Sleep fragmentation negatively linked to QoL in pediatric nocturnal enuresis
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Endometrial cancer (EC) ranks among the top three gynecologic malignancies globally, with rising incidence in younger populations driven by obesity, metabolic disorders, and lifestyle factors. Despite its prevalence, effective population-level screening remains elusive due to limitations in current methods: transvaginal ultrasound (TVU) exhibits moderate specificity (60–70%), cytology sensitivity is ≤50% in community settings, and histopathology is invasive. This review synthesizes advances in EC screening, highlighting emerging technologies poised to transform early detection.
Clinical Symptoms & Imaging:
• Vaginal bleeding is the primary symptom but lacks specificity due to overlap with benign conditions.
• TVU detects endometrial thickening (>4 mm in postmenopausal women) but misses 35% of early-stage/hormone-independent tumors (Type II EC). Sensitivity: 80–90%; specificity: 60–70%.
Tumor Markers:
• CA125 and HE4 correlate with advanced disease but lack utility for early detection. HE4 specificity is compromised by heterogeneity across studies.
Histopathology:
• Gold standard but invasive, with risks of complications and low patient compliance. Novel samplers (e.g., Pipelle, Tao Brush) enable outpatient cytology yet face challenges in detecting focal lesions.
1. Molecular & Epigenetic Biomarkers
• DNA Methylation Panels (e.g., ADCYAP1, HAND2):
• Phase II trials show 89–94% sensitivity and 91–97% specificity in liquid biopsies.
• Enables non-invasive early detection and monitoring of high-risk groups (e.g., Lynch syndrome).
• Genomic Profiling:
• Mutations in PTEN, TP53, and ARID1A achieve 92.9% sensitivity for hereditary EC.
• Exosomal miRNA:
• Plasma exosomal miR-15a-5p distinguishes EC patients (AUC: 0.823) and correlates with myometrial invasion depth.
2. Liquid Biopsy & Spectroscopy
• Circulating Tumor DNA (ctDNA):
• Combined with tumor-educated platelets, sensitivity reaches 77.8% for early-stage EC. Challenges include standardization and high cost.
• Vibrational Spectroscopy:
• Detects molecular changes in tissues/blood with 87% sensitivity and 78% specificity. Enables rapid intraoperative diagnosis.
3. AI-Driven Platforms
• Risk Prediction Models:
• Integrate demographic, imaging, and biomarker data (e.g., AI-enhanced Risk of Malignancy Index: 94% sensitivity, 75% specificity).
• Cytology Analysis:
• Deep learning algorithms classify benign/malignant cells (95% positive predictive value).
1. Risk Stratification
• High-Risk Groups: Obesity (BMI >30), Lynch syndrome, diabetes, nulliparity, and late menopause (>55 years).
• Lynch Syndrome: Annual TVU + endometrial biopsy from age 30–35.
2. Fertility Preservation
• Early-stage EC: Progestins, levonorgestrel IUDs, or GnRH agonists enable fertility-sparing treatment with 3–6 month follow-ups.
3. Economic & Ethical Considerations
• Cost-Effectiveness: AI and methylation testing reduce long-term costs by minimizing invasive procedures (e.g., Nordic studies show 20% cost reduction over 5 years).
• Ethical Priorities: Minimize invasiveness, address false-positive anxiety, and ensure equitable access.
Multimodal Screening: Combine methylation panels, exosomal miRNAs, and AI for community-level deployment.
Large-Scale Validation: Prospective trials to confirm biomarker efficacy across diverse populations.
Policy Integration: Develop guidelines for risk-stratified screening and subsidize high-accuracy tests (e.g., methylation panels).
Endometrial cancer screening is evolving from symptom-dependent approaches to precision strategies leveraging molecular biomarkers, AI, and non-invasive diagnostics. Key innovations—methylation panels (sensitivity >90%), vibrational spectroscopy, and exosomal miRNAs—offer transformative potential for early detection. Prioritizing risk-adapted frameworks, cost-effective implementation, and ethical deployment will be critical to reducing EC mortality globally.
Reference:
Liu H, Ai H, Liu Y. Exploring the Current State and Research Innovation in Endometrial Cancer Screening. Oncol Adv. 2025;3(1):50-60. doi: 10.14218/OnA.2024.00034.
Powered by WPeMatico

A new study published in the Journal of American Medical Association revealed that the necessity of including smoking cessation into addiction treatment programs is demonstrated by the 30% increased chance of recovery from non-tobacco addictions among smokers with drug use disorders who stopped cigarettes.
People with other substance use disorders (SUDs) are more likely to smoke cigarettes than people without SUDs. However, SUD treatment centers frequently lack smoking cessation programs. Thus, to validate if switching from present to past smoking is linked to sustained SUD recovery, this study was carried out to evaluate smoking status and SUD recovery across time.
Using data from the PATH (Population Assessment of Tobacco and Health) research, a nationally representative cohort of US people with a history of SUD participated in this cohort research. In the United States, the PATH Study is a continuous longitudinal cohort study that is nationally representative.
Adults (≥18 years old) in the wave 1 cohort (hired in 2013/2014) who were evaluated yearly for 4 years until wave 4 (2016/2018) were included in the analyses. Sensitivity analysis also evaluated a second nationally representative cohort (2016/2018–2023).
Data analysis was finished between June and September of 2024. Using the Global Appraisal of Individual Needs–Short Screener SUD subscale, the main outcome was SUD recovery, which was defined as either high lifetime SUD symptoms with no past-year symptoms or high lifetime SUD symptoms with any past-year symptoms.
The mean age of 2,652 adults from 2013/2014 to 2016/2018 was 39.4 years (95% CI, 38.7-40.3), and 41.9% of participants (95% CI, 39.4%-44.4%) were female.
13.9% (95% CI, 12.2%-15.6%) of participants were non-Hispanic Black, 63.1% (95% CI, 60.4%-65.7%) were non-Hispanic White, 17.0% (95% CI, 15.3%-18.9%) were Hispanic, and 6.0% (95% CI, 4.9%-7.4%) were another non-Hispanic race (Asian, Native Hawaiian/Other Pacific Islander, Native American/Alaska Native, more than one race).
After controlling for time-varying covariates and between-person variations, there was a positive correlation between SUD recovery and within-person change from current to former smoking: year-to-year change to former cigarette use was linked to a 30% increase in odds of recovery (odds ratio [OR], 1.30; 95% CI, 1.07-1.57).
Both in the second cohort evaluated from 2016/2018 to 2022/2023 (OR, 1.37; 95% CI, 1.13-1.66) and after trailing predictor by 1 year (OR, 1.43; 95% CI, 1.00-2.05), this connection remained significant.
Overall, recovery from other SUD was linked to a person’s transition from current to past smoking. These findings imply that quitting smoking may be a useful strategy to support SUD recovery and enhance health in adults.
Source:
Parks, M. J., Blanco, C., Creamer, M. R., Kingsbury, J. H., Everard, C. D., Marshall, D., Kimmel, H. L., & Compton, W. M. (2025). Cigarette smoking during recovery from substance use disorders. JAMA Psychiatry (Chicago, Ill.). https://doi.org/10.1001/jamapsychiatry.2025.1976
Powered by WPeMatico

Researchers at the Icahn School of Medicine at Mount Sinai have found that prenatal exposure to acetaminophen may increase the risk of neurodevelopmental disorders, including autism spectrum disorder and attention-deficit/hyperactivity disorder (ADHD), in children. The study, published today in BMC Environmental Health, is the first to apply the rigorous Navigation Guide methodology to systematically evaluate the rigor and quality of the scientific literature.
Acetaminophen (often sold under the brand name Tylenol®, and known as paracetamol outside the United States and Canada) is the most commonly used over-the-counter pain and fever medication during pregnancy and is used by more than half of pregnant women worldwide. Until now, acetaminophen has been considered the safest option for managing headache, fever, and other pain. Analysis by the Mount Sinai-led team of 46 studies incorporating data from more than 100,000 participants across multiple countries challenges this perception and underscores the need for both caution and further study.
The Navigation Guide Systematic Review methodology is a gold-standard framework for synthesizing and evaluating environmental health data. This approach allows researchers to assess and rate each study’s risk of bias, such as selective reporting of the outcomes or incomplete data, as well as the strength of the evidence and the quality of the studies individually and collectively.
“Our findings show that higher-quality studies are more likely to show a link between prenatal acetaminophen exposure and increased risks of autism and ADHD,” said Diddier Prada, MD, PhD, Assistant Professor of Population Health Science and Policy, and Environmental Medicine and Climate Science, at the Icahn School of Medicine at Mount Sinai. “Given the widespread use of this medication, even a small increase in risk could have major public health implications.”
The paper also explores biological mechanisms that could explain the association between acetaminophen use and these disorders. Acetaminophen is known to cross the placental barrier and may trigger oxidative stress, disrupt hormones, and cause epigenetic changes that interfere with fetal brain development.
While the study does not show that acetaminophen directly causes neurodevelopmental disorders, the research team’s findings strengthen the evidence for a connection and raise concerns about current clinical practices.
The researchers call for cautious, time-limited use of acetaminophen during pregnancy under medical supervision; updated clinical guidelines to better balance the benefits and risks; and further research to confirm these findings and identify safer alternatives for managing pain and fever in expectant mothers.
“Pregnant women should not stop taking medication without consulting their doctors,” Dr. Prada emphasized. “Untreated pain or fever can also harm the baby. Our study highlights the importance of discussing the safest approach with health care providers and considering non-drug options whenever possible.”
With diagnoses of autism and ADHD increasing worldwide, these findings have significant implications for public health policy, clinical guidelines, and patient education. The study also highlights the urgent need for pharmaceutical innovation to provide safer alternatives for pregnant women.
Reference:
Prada, D., Ritz, B., Bauer, A.Z. et al. Evaluation of the evidence on acetaminophen use and neurodevelopmental disorders using the Navigation Guide methodology. Environ Health 24, 56 (2025). https://doi.org/10.1186/s12940-025-01208-0
Powered by WPeMatico

A recent real-world study conducted in China has confirmed that baricitinib, a Janus kinase (JAK) inhibitor, significantly improves hair regrowth in patients with various forms of alopecia areata, including totalis, universalis, and eyebrow/eyelash loss. The study observed a substantial reduction in the Severity of Alopecia Tool (SALT) scores, with an average improvement from 70.21 at baseline to 48.51 after treatment. A total of 47 patients met inclusion criteria. At weeks 12 and 24, 47% and 53% achieved SALT 20, respectively. By the end of treatment (24–104 months), 78.7% achieved SALT 20. The overall SALT score improvement before and after treatment was 48.51 (±30.36), with a hair regrowth rate of 68.10% ± 35.45%. Patients with disease duration ≤ 4 years showed significantly greater SALT score improvement and shorter time to hair regrowth onset compared to those with > 4 years. At week 24, 85.2% and 90.4% achieved ClinRO scores of 0/1 for eyebrow and eyelash alopecia, respectively. Negative correlations were observed between disease duration and hair regrowth rate, a positive correlation was found between treatment duration and hair regrowth rate. Baricitinib was well tolerated with no serious adverse events. These findings align with previous research supporting baricitinib’s efficacy and safety in treating severe alopecia areata. The study’s results suggest that baricitinib is a promising treatment option for patients with various forms of alopecia areata, offering significant improvements in hair regrowth without serious side effects.
Reference:
Wada-Irimada, M., Takahashi, T., Sekine, M., et al. (2025). Long-term real-world outcomes of baricitinib in severe alopecia areata: A 104-week retrospective analysis from a single institute. Journal of Dermatology. https://doi.org/10.1111/1346-8138.17829
Keywords: baricitinib, alopecia areata, hair regrowth, SALT score, real-world study, JAK inhibitor, totalis, universalis, eyebrow loss, eyelash loss.
Powered by WPeMatico

Physical activity (PA) is associated with significant
positive impacts on both physical and mental health in non-pregnant populations.
Several health organisations have strongly suggested that PA is directly
correlated to a lower risk of heart disease, diabetes type 2, metabolic
syndrome, anxiety, and some types of cancer. Considering the physical changes
that occur during pregnancy, the maternal lifestyle can be a modifying factor
for both maternal and foetal health. For example, pregnant women are at risk of
pregnancy complications such as gestational diabetes and preeclampsia, which
are related to maternal obesity and inactivity.
Traditionally, pregnancy constitutes a barrier to PA due to
certain factors, beliefs, and lifestyle restraints. Moreover, pregnancy related
symptoms, including vomiting, abdominal discomfort, and easy fatigue, along
with safety concerns as well as limited scientific in formation and social
support, have steered pregnant women away from being active. However, over the
last few decades, scientific societies have issued guidelines recommending that
pregnant women without complications should engage in PA. For example, the
American College of Obstetricians and Gynecologists (ACOG) recommends at least
150 min of moderate-intensity PA per week. Despite these recommendations, only
a small percentage of pregnant women actually meet them. Few studies, with
limited numbers of cases, have examined PA levels during pregnancy in some
parts of the world. These studies used questionnaires with a small number of
participants and compared the data with the data collected using smartwatches
to estimate actual PA levels.
The pregnancy physical activity questionnaire (PPAQ) is
specially designed for pregnant women, which considers several hinderances that
women face during pregnancy. Several advantages, such as low cost, easy
implementation, self-administration, and ease of accessing a high volume of
individuals, make the questionnaire a suitable means to evaluate and promote PA
in a large population. The PPAQ has been translated into several languages and
adopted by various cultures, including the recently introduced Greek version.
This study aimed to record the degree of PA in pregnant Greek women during the
three trimesters of pregnancy and examine possible associations with
gestational age (GA), maternal age, education, and population of the
residential area. Authors tested the Greek version of the PPAQ and examined the
reliability of answers using a smartwatch in several cases.
This prospective study comprised two stages. The first stage
was the completion of the PPAQ Greek version twice, with a one-week interval
between the two rounds, to assess internal consistency and repro ductivity. The
validity was evaluated by comparing the PPAQ results with data from
smartwatches that recorded step counts and metabolic equivalent tasks (METs).
The second stage included pregnant women from various regions of Greece that
completed the PPAQ once during their pregnancy. The level of PA during
pregnancy and consistency with the international PA recommendations was
evaluated with the use of METs.
A total of 1058 pregnant women filled the PPAQ Greek
version, while eighteen women randomly participated in the reliability and
validity analyses of the PPAQ. Results from the PPAQ completed one week apart
showed strong agreement (Intraclass Correlation Coefficient [ICC]: 0.82–0.96).
A comparison between the PPAQ results and smartwatch data revealed no
significant differences in PA levels (correlation coefficient: 0.542; p =
0.022). The median total PA for all the participants was 142.1 MET-hours/week
(interquartile range: 106.04 MET-hours/week).
PA levels increased with advancing gestation in
sports/exercise (1st vs. 2nd trimester, p = 0.048; 2nd vs. 3rd trimester, p
< 0.001), occupational activities (1st vs. 3rd trimester, p < 0.001; 2nd
vs. 3rd trimester, p = 0.024), and transportation activities (1st vs. 3rd
trimester, p < 0.001; 2nd vs. 3rd trimester, p < 0.001).
Moderate-to-vigorous intensity activities also increased
with gestational age (p = 0.023, 95 % confidence interval [CI]: 0.1–1.4; p =
0.045, 95 % CI: 0–0.08, respectively).
Women were more active in household/ caregiving activities
across all trimesters (p = 0.017; 95 % CI: 0.09–0.95).
Women with higher educational levels were more likely to
engage in sports/exercise (p = 0.039, 95 % CI: − 3.3 to − 0.08) and had higher
overall PA levels (p = 0.029, 95 % CI: 0.37–6.3). However, only 14.8 % of the
participants met the international PA recommendations for pregnancy.
The results of this study demonstrate that the total PA
during pregnancy increases with advancing gestation. Women become more
physically active as pregnancy progresses, mainly in terms of household and
sports/exercise activities. A possible explanation is that women are familiar
with this new condition and might feel confident about the well-being of their
pregnancy. In addition, fear of a potential miscarriage and several symptoms
that are present in early pregnancy (fatigue, nausea, and vomiting) also play a
significant role in preventing pregnant women from engaging in activities.
Regarding the mode of conception, pregnant women who conceived through ART had
a significantly lower total level of PA, with similar findings for all
subcategories, except for vigorous-intensity and sedentary activities. Women
who conceived spontaneously performed significantly fewer sedentary activities
than those in the ART group. Most couples using ART are older and have experienced
from long-term infertility. Authors postulated that these women are
overcautious in protecting their pregnancy, which was achieved through
additional effort; thus, it is difficult for them to adopt an active lifestyle.
Another interesting point is the association between
maternal educational level, residential area population, and PA. Although the
total amount of PA between the two groups was similar, pregnant women with
higher educational levels performed significantly more sports/exercise
activities. This may be because well-educated people are usually better
informed and open to following new habits and recommendations. As far as
residential areas are concerned, broad and easy access to multiple exercise or
sports activities for citizens in areas with large populations could explain
our significant results. Moreover, the regression analysis showed that women of
advanced maternal age compared to younger ones, are more physically active in
most of the PA intensities, mainly referring to moderate and vigorous
activities. This finding is of great significance because it highlights the
fact that younger women participate in less energy “demanding” activities,
while the total level of PA does not differ. Pregnant women at a greater GA
conduct more household/caregiving activities. Furthermore, women with a
university degree were more likely to meet the recommendations for
moderate-intensity exercise during pregnancy.
The Greek version of the PPAQ is a reliable and valid tool
for assessing the PA levels in pregnant women. Moreover, the results of this
study demonstrate that pregnant women in the 3rd trimester, those with a higher
educational level, and those living in cities with large populations were more
active in sports and exercise. On the other hand, those who conceived of using
ART were less physically active. This highlights the need for clinicians to
promote PA during pregnancy in Greece so that exercise is part of the daily
routine of pregnant women.
Source: I. Mitrogiannis et al.; European Journal of
Obstetrics & Gynecology and Reproductive Biology 307 (2025) 29–33
Powered by WPeMatico
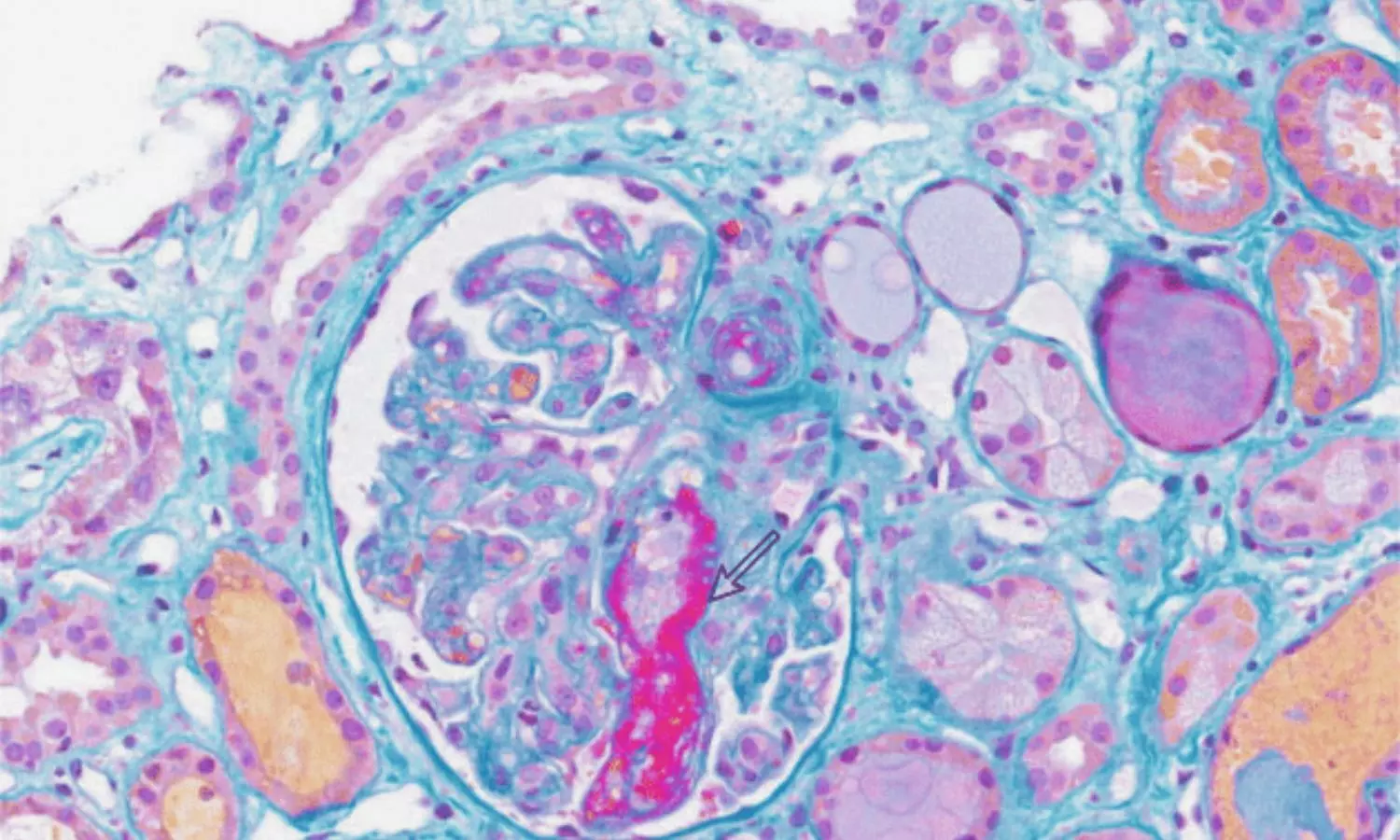
China: A team from The Second Clinical College of Guangzhou University of Chinese Medicine, led by Rui Jiang, has documented a rare case of bevacizumab-associated glomerular microangiopathy (Bmab-GMA) in BMC Nephrology, adding to growing evidence of serious kidney-related side effects tied to the cancer drug.
The case involved a 59-year-old man with stage IIIA right lung adenocarcinoma who underwent surgery in 2021, followed by targeted treatment with bevacizumab after developing metastatic disease in 2023. Within months of initiating therapy, the patient developed new-onset high blood pressure, swelling in the lower limbs, and worsening proteinuria. Laboratory tests confirmed progressive kidney dysfunction, with rising serum creatinine levels and falling serum albumin.
Despite dose reduction and eventual discontinuation of bevacizumab, kidney damage persisted. Upon admission in April 2024, the patient’s 24-hour urine protein excretion was markedly elevated at over 4.6 g/day, while his estimated glomerular filtration rate had dropped to 41.27 mL/min/1.73 m². Blood tests also revealed increased levels of the soluble complement membrane attack complex (C5b-9), indicating possible activation of the complement system — a clue that may shed light on the disease mechanism.
Renal biopsy provided definitive evidence of Bmab-GMA. Microscopic examination revealed mesangial expansion, double-contour formation of the glomerular basement membrane, and pseudothrombotic deposits. Immunofluorescence showed deposition of multiple immunoglobulins and complement components, while electron microscopy identified subendothelial and mesangial electron-dense deposits, widening of the subendothelial space, and partial loss of podocyte foot processes.
These findings confirmed the diagnosis of bevacizumab-induced glomerular microangiopathy, a condition that can cause both acute kidney injury and nephrotic syndrome. Notably, the case mirrors previous reports linking anti-VEGF agents, such as bevacizumab, to unique patterns of renal injury.
The patient was managed with antihypertensive medication (amlodipine), diuretics for edema control, and statin therapy for lipid abnormalities. Cancer treatment was switched to pralatrexate and anlotinib. At follow-up in July 2024, his hypertension persisted, kidney function remained impaired, and proteinuria had worsened to nearly 8 g/day.
According to the authors, the case highlights several important clinical lessons:
While Bmab-GMA remains rare, its potential severity makes awareness crucial. As anti-VEGF therapies continue to be widely used in oncology, further research is needed to define their pathogenesis, risk factors, and optimal management strategies.
Reference:
Jiang, R., Yu, Rz., Yang, Hf. et al. Bevacizumab-associated glomerular microangiopathy: a case report and literature review. BMC Nephrol 26, 445 (2025). https://doi.org/10.1186/s12882-025-04385-9
Powered by WPeMatico

The FDA has approved oral brensocatib (Brinsupri) for adults and children 12+ with non-cystic fibrosis bronchiectasis. As a first-in-class reversible DPP-1 inhibitor, it targets the disease’s underlying inflammation, which can cause permanent lung damage and affects about 500,000 people in the U.S.
BRINSUPRI is the first and only FDA-approved treatment for NCFB, giving hundreds of thousands of patients and clinicians across the U.S. an option to manage this chronic and progressive disease that can lead to permanent lung damage and lung function decline.
“This FDA approval represents a potential paradigm shift in how we approach non-cystic fibrosis bronchiectasis,” said Doreen Addrizzo-Harris, M.D., FCCP, the Fiona and Stanley Druckenmiller Professor of Pulmonary, Critical Care and Sleep Medicine at NYU Grossman School of Medicine and Director of the NYU Langone Health Bronchiectasis and NTM Program, and ASPEN investigator. “For the first time, we have a treatment that directly targets neutrophilic inflammation and addresses a root cause of bronchiectasis exacerbations. Based on the strength of the data and the impact we’ve seen in patients, I believe this could become the new standard in non-cystic fibrosis bronchiectasis care.”
There are approximately 500,000 people in the U.S. diagnosed with NCFB, and it is estimated that millions more are living with this disease globally. Unlike other respiratory diseases that are characterized by airway narrowing, bronchiectasis causes airways to permanently widen, making it harder to clear mucus and bacteria, leading to persistent inflammation and infection. A hallmark of bronchiectasis is frequent exacerbations, or flares, when symptoms worsen, such as coughing, increased mucus, shortness of breath and fatigue.
“Non-cystic fibrosis bronchiectasis deeply affects the lives of people living with this chronic lung condition, impacting both their physical health and emotional well-being,” added Elisha Malanga, Executive Director of the Bronchiectasis and NTM Association. “Many patients experience frequent flares, which can disrupt daily life and potentially lead to disease progression. The FDA approval of brensocatib represents a significant and long-awaited advancement as the first approved therapy for non-cystic fibrosis bronchiectasis. Our hope is that treatments like this will enable people with bronchiectasis to manage their condition.”
This approval is based on data from the Phase 3 ASPEN and Phase 2 WILLOW studies, which were both published in the New England Journal of Medicine. In ASPEN, patients taking BRINSUPRI 10 mg or 25 mg had a 21.1% and 19.4% reduction in annual rate of exacerbations respectively, as compared to placebo. Both dosage strengths of BRINSUPRI also met several exacerbation-related secondary endpoints, including significantly prolonging the time to first exacerbation and significantly increasing the proportion of patients remaining exacerbation-free over the treatment period. Patients who received BRINSUPRI 25 mg experienced statistically significant less decline in lung function, as measured by forced expiratory volume in one second (FEV₁) after using a bronchodilator, at week 52. The safety of BRINSUPRI was also evaluated in both studies. The most common adverse reactions ≥2% in the ASPEN trial included upper respiratory tract infection, headache, rash, dry skin, hyperkeratosis, and hypertension. The safety profile for adult patients with NCFB in WILLOW was generally similar to ASPEN, except for a higher incidence of gingival and periodontal adverse reactions in WILLOW.
“The FDA approval of the first-ever treatment for non-cystic fibrosis bronchiectasis is a historic milestone for patients and for Insmed,” said Martina Flammer, M.D., MBA, Chief Medical Officer of Insmed. “By keeping patients at the center of everything we do, we have once again delivered a first-in-class medicine for a disease with no prior approved treatments. This is an incredible achievement in medicine. We’re deeply grateful to the patients, providers, and advocates who made this possible – this is just the beginning of what we can accomplish together for this community.”
BRINSUPRI is a first-in-class dipeptidyl peptidase 1 (DPP1) inhibitor, designed to inhibit the activation of enzymes (neutrophil serine proteases) in neutrophils that are key drivers of chronic airway inflammation in NCFB. BRINSUPRI is the first approved therapy to address the underlying inflammatory process of NCFB.
In parallel, applications for brensocatib with the European Medicines Agency (EMA) and the Medicines and Healthcare products Regulatory Agency (MHRA) have been accepted, and the Company plans to file in Japan in 2025. Commercial launches are anticipated in 2026, pending approval in each territory.
BRINSUPRI is now available in the U.S. by prescription through a comprehensive specialty pharmacy network.
BRINSUPRI™ (brensocatib) is a small molecule, once-daily, oral, reversible inhibitor of dipeptidyl peptidase 1 (DPP1) indicated for the treatment of non-cystic fibrosis bronchiectasis (NCFB) in adult and pediatric patients 12 years of age or older. Brensocatib is designed to inhibit the activation of enzymes (neutrophil serine proteases) in neutrophils that are key drivers of chronic airway inflammation in NCFB. Brensocatib is also being evaluated for its potential role in other neutrophil-mediated diseases.
Powered by WPeMatico

An autopsy study published in the Journal of American Medical Association revealed that higher adherence to the Mediterranean–Dietary Approaches to Stop Hypertension Intervention for Neurodegenerative Delay (MIND) diet was associated with lower odds of hippocampal sclerosis and less dementia at death, suggesting the diet’s protective effect may be partly mediated through reduced hippocampal damage.
Severe neuronal loss and astrogliosis in coronal sections of the mid-hippocampus cornu ammonis 1 or subiculum is known as hippocampal sclerosis (HS). This pathology is linked to dementia, Alzheimer’s disease, and limbic-predominant age-related transactive response DNA-binding protein 43 encephalopathy neuropathological change (LATE-NC). In humans, nothing is known about the relationship between food and HS or HS and LATE-NC. Thus, this study examined the relationship between HS and HS with LATE-NC and the MIND diet.
Autopsied patients from the ongoing Rush Memory and Aging Project cohort research were included in this investigation. Researchers included participants with neuropathological and nutritional data from 2004 to 2024. Analysis of the data was place between April 3, 2024, and May 13, 2025. The average MIND diet scores were calculated using all verified food frequency questionnaires that were given every year for up to 18 years before to death.
Hematoxylin and eosin staining was used to determine the presence of HS, while TDP-43 immunohistochemistry was used to identify the presence of LATE-NC in eight different brain areas. A semiquantitative measure was used to evaluate the degree of hippocampus neuronal loss in a group of 300 patients. The scale ranged from 0, which indicates no neuronal loss, to 5, which is classified as none to mild, moderate, and severe neuronal loss.
Of the 809 participants (mean [SD] age at death, 91.3 [6.1] years; mean [SD] follow-up, 7.2 [4.4] years; 538 [72%] female; mean [SD] follow-up, 7.2 [4.4] years), 82 (10.1%) had HS; 71 (9%) had both HS and LATE-NC; and in the scored subset, 35 (12%) and 43 (14%) had severe hippocampus neuronal loss.
After adjusting for age at death, sex, education, total calories, APOE-ε4 status, AD, and vascular pathologies, higher MIND diet scores were linked to decreased risks of HS (odds ratio [OR], 0.78; 95% CI, 0.65 to 0.95) and HS with LATE-NC (OR, 0.79; 95% CI, 0.64 to 0.97).
The MIND diet was linked to a 21% indirect connection through HS (β = -0.05; 95% CI, -0.10 to -0.01; P =.02) and a lower incidence of dementia at the time of death (β = -0.26; 95% CI, -0.36 to -0.15; P <.001) in mediation analyses. Less hippocampus neuronal loss was linked to a higher MIND diet score (P for trend =.01).
Overall, MIND diet adherence throughout follow-up was linked to a decreased risk of HS, HS with LATE-NC, and hippocampus neuronal loss in this cohort analysis of autopsied subjects. According to these results, the MIND diet may lessen negative effects on brain health.
Reference:
Agarwal, P., Agrawal, S., Wagner, M., Cherian, L. J., Aggarwal, N. T., James, B. D., Holland, T. M., Bennett, D. A., Barnes, L. L., Leurgans, S. E., & Schneider, J. A. (2025). MIND diet and hippocampal sclerosis among community-based older adults. JAMA Network Open, 8(8), e2526089. https://doi.org/10.1001/jamanetworkopen.2025.26089
Powered by WPeMatico
