Can transcranial magnetic stimulation damage or interact with implanted cardiac devices?
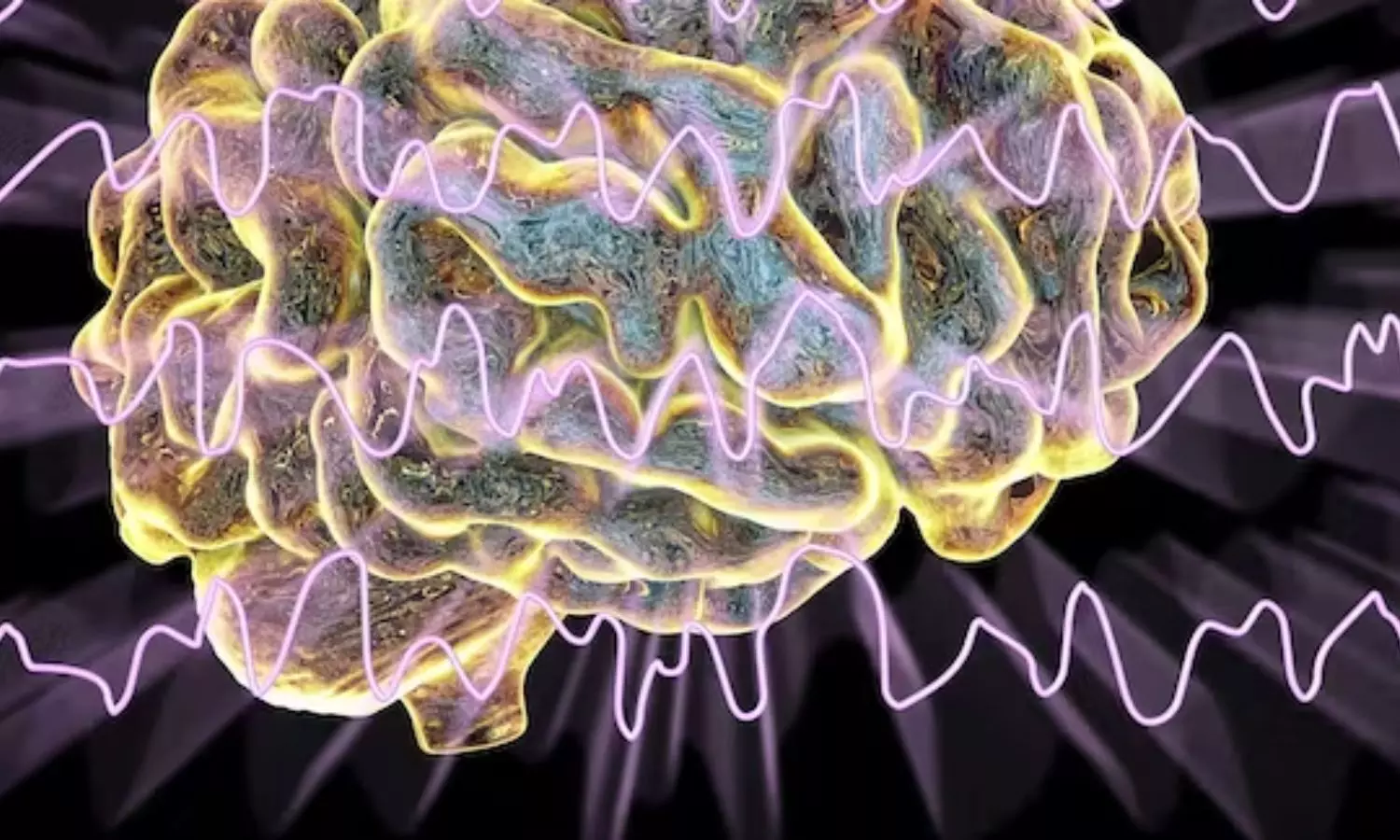
Germany: A recent study showed a low risk of implantable cardioverter-defibrillator (ICD) damage or overheating during transcranial magnetic stimulation (TMS), used for treating several neuropsychiatric disorders, even when stimulation was much stronger than normal. The findings were published online in JACC: Clinical Electrophysiology on January 3, 2024.
Multiple experiments indicated that electromagnetic therapy for depression shouldn’t damage a person’s pre-existing implantable cardioverter-defibrillator.
Felix Wegner, MD, of University Hospital Muenster, Germany, and colleagues had several Biotronik ICDs hooked up to an arrhythmia simulator and exposed ex vivo to magnetic stimulation, using MagStim equipment, with an increasing gradient during continuous device telemetry:
- Biotronik Intica Neo 7 DR-T ICD programmed to the device’s MRI mode and asynchronous pacing (DOO 80/min): No interaction between magnetic stimulation and the device even at the maximum output. There were no significant changes in sensing amplitude, lead impedance, or thresholds.
- Biotronik Intica Neo 7 DR-T ICD programmed to a dual-chamber mode: Atrial oversensing occurred at an output of 25% of maximum, leading to a pacemaker tachycardia which was correctly identified and terminated by the device. No significant changes in sensing amplitude, lead impedance, or thresholds were observed.
- Biotronik Itrevia 7 VR-T Dx ICD programmed in a single-chamber mode: No signal interference detected up to an output of 50% of maximum. At the maximum possible output, intermittent ventricular oversensing of the stimulation impulse occurred. No significant changes in sensing amplitude, lead impedance, or thresholds were observed.
A last experiment revealed that a Biotronik Rivacor 5 VR-T Dx ICD, connected to a Medtronic Sprint Quattro Secure MRI SureScan 6947M dual-coil defibrillator lead and immersed in saline solution, stayed undamaged when it was programmed to a single-chamber mode and exposed to magnetic stimulation at an output of 70% of maximum and a repetition rate of 0.9 Hz for 15 minutes. Also, there was no change in the temperature of the saline bath.
“Our proof-of-principle experiments suggest that the risk of damage to an ICD and heating of an ICD may be low during magnetic stimulation, even when stimulation is delivered directly to the device,” the researchers wrote.
“We consistently used a far greater output at a far closer distance to the ICD than would be realistic for TMS/TCMS [transcutaneous magnetic stimulation].”
They suggested that in light of the high comorbidity of depression in cardiovascular disease and its distinct effect on outcomes and prognosis, this might add therapeutic options for a significant proportion of cardiac patients.
“Our data could encourage investigators using TMS/TCMS to include device patients in future studies after careful individual risk/benefit analysis,” they concluded.
They added that “Because only Biotronik ICD and Medtronic defibrillator leads were studied, research on pacemakers, ICD, and magnetic stimulation coils and generators of all types and manufacturers in more physiologic models of magnetic device interference is warranted.”
Reference:
Wegner, F. K., Bietenbeck, M., Suntrup-Krueger, S., Markman, T. M., Eckardt, L., & Wolters, C. (2024). Transcranial/Transcutaneous Magnetic Stimulation Interacts With But Does Not Damage Implantable Cardioverter-Defibrillators. JACC: Clinical Electrophysiology. https://doi.org/10.1016/j.jacep.2023.10.021
Powered by WPeMatico