New Delhi: The State Consumer Disputes Redressal Commission, Delhi recently held the All India Institute of Medical Sciences (AIIMS) guilty of medical negligence while providing In Vitro Fertilization (IVF) treatment to a patient.
Despite undergoing the IVF procedure twice, the complainant could not conceive. She alleged that the treating doctors at the hospital failed to prescribe the necessary Thyroid test before undergoing the procedure.
AIIMS has been directed by the Commission to pay Rs 2.5 lakh compensation (including the cost of treatment spent for IVF) to the Complainant for the suffering, mental pain and agony caused.
The Commission opined that there was sheer negligence on the part of the hospital as the patient was not treated with due care and caution by the hospital and the treatment was not done in accordance with the medical practice followed by the doctors while treating the patient of similar condition and age.
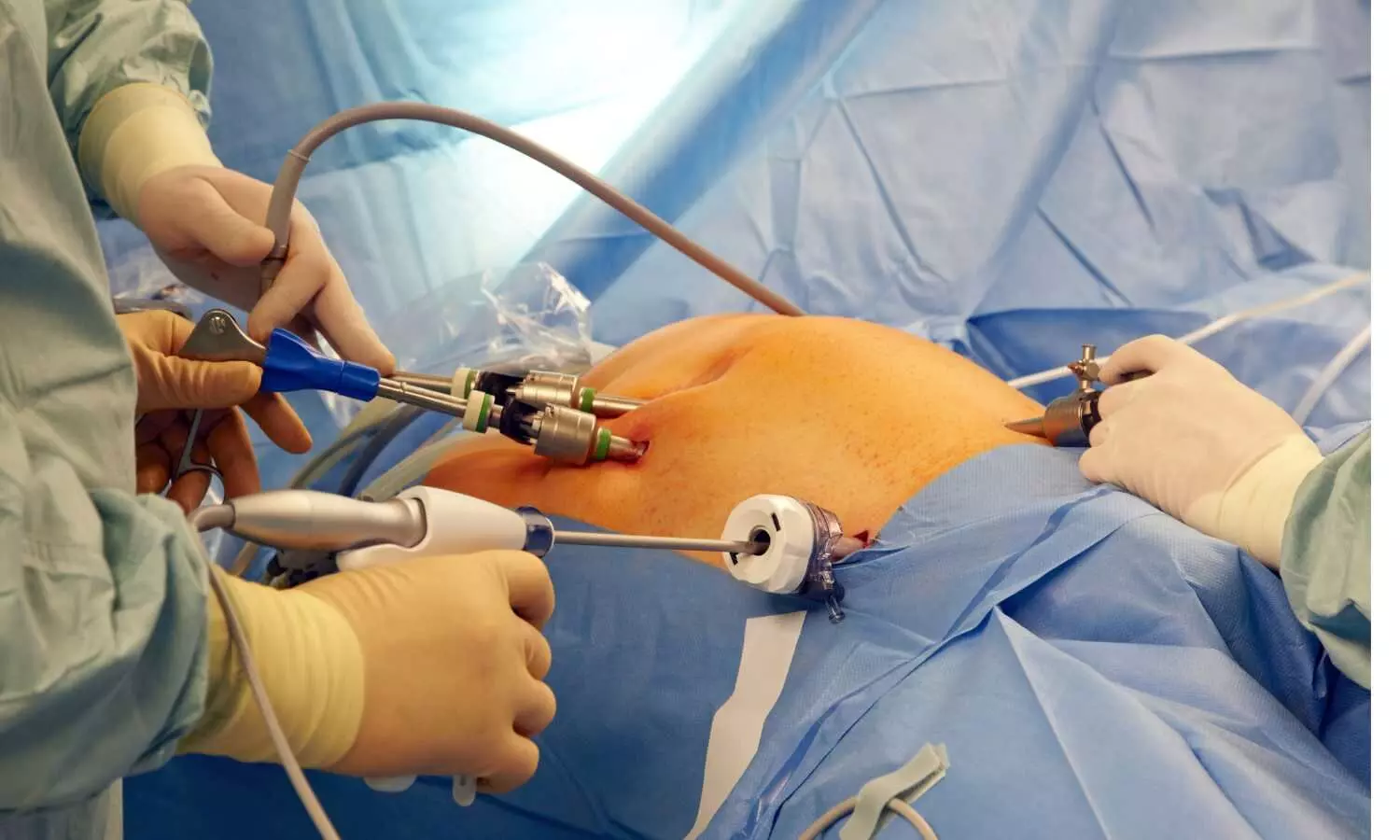
The matter goes back to 2008 when the complainant approached AIIMS hospital to undergo the necessary treatment to overcome infertility and to have a child. After the preliminary tests and examinations under the guidance of the HOD Gynae, the complainant was advised to opt for In Vitro Fertilization (IVF) and accordingly, she got admitted to the hospital on 07.01.2008 and a team of doctors was engaged to start laparoscopy and a mandatory process before the IVF i.e. Mock ET on 26.03.2008. Consequently, the IVF process was conducted by the operating doctor on 01.12.2008.
Following this, the patient was discharged on the same day after charging an amount of Rs 60,000 for the said process. However, allegedly, the Thyroid-test, which is necessary in cases of fertility was not done or advised by the operating doctor before commencement of the treatment.
The second plan for IVF was adopted beginning on 20.05.2010 with the help of frozen embryo. However, the doctors failed to advise the Thyroid Test before undergoing the method adopted and therefore, no positive result came out from the second IVF process, alleged the complainant.
Thereafter, the third IVF process was proposed to be carried out on 21.04.2011. However, as the patient was putting on weight, she decided to go for the Thyroid Test through a pathology, from where she got to know that she was suffering from thyroid and therefore she consulted Dr. Ganpati, a specialist, who prescribed some medicines for the treatment of thyroid.
Once again the complainant approached AIIMS, where the operating doctor advised the Thyroid test and based on the report dated 27.06.2011. However, no such test was prescribed by them prior to such date, alleged the complainant. Losing all her faith in the hospital, the complainant deferred to go for the third IVF process.
It was alleged by the complainant that when she was admitted to AIIMS, the operating doctor should have, at the first instance, advised for the Thyroid-Test since it is crucial to know about the success rate of the IVF and the process should run accordingly. She alleged that there was clear negligence on the part of the hospital as the operating doctors also failed to conduct the required test during the second phase of IVF.
In her complaint, she pointed out that the success rate in the case of IVF is 25 to 30%. However, in the case when the patient is suffering from Thyroid, the success rate falls to 15%. However, no efforts were made by the hospital to advice for the Thyroid Test, alleged the complainant.
Therefore, on these grounds mentioned above, the complainant alleged utter Medical Negligence on the part of the hospital and approached the State Consumer Court, Delhi.
While considering the matter, the consumer court heard the complainant’s counsel and also perused the material available on record including the written arguments filed on behalf of the complainant and the hospital. In order to discuss in detail the scope and extent of Negligence with respect of Medical Professionals, the consumer court referred to the order in the case of Seema Garg & Anr. vs. Superintendent, Ram Manohar Lohia Hospital & Anr. decided on 31.01.2022.
In the concerned judgment, it was mentioned that in cases where the allegations are levelled against the Medical Professionals, negligence is an essential ingredient for the offence, which is basically the breach of a duty exercised by omission to do something which a reasonable man would do or would abstain from doing. However, negligence cannot be attributed to a doctor so long as he performs his duties with reasonable skill and competence and they are entitled to protection so long as they follow the same.
Referring to this order, the consumer court noted,
“In the present case also, it will have to be ascertained whether there was any lack of skill and competence on the part of the operating doctor and/or any omission to do what was actually required in the present facts and circumstances.”
The Commission observed that the complainant did not allege that the operating doctors did not have the requisite skill or competence or they were not qualified to operate on the complainant. The main complaint was that the treating doctors at AIIMS failed to do the thyroid test before doing the IVF procedure, noted the Commission.
At this outset, the Commission perused the discharge summary and noted,
“Therefore, in order to check whether there was an deficiency on the part of treating doctor, we have carefully perused the medical records filed by the Complainant and found that the treating doctor have prescribed certain tests before doing the first process of IVF and they were done before doing IVF, however, no Thyroid-test was done and prescribed by the treating doctors which can be clearly seen from the discharge summary available before us…”
Additionally, the consumer court found that the treating doctors while mentioning the history of patient have mentioned about the Thyroid-Test which was undertaken by the Complainant in the year 2004 and mentioned the readings as: T3-119.0, T4 – 6.54 and TSH – 4.38 which was normal.
Besides, the Commission also took note of the fact that the “…Thyroid function may indeed affect the process and success of in vitro fertilization (IVF) as the thyroid gland plays a crucial role in regulating metabolism and hormone production, and thyroid disorders can impact fertility in the patient. Additionally, Thyroid hormones, specifically thyroxine (T4) and triiodothyronine (T3), plays a role in regulating the menstrual cycle and ovulation. An underactive thyroid (hypothyroidism) or an overactive thyroid (hyperthyroidism) can disrupt the normal hormonal balance required for ovulation and the preparation of the uterine lining for embryo implantation and due to these reasons, it is important for individuals undergoing IVF to have their thyroid function evaluated and, if necessary, treated or managed before and during the IVF process. Further, if a thyroid disorder is diagnosed, appropriate treatment or medication may be recommended to bring thyroid function into the normal range.”
However, the Commission observed that the treating doctors have failed to diagnose the Thyroid function at the primary stage and it came to the knowledge of the treating doctor in the year 2011, when the Complainant opted to get herself checked for the Thyroid test. “Additionally, considering the age of the Complainant in the present case, it was clear to the treating doctor that the chances of getting the IVF successful in the present case is very low,” noted the Commission.
“Moreover, it is a well laid down principle that the doctor diagnosing upon a patient is the best judge of the treatment which is to be undertaken for that specific patient. There may be multiple approaches with which the patient may be treated upon, however, the doctor is expected to choose the most appropriate one in the given facts and circumstances. Hence, a higher degree of reliance is placed upon the concerned doctor, that whatever option he/she exercises will be for the benefit and interest of the patient. However, failure on the part of doctor in diagnosing the Thyroid function at the primitive stage has mentally and physically harassed the Complainant and her family,” it further added.
Finally, relying upon the Supreme Court order in the case of Jacob Mathew v. State of Punjab and Anr, Martin F. D’Souza v. Mohd. Ishfaq, and Kusum Sharma and Ors. (supra), the Commission opined that the approach in medical negligence cases should be “what was actually done by the doctor was not acceptable or generally used in the medical practices at the given point of time.”
Taking all these factors into account, the Commission opined that there was sheer negligence on the part of the hospital i.e. AIIMS
“as the patient (Complainant) was not treated with due care and caution by the Opposite Party no. 1 and the treatment was not done in accordance with the medical practice followed by the doctors while treating the patient of similar condition and age.”
Therefore, holding AIIMS negligent in providing its services to the Complainant and keeping in view the principles detailed above and the facts and circumstances of the case, the age of the patient, and other necessary and essential factors, the Commission opined it to be just and reasonable to award compensation of Rs. 2,50,000 (including the cost of treatment spent by the Complainant for IVF) to the Complainant for the suffering, mental pain and agony caused.
“The amount so awarded … be paid by the Opposite Party no. 1 being liable, within a period of three months from the date of present judgment i.e. on or before 29.02.2024, failing which, the Opposite Party no. 1 would be liable to pay the said amount alongwith the interest at the rate of 9% p.a. from 01.12.2008 (when the Complainant has undergone for the first IVF process) till the actual realization of said amount,” the Commission mentioned in its order.
To view the order, click on the link below:
https://medicaldialogues.in/pdf_upload/aiims-negligence-229143.pdf
Also Read: Treatment of patient based on telephonic advice from doctor constitutes negligence, opines NCDRC