10-year clinical trial report finds radiation comparable to surgery for early-stage non-small cell lung cancer
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

New Delhi: Union Health Minister JP Nadda on Monday informed that nine lakh health camps have been held across the country under the ‘Swasth Nari, Sashakt Parivar Abhiyaan.These camps have screened over 3.6 crore people for non-communicable diseases, such as hypertension, diabetes, and cancers.
Speaking at a media event in the national capital, Nadda noted that the health camps have screened over 3.6 crore people for non-communicable diseases, such as hypertension, diabetes, and cancers.
According to an IANS report, “The health initiative that was launched on Prime Minister Narendra Modi’s birthday, and will run till Gandhi Jayanti, is called Swasth Nari, Sashakt Nari. So far, 9,00,000 health camps have been organised and each was attended by specialists. Nearly 3.6 crore have already been screened, and I believe we will cross 4 crore by October 2,” Nadda said.
Also Read:PM Modi launches largest Women and Child Health campaign
At the nationwide health camps, citizens have been screened for hypertension, diabetes, breast cancer, cervical cancer, oral cancer, and anaemia.
The camps also conducted antenatal check-ups, provided life-saving vaccines to children, and nutrition counselling sessions to families.
Further, the health camps also conducted screening for tuberculosis and Sickle Cell Disease, registered blood donors, and issued new Ayushman/PM-JAY cards.
The Health Minister noted that the country’s health policy has changed over the last decade, and a holistic health approach has been introduced since 2014.
“In this approach, we started looking at health by incorporating prevention, health promotion, detection, curative, and palliative parts into our system,” Nadda said.
As part of this continued approach, the government has established 1,79,000 Ayushman Arogya Mandirs, which serve as the first point of contact to connect with 140 crore citizens.
Further, from the very day a woman conceives, ASHA workers start tracking their health, check-up regimen, and share the data with the state government.
He also shared the achievements in the rate of institutional deliveries.
“Our institutional delivery rate has increased from 79 per cent to about 90 per cent. This progress has been possible because we incentivised ASHA workers. For every mother, the delivery is free, and the transportation to the institution and back home is provided by the government,” Nadda said.
He also spoke about the health initiatives launched by PM Modi, such as the Fit India Movement, POSHAN Abhiyan, and Khelo India, to promote a healthy lifestyle.
The Minister also highlighted a positive change in mental health awareness, and that the availability of high-quality medicines has supported people in leading a normal and healthier life.
Also Read:Delhi Govt to empanel 100 additional hospitals under Ayushman Bharat
Powered by WPeMatico
A new study published in the Frontiers in Cardiovascular Medicine showed that wearable technology for monitoring pulmonary congestion in heart failure (HF) patients decreased the risk of both hospitalization and mortality by 37%.
Hospitalizations for HF have a considerable predictive impact. They are expensive, intrusive, and have no discernible mortality benefit, yet, implanted hemodynamic monitors can identify early congestion.
Although it may not be a reliable indicator of decompensation, body weight is frequently tracked as an outpatient for the onset of congestion. An alternative to intrusive methods of monitoring traffic is provided by wearable technology. Therefore, in comparison to conventional therapy, this meta-analysis was carried out to investigate the effectiveness of wearable devices in lowering HF hospitalizations and death.
PRISMA criteria were followed in conducting a systematic review and meta-analysis. Trials comparing wearable device-guided care with conventional HF therapy were found by searching the PubMed, MEDLINE, EMBASE, and Cochrane databases.
Hospitalization for heart failure, worsening heart failure events (hospitalization or ED visit for heart failure), and all-cause death were among the outcomes. Random effect models were used to do meta-analyses of total (first and recurring) events.
All the 958 individuals who were enrolled at the time of or within 10 days after being discharged from a hospitalization for heart failure were included in 4 trials that satisfied the inclusion criteria.
When compared to standard treatment, wearable device-guided therapy led to a 40% decrease in HF occurrences (RR: 0.60, 95% CI: 0.42–0.86, p = 0.005) and a 41% decrease in hospitalizations for HF (RR: 0.59, 95% CI: 0.41–0.87, p = 0.007).
The wearable monitoring arm saw a 26% decrease in all-cause mortality (RR: 0.74, 95% CI: 0.55–0.99, p = 0.04).
Wearable monitoring resulted in a 37% reduction in the composite outcome of HF hospitalization and death (RR: 0.63, 95% CI: 0.44–0.91, p = 0.04).
All-cause mortality and HF hospitalizations were decreased in newly admitted patients when treatment for HF was directed by wearable technology that measures pulmonary congestion.
Overall, across the range of EF, HF therapy guided by wearable devices that identify pulmonary congestion decreased HF hospitalizations and mortality. When transferring treatment from the acute to the home environment, wearable monitoring may offer more protection against unfavorable outcomes. This approach proved successful in patients with characteristics indicating a worse prognosis, such as a recent hospitalization.
Reference:
Murray, C. P., Kenny, A. P., O’Sullivan, N. J., Murphy, R. T., & Curtain, J. P. (2025). Efficacy of wearable devices detecting pulmonary congestion in heart failure: a systematic review and meta-analysis. Frontiers in Cardiovascular Medicine, 12, 1612545. https://doi.org/10.3389/fcvm.2025.1612545
Powered by WPeMatico
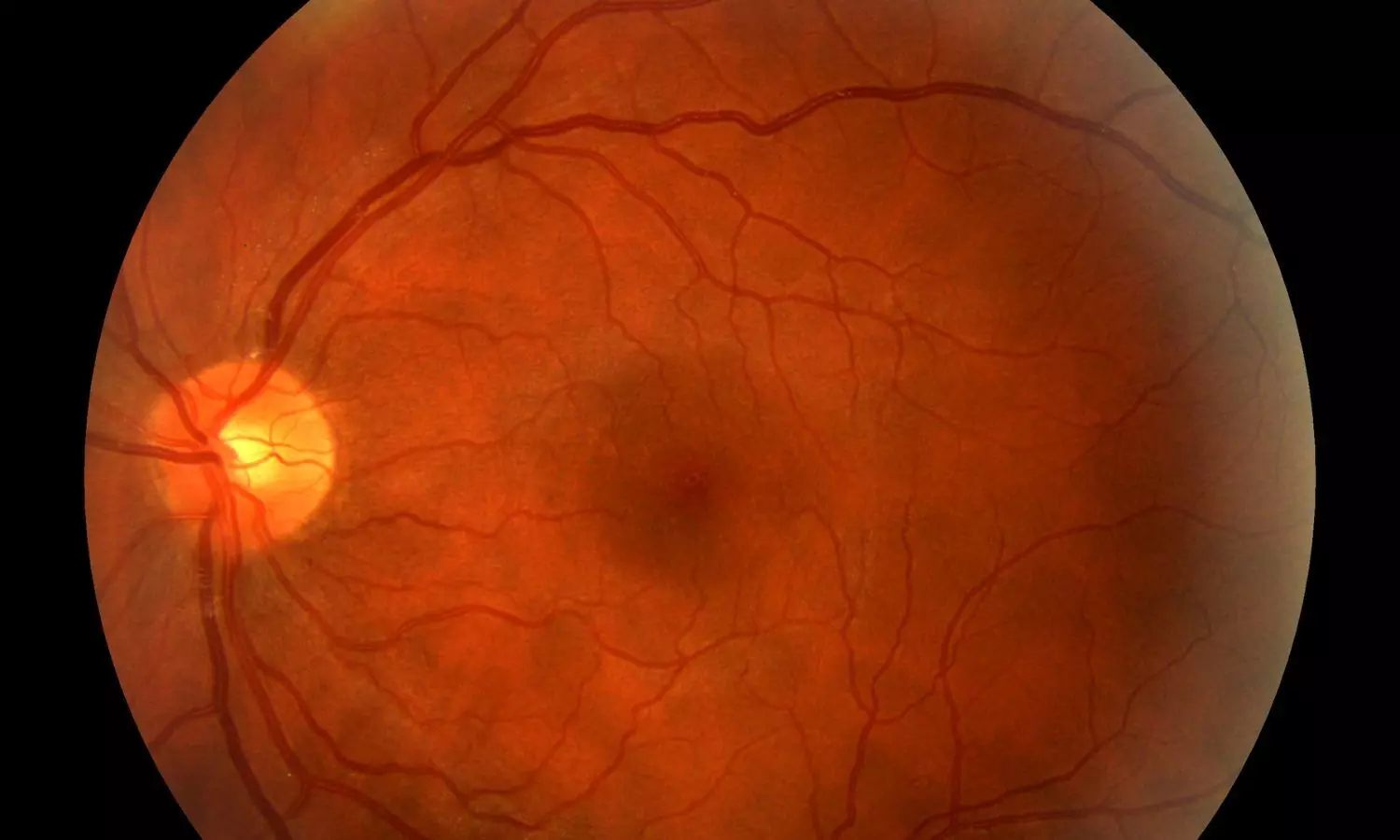
USA: A recent study published in Frontiers in Endocrinology has shed light on a critical finding: diabetic retinopathy (DR) and diabetic nephropathy (DN)—two major microvascular complications in type 2 diabetes—do not always progress in parallel. Conducted by Dr. Ashley Fitzgerald and colleagues from the Department of Ophthalmology and Visual Sciences, University of New Mexico School of Medicine, the cross-sectional case-control study aimed to evaluate the degree of concordance between the severity of DR and DN in a New Mexican diabetic population.
To explore this relationship, researchers analyzed data from two distinct patient groups—one with end-stage renal disease (ESRD, Stage 5, on dialysis) and the other with early-stage DN (Stage 1 or 2). The ESRD group included 164 individuals with severely reduced kidney function (eGFR <15 mL/min), while the mild DN group comprised 165 patients with relatively preserved kidney function (eGFR >60 mL/min). Retinal status was evaluated through dilated fundus examinations, and systemic clinical parameters were extracted from retrospective chart reviews.
The following were the key findings of the study:
Despite its findings, the study acknowledges several limitations, including its retrospective nature and missing data from patient records, which may introduce selection bias. Some patients had irregular follow-ups, making it difficult to capture the full progression of complications. Additionally, race and ethnicity were self-reported and inconsistently recorded, potentially affecting statistical interpretations.
The researchers concluded that while DR and DN share several modifiable risk factors, their progression is not necessarily synchronous. Relying solely on glycemic control is inadequate for predicting the severity of either condition. Therefore, both complications should be assessed independently, taking into account individual clinical profiles and risk markers. The team also hypothesized that genetic variability may play a role in the discordant progression patterns, with some individuals being genetically predisposed to more aggressive forms of one complication over the other.
“The study emphasizes the importance of individualized assessment and the need for further longitudinal research to better understand the mechanisms underlying the divergence between diabetic eye and kidney disease progression,” the researchers wrote.
Reference:
Fitzgerald, A., Das, R., Moezzi, C. J., Salazar, S. R., Mankad, R., Qualls, C. R., Cabrera, A., Kathuria, A., Monickaraj, F., Tzamaloukas, A., & Das, A. (2025). Discordance of diabetic retinopathy severity in a cohort of diabetic nephropathy patients: A cross-sectional case-control study in a new Mexican population of type 2 diabetes. Frontiers in Endocrinology, 16, 1638415. https://doi.org/10.3389/fendo.2025.1638415
Powered by WPeMatico
In 2023, the groundbreaking Australian BANDIT (Baricitinib in New Onset Type 1 Diabetes) trial reported that a daily pill of baricitinib, commonly prescribed for rheumatoid arthritis and alopecia, could safely preserve the body’s own insulin production and slow the progression of type 1 diabetes (T1D) in people recently diagnosed with the condition.
Now the follow-up of the blinded BANDIT trial, being presented at this year’s Annual Meeting of The European Association for the Study of Diabetes (EASD), Vienna (15-19 Sept), reveals that once baricitinib treatment was stopped, participants’ diabetes progressed-they produced less insulin and had less stable blood sugar levels, that were not significantly different to those on placebo.
“Among the promising agents shown to preserve beta cell function in T1D, baricitinib stands out because it can be taken orally, is well tolerated, including by young children, and is clearly efficacious”, said author Dr Michalea Waibel from St Vincent’s Institute of Medical Research, Fitzroy, Australia.
She added, “These latest data support our previous clinical trial data by showing that the therapeutic effect is lost when baricitinib is stopped and justify further trials to determine if treatment benefit can be sustained over many years on treatment and if treating earlier stages of disease can prevent or delay clinical diagnosis.”
T1D is caused by the immune system mistakenly attacking the insulin-producing cells in the pancreas. Over time, this leads to the need for lifelong insulin injections to manage blood sugar levels.
Baricitinib, a Janus kinase (JAK) inhibitor, works by blocking signals in the body that lead to overactivity of the immune system, and helps to protect the remaining insulin-producing cells in people who are newly diagnosed with T1D, thus delaying progression of full-blown symptoms. It is already prescribed to treat several autoimmune diseases, including rheumatoid arthritis, ulcerative colitis, and alopecia.
The BANDIT trial enrolled 91 people aged between 10 and 30 years old who had been diagnosed with T1D in the previous 100 days. Participants were either given a baricitinib pill (4mg) or a placebo, once daily for 48 weeks.
At the beginning of the trial and at weeks 12, 24 and 48, researchers measured participants’ C-peptide levels (a marker of insulin secretion) to find out how much insulin participants could make themselves. They also used continuous glucose monitoring and HbA1c (a marker of longer-term blood sugar levels) to assess the need for injected insulin and how well blood sugar levels were managed.
The findings revealed that takingly a daily pill of baricitinib for 48 weeks preserved insulin-producing beta cell function, decreased blood glucose fluctuations, and reduced the need for insulin in people with newly diagnosed T1D. The researchers also found that baricitinib was safe, with no side effects attributed to the drug.
In this study, researchers report the findings from the off-drug follow-up period, with assessments done at weeks 72 and 96.
At 48 weeks the C-peptide level was 0.65 in the baricitinib group and 0.43 in the placebo group. After treatment was stopped, C-peptide levels fell to 0.49 in the baricitinib group and 0.36 in the placebo group at 72 weeks, and then to 0.37 and 0.26, respectively, at 96 weeks, demonstrating reduced insulin production.
The fall in insulin-producing beta cell function after baricitinib treatment was stopped resulted in the need for more insulin treatment, with insulin requirements at weeks 72 and 96 that were not significantly different between the groups.
Baricitinib cessation also led to a deterioration in glucose control, with differences in the time spent in the safe glucose range and blood glucose fluctuations between the groups in the first 48 weeks, no longer statistically significant at weeks 72 and 96.
Further analyses were unable to identify any characteristic at the start of the trial that predicted treatment response, including age, specific immune system genes known as human leukocyte antigens (HLA), body mass index (BMI), or number of autoantibodies. Moreover, drug adherence (at least 80% of study drug taken) did not distinguish responders from non-responders. Overall, around two-thirds of participants taking baricitinib met the criteria for response.
Notably, there was no additional safety concerns raised in the follow-up period.
“This is a really exciting step forward. For the first time, we have an oral disease-modifying treatment that can intervene early enough to allow people with T1D to be significantly less dependent on insulin treatment and provide time free from the demands of the disease’s daily management, and which could also lower rates of long-term complications,” said Dr Waibel.
She added, “If we can identify people at high risk of developing type 1 diabetes with genetic tests and blood markers, they could be offered treatment even earlier to prevent the disease taking hold in the first place. We are hopeful that larger phase III trials with baricitinib are going to commence soon, in people with recently diagnosed T1D as well as in earlier stages to delay insulin dependence. If these trials are successful, the drug could be approved for T1D treatment within 5 years.”
Reference:
Fresh hope for type 1 diabetes as daily pill that slows onset confirms promise at 2-year follow-up, European Association for the Study of Diabetes, Meeting: Annual Meeting of the European Association for the Study of Diabetes (EASD).
Powered by WPeMatico
A new study has found that prompt administration of opioid pain relief in emergency departments reduces the likelihood of hospitalization for children with sickle cell disease, according to findings published in JAMA Pediatrics.
Sickle cell disease (SCD) is a genetic blood disorder that can cause severe episodes of intense pain due to blocked blood flow. While national guidelines recommend prompt opioid treatment, this study is among the first to quantify the impact of timing on hospitalization rates, said Elizabeth Alpern, MD, MSCE, the George M. Eisenberg Professor and Vice Chair in the Department of Pediatrics at Northwestern University Feinberg School of Medicine, who was a co-author of the study.
“There hasn’t been prior work that shows if timely pain relief can impact important patient-centered outcomes like admission to the hospital,” said Alpern, who is also head of the Division of Emergency Medicine at Ann & Robert H. Lurie Children’s Hospital of Chicago. “If we can stabilize and treat patients’ pain, they won’t need to be admitted to the hospital, where they would miss school, their families would miss work, and it’s disruptive to their lives.”
In the study, investigators analyzed data from the Pediatric Emergency Care Applied Research Network Registry, reviewing over 9,000 emergency department (ED) visits by 2,538 children under the age of 19 between 2019 and 2021. The findings offer compelling evidence that faster pain management can lead to better outcomes for pediatric patients with SCD, said Jacqueline Corboy, MD, Assistant Professor of Pediatrics in the Division of Emergency Medicine at Northwestern University Feinberg School of Medicine, who was also a co-author of the study.
“We were able to statistically show that if patients receive a timely first dose of opioid medications and a timely second dose of opioid medications, we could drastically reduce the number of hospital admissions within this population,” said Corboy, who is Director Of Quality in the Division of Emergency Medicine at Lurie Children’s. “This is the first study that shows concrete evidence, so this is really important.”
The study focused on two key time intervals: the time from ED arrival to the first opioid dose, and the time between the first and second doses. Children who received their first dose within 60 minutes of arrival were less likely to be hospitalized. The odds of hospitalization dropped even further when the second dose was administered within 30 minutes of the first.
The combination of a first dose within one hour and a second dose within 30 minutes was associated with a reduction in hospitalization odds compared to less timely treatment, according to the study. Even when the second dose was delayed up to 60 minutes, timely first-dose administration still showed a protective effect.
Alpern and Corboy said they hope the results will inform future clinical guidelines and improve care standards for children with SCD nationwide.
“Our next steps are to continue to improve the processes that we have through the ED and work collaboratively with our inpatient partners, nurses and paramedics. We want to ensure that everybody’s included as we implement these quality initiatives to improve care for our patients,” Corboy said.
The study was a collaborative effort among 12 pediatric hospitals, Alpern said, and data collected will be studied further as part of the Pediatric Emergency Care Applied Research Network.
“We’ve utilized electronic health record data that’s centralized and harmonized to see how this impacts operations and outcomes,” said Alpern, who is Principal Investigator of the PECARN Registry. “The information that we have as a result helps us understand, in a much larger setting, how we can be effective.”
Reference:
Gwarzo I, Coleman KD, McKinley K, et al. Opioid Timeliness in the Emergency Department and Hospitalizations for Acute Sickle Cell Pain. JAMA Pediatr. Published online September 02, 2025. doi:10.1001/jamapediatrics.2025.2967
Powered by WPeMatico
