A course of acupuncture may curb the heightened risk of stroke associated with rheumatoid arthritis, finds a comparative study published in the open access journal BMJ Open.
The effects seem to be independent of sex, age, medication use, and co-existing conditions, the findings indicate, prompting the researchers to suggest that the procedure may reduce levels of pro-inflammatory proteins (cytokines) in the body that are linked to cardiovascular disease.
The principal cause of death in people with rheumatoid arthritis is cardiovascular disease. And they are more likely to have a stroke than the general population, note the researchers.
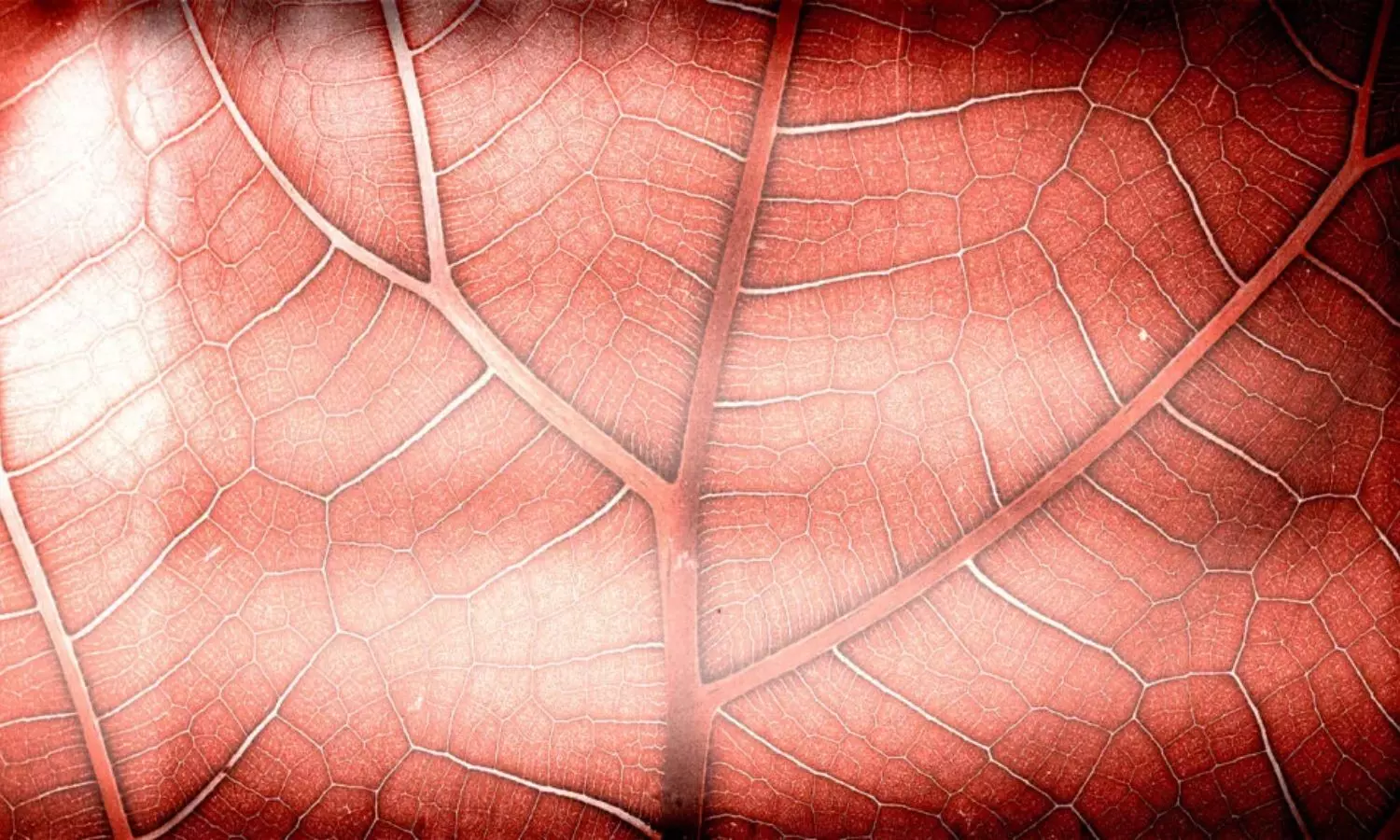
Acupuncture is already used to control pain and dampen down inflammation, and the researchers wanted to find out if it might also lower the risk of ischaemic stroke–caused by a blood clot in the brain-that is associated with systemic inflammation.
They drew on national medical records from the Registry for Catastrophic Illness Patients Database (RCIPD), for 47,809 adults newly diagnosed with rheumatoid arthritis between 1997 and 2010.
The final analysis included 23,226 patients with complete data, 12,266 of whom were treated with acupuncture following their diagnosis up until the end of December 2010.
Of these, 11,613 were each matched for age, sex, co-existing conditions-diabetes, high blood pressure, high blood fats, congestive heart failure, anxiety/depression, obesity, atrial fibrillation, alcohol dependency, and smoking-medication use-non-steroidal anti-inflammatory drugs, statins, and disease modifying drugs-and year of diagnosis with a patient who hadn’t been treated with acupuncture.
Women, those aged 40–59, and participants with high blood pressure predominated in both groups.
Most (87%) of those in the acupuncture group were treated with manual acupuncture (87%); 3% were treated with electroacupuncture, whereby an electrode producing a low pulse of electricity is attached to the needle; and 10% received both types.
On average, 1065 days elapsed between a rheumatoid arthritis diagnosis and receipt of the first acupuncture treatment, with the number of treatments averaging around 10 in total.
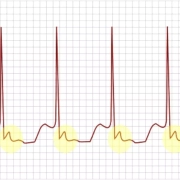
During the monitoring period up to the end of 2011, 946 patients had an ischaemic stroke. Unsurprisingly, risk rose in tandem with increasing age, and with the number of co-existing conditions.
Those with high blood pressure, for example, were more than twice as likely to have a stroke as those with normal blood pressure, while those with diabetes were 58% more likely to do so.
But there were significantly fewer cases of ischaemic stroke among the acupuncture group: 341 vs 605, equivalent to a 43% lower risk. And this was independent of age, sex, medication use, and co-existing conditions.
This is an observational study, and as such, no firm conclusions can be drawn about cause and effect, and the researchers also acknowledge that they were only able to estimate disease severity from the drugs the patients took.
Nor did they have information on potentially influential factors, such as height, weight, lab tests or physical activity levels, and not everyone would have had the same pressure points needled, they add.
But they point out: “Inflammation is a consistent and independent predictor of cardiovascular disease in [rheumatoid arthritis],” so acupuncture may lower pro-inflammatory proteins, thereby reducing the risk of cardiovascular disease, including ischaemic stroke, they suggest.
“Unstable blood pressure and lipid profiles are the two risk factors for ischaemic stroke, and acupuncture therapy has the advantage of controlling both hypertension and dyslipidaemia,” they explain, adding: “If acupuncture relieves morning stiffness and joint pain, patients might also benefit from increasing daily activities, which might also reduce the risk of stroke.”
Reference:
http://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2023-075218