improving long-term kidney transplant success. Public health policies aimed at cleaner air, combined with patient-level interventions such as monitoring environmental exposures, may provide new opportunities to protect vulnerable populations. The authors underline that transplant recipients already face multiple risks, and air pollution represents a factor that can be mitigated at both systemic and individual levels. This research therefore bridges nephrology and environmental health, calling for interdisciplinary approaches to safeguard transplant outcomes.
Powered by WPeMatico

Singing can improve the quality of life of people with lung disease and help reduce their symptoms, according to a gold-standard randomised-controlled trial presented at the European Respiratory Society Congress in Amsterdam, the Netherlands .
The study was presented by Professor Natasha Smallwood from Monash University, Melbourne, Australia.
Professor Smallwood told the Congress: “Chronic breathlessness is a common and highly distressing symptom for people with chronic obstructive pulmonary disease and interstitial lung disease. Yet there is a lack of safe, effective, and acceptable treatment options for managing this symptom.
“Group singing is increasingly used to manage symptoms and improve quality of life for people with neurological, mental health, and respiratory conditions, but we need more evidence to prove that this is beneficial, especially for people with interstitial lung disease.”
Interstitial lung disease (ILD) is a general term for a large group of conditions that cause progressive scarring and inflammation of the lung tissue affecting hundreds of thousands of people around world. Chronic obstructive pulmonary disease (COPD) is a serious lung condition affecting around 400 million people worldwide.
The SINFONIA study saw patients take part in a 90-minute online group singing session delivered once a week for 12 weeks over Zoom. The content of the SINFONIA sessions was developed and delivered by a registered music therapist and included dedicated time for warmups, breathing exercises, song singing, and social check ins to foster group connection.
The programme was delivered online to make it as easy as possible to take part, and patients were loaned iPads and given free data plans to help reduce barriers to participation. The group sang songs such as ‘Can’t Help Falling In Love’, ‘Let It Be’, and ‘Pack Up Your Troubles’.
Of the 101 participants, 50 were allocated to the singing sessions and 51 to a group who were given usual care (for example smoking cessation, respiratory vaccines, inhaler therapy, self-management education, and anti-fibrotic medications).
Sixty-four of the patients had chronic obstructive pulmonary disease (COPD), and 37 had interstitial lung disease (ILD).
Patients completed a questionnaire called the SF-36, which records their quality of life across eight sub domains (including pain, social functional, general health and fatigue). These domains are rated from 0 (worst quality of life) to 100 (best quality of life) and then averaged to give a total score.
SF-36 was 7.4 points higher in the singing group compared to the control group.
Professor Smallwood explained: “Compared to usual care, taking part in the SINFONIA singing programme led to improved quality of life for people with chronic obstructive pulmonary disease or interstitial lung disease with chronic breathlessness. These effects were most pronounced amongst people who attended at least 8 of the 12 sessions.
“We saw the greatest improvements in the domains that measured limitations due to physical health or emotional problems,” she adds.
There was also some evidence to suggest that women, people with anxiety or depression, and those who have not previously completed pulmonary rehabilitation experienced the greatest improvements in quality of life as a result of taking part in the online group singing programme.
“The way in which group singing improves quality of life remains unclear and may vary for different participants,” Professor Smallwood added. “But it could be due to better control of breathing, social connection, or mood improvements.”
Dr Apostolos Bossios, Head of the European Respiratory Society’s expert group on airway diseases, asthma, COPD and chronic cough, based at the at Karolinska Institutet, Sweden, who was not involved in the research said: “People with COPD and ILD suffer with long-term breathing difficulties, and this can severely restrict their day to day lives. These conditions cannot be cured, so we need better strategies to help people live happier, healthier lives.
“The world-first SINFONIA study adds to a growing body of evidence that supports using non-medication-based approaches for managing challenging conditions.
“By better understanding how group singing can be incorporated in existing healthcare services, we will be able to make a difference in the lives of patients with lung disease such as COPD and ILD.”
Reference:
Specialised singing programmes can improve the symptoms and quality of life of people with lung disease, European Respiratory Society,Meeting: European Respiratory Society Congress.
Powered by WPeMatico
