Breakthrough Treatment Offers Hope for Electrical Storm Patients
In
a groundbreaking effort to address the clinical emergency posed by electrical
storms (ES) and the scarcity of effective treatments, researchers have unveiled
compelling findings from the STAR study, a multicenter observational
investigation. The study focused on the potential efficacy and safety of
percutaneous stellate ganglion block (PSGB) as a novel intervention for ES,
refractory to standard treatments. The results, spanning the period from July
1, 2017, to June 30, 2023, present a ray of hope for patients grappling with
this challenging condition.
The
study results were published in the European Heart Journal.
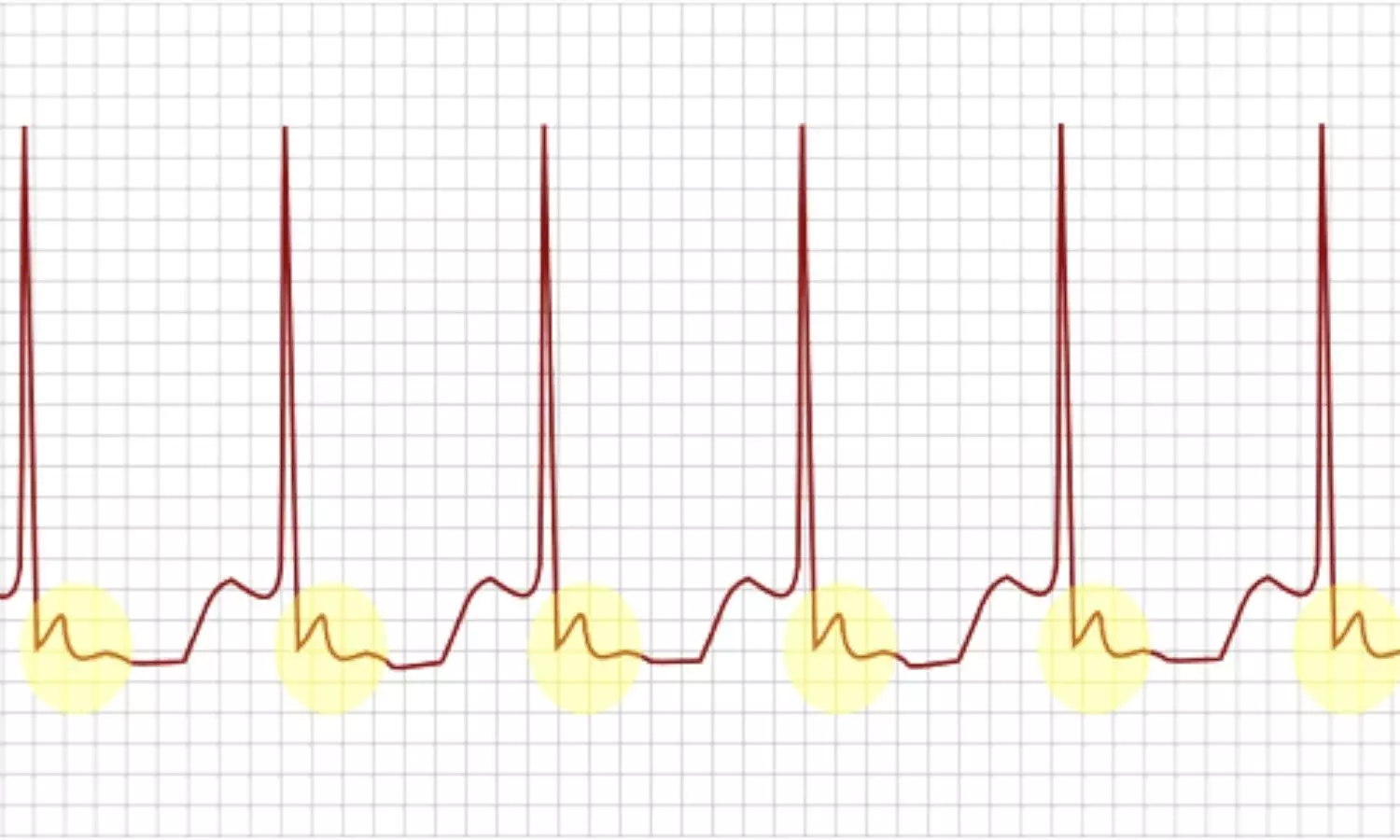
Electrical
storms, characterized by three or
more episodes of ventricular arrhythmias or ventricular fibrillation (VF),
represent a critical clinical scenario with limited established therapeutic
options. Initial reports on PSGB hinted at its safety and effectiveness, but
questions lingered, prompting the need for a comprehensive study. The STAR
study aimed to fill this void, shedding light on the potential of PSGB as a
viable intervention for ES.
Conducted
as a multicenter observational study, STAR enrolled 131 patients from 19
centers, all experiencing ES refractory to standard treatments. The primary
focus was on assessing the reduction of treated arrhythmic events by at least
50%, comparing the 12 hours following PSGB with the 12 hours preceding the
procedure. Operators underwent specialized training for both the anterior
anatomical and lateral ultrasound-guided approaches.
Key
Findings:
- The results of the STAR study are nothing short of promising.
- Among the 184 PSGB procedures conducted, 92% of patients achieved the primary outcome, showcasing a significant reduction in arrhythmic events.
- The median reduction of arrhythmic episodes between 12 hours before and after PSGB was an impressive 100%, underscoring the potential efficacy of this intervention.
- Importantly, arrhythmic episodes requiring treatment exhibited a noteworthy decline, with a statistically significant difference observed between the 12 hours before the first PSGB and the 12 hours after the last procedure.
- The reduction continued when comparing 1 hour before and 1 hour after each procedure, emphasizing the sustained impact of PSGB.
- Moreover, the study reported a low incidence rate of one major complication, emphasizing the safety profile of the intervention.
The
STAR study marks a significant stride in the pursuit of effective treatments
for electrical storms. The compelling evidence supporting the effectiveness and
safety of PSGB in treating refractory ES offers newfound hope for patients and
clinicians alike. These findings pave the way for further exploration and
potential incorporation of PSGB into the standard armamentarium for managing
this complex clinical emergency.
Further reading: Savastano S, Baldi E, Compagnoni S, et al. Electrical storm treatment by percutaneous stellate ganglion block: the STAR study. Eur Heart J. Published online January 30, 2024. doi:10.1093/eurheartj/ehae021
Powered by WPeMatico