Doctors found to be quitting over stress and cost of finding suitable childcare
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico

Home insulin pump use is safe for hospitalised children with diabetes without active ketoacidosis suggests a new study published in the JAMA Netw Open.
Pediatric data on inpatient home insulin pumps are absent in the literature. Understanding safety of home insulin pumps, managed by patients or caregivers, during times of illness will help diabetes technology securely move into pediatric hospitals. A study was done to examine whether insulin can be safely and accurately delivered to hospitalized children through home insulin pumps when managed by patients or caregivers. This single-center, retrospective, observational cohort study included children with insulin-dependent diabetes admitted to a tertiary children’s hospital from January 1, 2016, to December 31, 2021. In all these patients, diabetes was the primary or secondary diagnosis on admission. Hyperglycemia (glucose, >250 mg/dL) and hypoglycemia (glucose, <45 mg/dL) rates (quantified as the proportion of total insulin-days), glucose variability, and diabetic ketoacidosis (DKA) recurrences were compared for hospital pumps (manual mode), home pumps (manual mode), and subcutaneous injections using bivariate tests. Results There were 18 096 insulin-days among 2738 patients aged 0.5 to 25 years (median age, 15.8 years [IQR, 12.3-18.3 years]). Overall, 990 (5.5%) of insulin-days involved hospital insulin pumps, and 775 (4.3%) involved home pumps. A total of 155 insulin-days (15.7%) involving hospital pumps were hyperglycemic, compared with 209 (27.0%) involving home pumps and 7374 (45.2%) involving injections (P < .001). Moderate hypoglycemia days comprised 31 insulin-days (3.1%) involving hospital pumps compared with 35 (4.5%) involving home pumps and 830 (5.1%) involving injections (P = .02). Severe hypoglycemia did not differ significantly according to insulin delivery method. Two patients using injections (0.01%) developed DKA; no patients using hospital or home pumps developed DKA. In this cohort study, home insulin pump use was found to be safe in a children’s hospital regarding hyperglycemia and hypoglycemia. These data support use of home insulin pumps during pediatric admissions in patients who do not require intensive care and without active DKA.
Reference:
Owens J, Courter J, Schuler CL, Lawrence M, Hornung L, Lawson S. Home Insulin Pump Use in Hospitalized Children With Type 1 Diabetes. JAMA Netw Open. 2024;7(2):e2354595. doi:10.1001/jamanetworkopen.2023.54595
Keywords:
Home insulin pump, hospitalised children, diabetes, active ketoacidosis, Owens J, Courter J, Schuler CL, Lawrence M, Hornung L, Lawson S, JAMA Netw Open
Powered by WPeMatico
Taiwan: A recent study revealed an increased odds of coronary artery calcification (CAC) with abdominal obesity (AO) and association of AO with a 4.4-fold increased risk of severe CAC in patients with chronic kidney disease (CKD). The findings were published online in Dove Press International Journal of Nephrology and Renovascular Disease.
In the large population-based study, the researchers observed close associations between CKD and abdominal obesity with increased risks of both positive CAC and severe CAC.
“Participants with CKD exhibited adjusted odds ratios (ORs) of 1.1 and 2.6 for positive CAC and severe CAC, respectively, and the participants with AO had adjusted ORs of 1.4 and 1.8 for positive CAC and severe CAC, respectively,” the researchers reported.
“The combined effects of CKD and AO resulted in increased ORs of 2.4 and 4.4 for positive CAC and severe CAC, respectively.”
An elevated CAC score indicates the increased presence of fibro-calcified lesions in the coronary arteries, resulting in increased vessel wall stiffness. Accordingly, the CAC score is regarded as a robust predictive marker of coronary artery disease (CAD) risk.
Cardiovascular disease is the main cause of mortality in CKD patients, with the risk exacerbated by metabolic disorders. Compared with body mass index (BMI), waist circumference (WC) has been suggested as a more effective indicator of abnormal visceral fat. However, the associations between CKD, abnormal WC, and cardiovascular disease (CVD) have not been studied well.
Although both CKD and abdominal obesity independently raise CAD incidence, the combined effects of CKD and AO on CAC remain uncertain. CKD. Accordingly, Peng-Tzu Liu and Jong-Dar Chen from the Department of Family Medicine, Shin Kong Wu Ho-Su Memorial Hospital, Taipei City, Taiwan, elucidated this association and highlighted the importance of waist circumference as a clinical parameter for assessing patients with pre-dialysis
For this purpose, they conducted a cross-sectional study in Taiwan from 2006 to 2016 comprising 10,342 participants undergoing self-paid health checkups at a single medical centre. Blood samples and physical examinations were taken to assess metabolic parameters, and the Chronic Kidney Disease Epidemiology Collaboration formula was used for evaluating renal function.
Coronary artery calcification scores were determined through coronary 256-slice multidetector computed tomography angiography, with a CAC score of >0 Agatston unit (AU) and ≥ 400 AU denoting positive CAC and severe CAC, respectively.
Sex-based comparisons were conducted between individuals with chronic kidney disease and those without CKD.
The study revealed the following findings:
To conclude, the study provides evidence for the combined effects of chronic kidney disease and abdominal obesity on CAC. The participants with both CKD and AO exhibited 2.4- and 4.4-fold increased risks of positive CAC and severe CAC, respectively.
“Accordingly, in clinical practice, increased attention should be paid to reduce AO for individuals with CKD,” the researchers wrote.
Reference:
Liu PT, Chen JD. The Associations Between Abdominal Obesity and Coronary Artery Calcification in Chronic Kidney Disease Population. Int J Nephrol Renovasc Dis. 2024 Feb 1;17:39-45. doi: 10.2147/IJNRD.S446445. PMID: 38317662; PMCID: PMC10840527.
Powered by WPeMatico
Nighttime acid reflux commonly referred to as nocturnal acid breakthrough (NAB) is defined as a persistent decrease in intragastric pH below 4 for more than 60 minutes at night. (1) It has clinical sequels, particularly in patients with complicated gastroesophageal reflux disease (GERD), Barrett’s esophagus, and esophageal motility abnormalities. (2) Nocturnal acid breakthrough (NAB) occurs in 40% to 70% of patients with GERD who are being treated with proton pump inhibitors (PPIs), (1) and more than 70% of Helicobacter pylori-negative patients on PPI therapy. (2)
Clinical Relevance of Nocturnal Acid Breakthrough
Most individuals are recumbent during nighttime and do not swallow as frequently as during daytime. Without the assistance of gravity and with decreased salivary buffering, esophageal acid clearance depends primarily on esophageal peristalsis. Therefore, a nocturnal acid breakthrough is particularly relevant in patients with complicated GERD, Barrett’s esophagus, and esophageal motility abnormalities. (2)
Interestingly, clinical studies have indicated that nocturnal acid breakthrough is an isolated gastric phenomenon and esophageal acid suppression, and symptom control are not dependent on the degree of nocturnal acid breakthrough elimination. Nocturnal acid breakthrough increases the likelihood of reflux during the gastric acid breakthrough in patients with decreased lower esophageal sphincter pressure and ineffective esophageal motility, i.e. high frequency of distal esophageal body contractions <30 mmHg. (2)
Approach to Management of Nocturnal Acid Breakthrough
The maximal benefit from PPI therapy is achieved when PPIs are taken 15–30 minutes before meals, allowing optimal blood concentrations of the drug during meal-induced activation of proton pumps to produce blockade of many pumps. Researchers have also focused on eliminating NAB by targeting the histamine surge during nighttime using histamine H2 receptor antagonists (H2RA) such as ranitidine. (1) Normally, there is no food ingestion during nighttime, so bedtime dosing of H2RAs benefits inhibiting nocturnal acid secretion. Adding bedtime H2RAs is clinically effective in controlling nocturnal acid breakthrough and GERD symptoms. (2)
Bedtime ranitidine more effective than bedtime proton pump inhibitor (PPI): A double-blind, placebo-controlled, crossover study compared the effect of overnight intragastric pH of 20 mg omeprazole twice daily plus 20 mg at bedtime with those of 20 mg omeprazole twice daily plus 150 or 300 mg ranitidine or placebo at bedtime. The study included 12 subjects with an intragastric pH <4 for 48% of them (IQR, 35%–63%) of the overnight period with omeprazole, 20 mg twice daily, plus placebo at bedtime. A third dose of omeprazole at bedtime decreased this percentage to 31% (7%–36%; P<0.005). The result further showed that bedtime ranitidine significantly reduced the percentage of time with intragastric pH <4 by 5% with 150 mg and 6% with 300 mg (P <0.01 vs. omeprazole twice daily plus bedtime). These were significantly lower than those with placebo (p<0.001) or additional omeprazole at bedtime (p<0.01). This concludes that bedtime ranitidine is more effective than bedtime proton pump inhibitors in reducing NAB. (3)
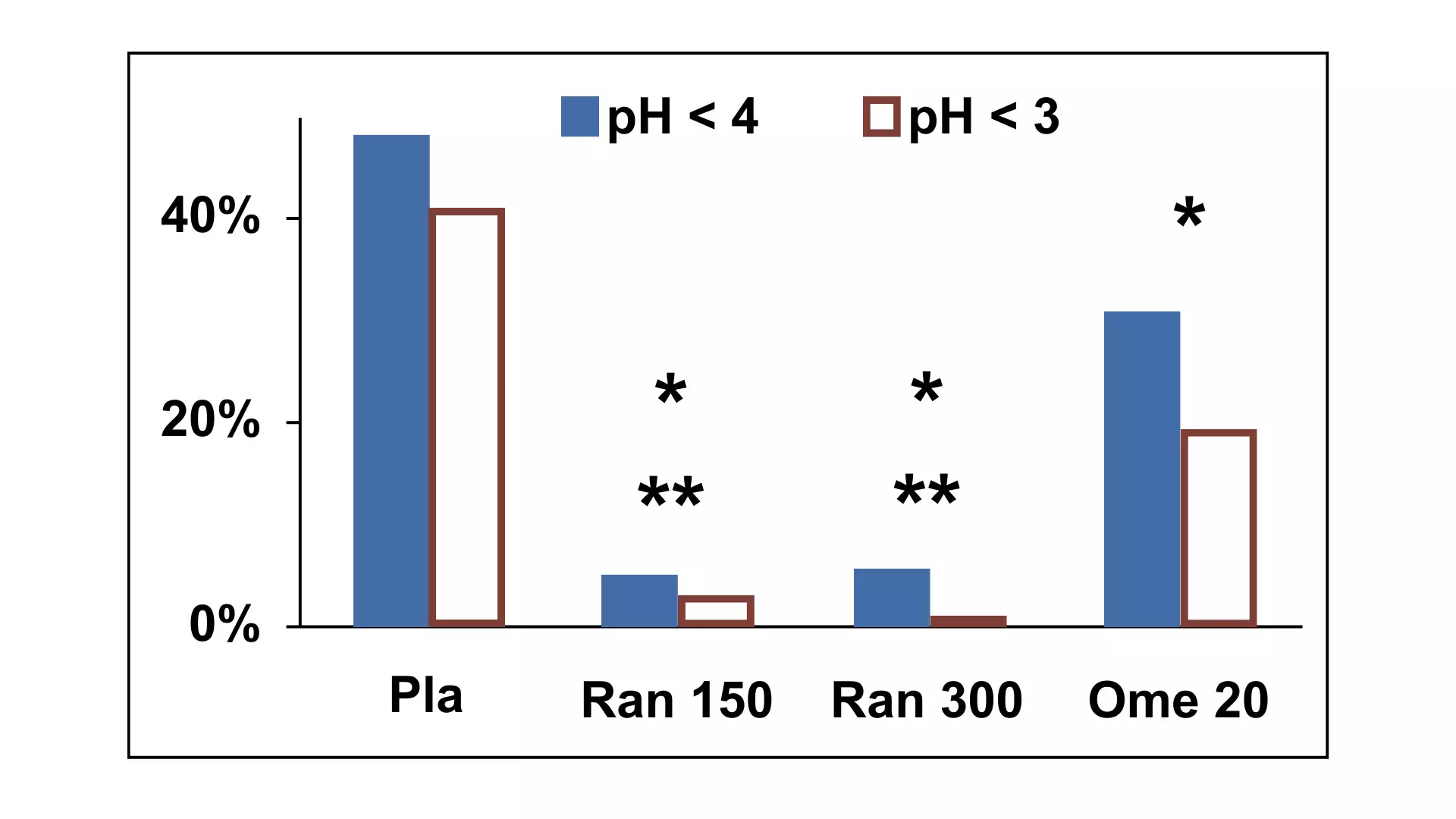
Figure: Median percentage of time with intragastric pH <4 and <3 from intake of the study medication at 10:30 PM until the end of the study at 6:30 AM. Adapted from Peghini, P L et al. “Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects.” Gastroenterology vol. 115,6 (1998): 1335-9.
The 4 treatments were placebo (Pla), 150 mg ranitidine (Ran 150), 300 mg ranitidine (Ran 300), and 20 mg omeprazole (Ome 20) in addition to 20 mg omeprazole twice daily. *P < 0.005 vs. placebo, **P < 0.01 vs. omeprazole 20 for both pH 4 and pH 3.
Combination of H2RAs and PPI Effective in NAB: Given the role of histamine in the nocturnal acid breakthrough mechanism, combining ranitidine at bedtime with daily PPI therapy is another effective approach to reducing nocturnal acid breakthrough. (4)
Review of Guideline Recommendations:
Indian Guideline: The Consensus Guidelines for Management of Gastroesophageal Reflux Disease by the Indian Society of Gastroenterology (ISG) and Association of Physicians of India (API) recommended adding bedtime H2RA in patients having nocturnal reflux symptoms despite the use of PPI. (Level of evidence: II-3 Grade of recommendation C) The consensus noted that adding bedtime H2RA (alone or in combination with PPI) to double dose PPI in patients with GERD decreases gastric acidity and NAB. (7)
Global Guidelines: The Seoul Consensus on the Diagnosis and Management of Gastroesophageal Reflux Disease also suggested adding the administration of H2RAs at bedtime to prevent NAB. It further noted the potential preventive role of H2RAs on nocturnal histamine-driven gastric acid secretion, supporting H2RAs as an option for patients with incomplete control of nighttime symptoms despite optimal PPI use. (8)
The Evidence-based Clinical Practice Guidelines for GERD by the Japanese Society of Gastroenterology suggested the addition of an H2RA before bedtime with a PPI to reduce NAB. (9)
Similarly, “A Management Update on the Refractory Gastroesophageal Reflux Disease” also suggested adding H2RAs at bedtime is considered to reduce and control NAB better and effectively. (10)
Key Points
References:
1. Jeon HK, Kim GH. Can Nocturnal Acid-breakthrough Be Reduced by Long-acting Proton Pump Inhibitors? J Neurogastroenterol Motil. 2017 Apr 30;23(2):145-148. doi: 10.5056/jnm17037.
2. Tutuian R, Castell DO. Nocturnal acid breakthrough – approach to management. MedGenMed. 2004 Oct 26;6(4):11.
3. Peghini PL, Katz PO, Castell DO. Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects. Gastroenterology. 1998 Dec;115(6):1335-9. doi: 10.1016/s0016-5085(98)70010-1.
4. Gerson LB, Fass R. A systematic review of the definitions, prevalence, and response to treatment of nocturnal gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2009 Apr;7(4):372-8; quiz 367. doi: 10.1016/j.cgh.2008.11.021. Epub 2008 Dec 3.
5. Mainie I, Tutuian R, Castell DO. Addition of a H2 receptor antagonist to PPI improves acid control and decreases nocturnal acid breakthrough. J Clin Gastroenterol. 2008 Jul;42(6):676-9. doi: 10.1097/MCG.0b013e31814a4e5c.
6. Xue, S., Katz, P. O., Banerjee, P., Tutuian, R., & Castell, D. O. (2001). Bedtime H2 blockers improve nocturnal gastric acid control in GERD patients on proton pump inhibitors: PROTON PUMP INHIBITORS PLUS H2RA IN GERD. Alimentary Pharmacology & Therapeutics, 15(9), 1351–1356.
7. Bhatia, Shobna et al. “API-ISG Consensus Guidelines for Management of Gastrooesophageal Reflux Disease.” The Journal of the Association of Physicians of India vol. 68,10 (2020): 69-80.
8. Jung HK, Tae CH, Song KH, Kang SJ, Park JK, Gong EJ, Shin JE, Lim HC, Lee SK, Jung DH, Choi YJ, Seo SI, Kim JS, Lee JM, Kim BJ, Kang SH, Park CH, Choi SC, Kwon JG, Park KS, Park MI, Lee TH, Kim SY, Cho YS, Lee HH, Jung KW, Kim DH, Moon HS, Miwa H, Chen CL, Gonlachanvit S, Ghoshal UC, Wu JCY, Siah KTH, Hou X, Oshima T, Choi MY, Lee KJ; Korean Society of Neurogastroenterology and Motility. 2020 Seoul Consensus on the Diagnosis and Management of Gastroesophageal Reflux Disease. J Neurogastroenterol Motil. 2021 Oct 30;27(4):453-481. doi: 10.5056/jnm21077.
9. Iwakiri K, Kinoshita Y, Habu Y, Oshima T, Manabe N, Fujiwara Y, Nagahara A, Kawamura O, Iwakiri R, Ozawa S, Ashida K, Ohara S, Kashiwagi H, Adachi K, Higuchi K, Miwa H, Fujimoto K, Kusano M, Hoshihara Y, Kawano T, Haruma K, Hongo M, Sugano K, Watanabe M, Shimosegawa T. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol. 2016 Aug;51(8):751-67. doi: 10.1007/s00535-016-1227-8. Epub 2016 Jun 21.
10. Rettura, Francesco et al. “Refractory Gastroesophageal Reflux Disease: A Management Update.” Frontiers in medicine vol. 8 765061. 1 Nov. 2021, doi:10.3389/fmed.2021.765061
Powered by WPeMatico
Uncontrolled blood sugar levels can damage blood vessels and organs, increasing the risk of heart disease, stroke, kidney failure, and other serious complications. Regular monitoring, lifestyle changes, and proper medical management are essential for maintaining optimal blood sugar levels and preventing the progression of diabetes-related complications.
While yoga offers various health benefits, claiming it as a sole cure for diabetes oversimplifies the complexity of the condition. Yoga can contribute to overall well-being by promoting physical activity, stress reduction, and improved insulin sensitivity. However, diabetes management requires a comprehensive approach, including medication, dietary changes, and regular monitoring. Relying solely on yoga might neglect other essential aspects of diabetes care. It is vital to approach diabetes holistically, incorporating proven medical interventions alongside complementary practices like yoga.
In this video, Dr Sachin Yadav, Consultant physician and diabetologist from Chintamani Hospital, Pune, Maharashtra, explains diabetes and its complications while debunking the misconception that yoga alone can cure diabetes.
Powered by WPeMatico
A recent study highlights the close association between influenza infections and an increased risk of atherothrombotic events, including the acute myocardial infarction (heart attack) and ischemic stroke. The key findings of this study were published in the recent edition of The Journal of Infectious Diseases.
This study utilized a population-based self-controlled case series design and drew individual-level data sourced from electronic registries in the Spain. This study encompassed over 2 million individuals and examined the correlation between influenza infections diagnosed in primary care settings with laboratory-confirmed cases in hospitals with subsequent atherothrombotic events.
The results revealed a sharp increase in the risk of such events among individuals aged 50 years and above in the two weeks following even mild influenza cases. Those with fewer pre-existing risk factors saw their risk double, while the individuals with severe cases faced more than a fourfold increase in risk and persisted at more than twice the baseline risk for up to two months post-infection.
Through meticulous sensitivity analyses, the findings provided compelling evidence that support a causal relationship between influenza infection and atherothrombotic events. This transient yet substantial increase in the risk following influenza infection underlines the need for more vigilant and cautious preventive measures among the high-risk groups.
These findings of this research should reinforce the existing recommendations for influenza prevention, particularly among at-risk populations. The findings of this research highlights the critical importance of influenza prevention efforts in older adults and those with pre-existing health conditions. The relationship between influenza infection and the increased risk of heart attacks and strokes mandates proactive measures to reduce the impact of seasonal influenza.
Source:
Muñoz-Quiles, C., López-Lacort, M., Urchueguía, A., Díez-Domingo, J., & Orrico-Sánchez, A. (2024). Risk of cardiovascular events after influenza: A population-based Self Controlled Case Series study, Spain 2011-2018. In The Journal of Infectious Diseases. Oxford University Press (OUP). https://doi.org/10.1093/infdis/jiae070
Powered by WPeMatico

Princeton: Bristol Myers Squibb has announced that the U.S. Food and Drug Administration (FDA) has accepted the supplemental New Drug Application (sNDA) for Augtyro (repotrectinib) for the treatment of adult and pediatric patients 12 years of age and older with solid tumors that have a neurotrophic tyrosine receptor kinase (NTRK) gene fusion, and are locally advanced or metastatic or where surgical resection is likely to result in severe morbidity.
The filing acceptance is based on results from the registrational Phase 1/2 TRIDENT-1 trial (adult patients with NTRK-positivesolid tumors) and CARE study (pediatric patients with NTRK-positivesolid tumors). The FDA granted the application Priority Review status and assigned a Prescription Drug User Fee Act (PDUFA) goal date of June 15, 2024.
“While great advancements have been made over the last decade, patients with NTRK-positive locally advanced or metastatic solid tumors still experience significant unmet needs. New and effective treatment options that may improve durability of response and address resistance to existing tyrosine kinase inhibitors are critical to helping patients with these aggressive tumors,” said Joseph Fiore, vice president, global program lead, Augtyro, Bristol Myers Squibb. “We look forward to working closely with the FDA on the review of our application for Augtyro for this tumor-agnostic indication and potentially offering patients with NTRK-positive disease a new, durable treatment option.”
The filing was based on the results from the TRIDENT-1 and CARE trials. In the TRIDENT-1 study, Augtyro demonstrated clinically meaningful response rates in patients with NTRK-positive locally advanced or metastatic solid tumors. Durability of response was robust, including among patients whose tumors harbor common resistance mutations, and intracranial responses were observed. Augtyro showed a safety profile that was well tolerated and generally manageable. The study remains ongoing to assess long-term outcomes and additional endpoints. Results from TRIDENT-1 were supported by data from the CARE study, which evaluates Augtyro in pediatric and young adult patients with locally advanced or metastatic solid tumors harboring ALK, ROS1 or NTRK1-3 gene alterations.
Additionally, in November 2023 the U.S. Food and Drug Administration approved Augtyro for the treatment of adult patients with locally advanced or metastatic ROS1-positive non-small cell lung cancer NSCLC.
Turning Point Therapeutics is a wholly owned subsidiary of the Bristol-Myers Squibb Company. As of August 2022, Bristol Myers Squibb acquired the company, including its asset repotrectinib.
Read also: Bristol Myers Squibb concludes acquisition of Mirati Therapeutics
Powered by WPeMatico
Maintaining HbA1c below 7% is vital for individuals with diabetes as it reflects stable blood sugar levels over time. This target is crucial in reducing the risk of complications such as heart disease and kidney issues. Regular monitoring and achieving this goal contribute to effective diabetes management, promoting overall well-being and minimizing the potential for long-term health problems.
Contrary to the popular myth that being a non-vegetarian guarantees immunity from diabetes, it’s crucial to understand that diabetes risk is influenced by various factors. While diet plays a role, genetics, lifestyle, and overall health are significant contributors. Non-vegetarians can develop diabetes if other risk factors are present, such as a sedentary lifestyle or genetic predisposition. A balanced diet, regular exercise, and overall healthy living are essential for diabetes prevention, emphasizing that the type of diet alone doesn’t determine one’s susceptibility to the condition.
In this video, Dr. Suhas Khaire, Consultant Endocrinologist from Pune, Maharashtra discusses HbA1c and the importance of keeping HbA1c levels below 7% while dispelling the myth that a person cannot acquire diabetes if they are non-vegetarian.
Powered by WPeMatico

People using anabolic steroids could be increasing their underlying risk of a heart condition called atrial fibrillation, a new study has found.
The new research published in the Journal of Physiology conducted by an interdisciplinary consortium of clinicians and researchers led by University of Birmingham and collaborators in Germany.
The team found that male sex hormones, such as testosterone, also called androgenic anabolic steroids (AAS), which are misused for muscle building particularly among in young men can increase the risk of atrial fibrillation in individuals genetically predisposed to heart diseases.
Dr Laura Sommerfeld, Postdoctoral Researcher at the UKE Hamburg, who completed her PhD at the Institute of Cardiovascular Sciences at the University of Birmingham focusing on this work is lead author of the study.
Dr Sommerfeld said: “Our study can significantly contribute to understanding the impact on the heart health of young men who misuse anabolic steroids to increase muscle mass. Recent reports have shown that young men in particular are being targeted on social media such as TikTok being sold testosterone products, but we have shown how the misuse of steroids carries a specific risk that many people will not be aware of.”
Professor Larissa Fabritz, Chair of Inherited Cardiac Conditions at UKE Hamburg and Honorary Chair in the Institute of Cardiovascular Sciences at the University of Birmingham added:
“Heart muscle diseases like ARVC affect young, athletic individuals and can lead to life-threatening heart rhythm disturbances. Atrial fibrillation is a common condition in the general population. Elevated testosterone levels can result in an earlier onset of these diseases.”
The scientists examined potential effects on a condition called arrhythmogenic right ventricular cardiomyopathy (ARVC), which is genetically determined and primarily attributed to disruptions in the formation of cell connections critical for heart muscle stability.
The scientists initially confirmed, based on clinical patient data from UHB and elsewhere, that ARVC occurs more frequently and severely in men than in women. In laboratory experiments, they discovered that six weeks of AAS intake, combined with impaired cell connections, could lead to reduced sodium channel function in heart tissue and a slowing of signal conduction within the atria.
Dr Andrew Holmes, co-author and Assistant Professor in the Institute of Clinical Sciences at the University of Birmingham said:
“This work implies that young male individuals with key inherited genetic changes have a greater risk of developing electrical problems in the heart in response to anabolic steroid abuse.”
Reference:
Laura C. Sommerfeld, Andrew P. Holmes, Ting Y. Yu, Christopher O’Shea, Deirdre M. Kavanagh, Jeremy M. Pike, Thomas Wright, Fahima Syeda, Areej Aljehani, Tania Kew, Victor R. Cardoso, S. Nashitha Kabir, Claire Hepburn, Reduced plakoglobin increases the risk of sodium current defects and atrial conduction abnormalities in response to androgenic anabolic steroid abuse, The Journal of Physiology, https://doi.org/10.1113/JP284597.
Powered by WPeMatico
