The complaint was filed on December 14, 2021, before the consumer court against the Hospital (OP 1) and two physicians (Opposite party No.2 Dr Premlatha and 3 Dr Rajaram), a general surgeon, Dr Kumar (Opposite Party No.4) and Rajaji Government Hospital (Opposite Party No.5).
The core of the complaint revolved around the complainant’s wife, who was admitted to Shri Andal Hospital for abdomen pain. The complainant, the husband of deceased patient, brought his wife to the hospital on November 18, 2020, for abdomen pain. The 3rd opposite party physician Dr Rajaram admitted her as an inpatient. On November 19, 2020, the 2nd opposite party physician Dr Premlatha recommended immediate surgery, claiming a cyst in her uterus posed a life-threatening risk. The complainant, persuaded by the 1st physician, agreed to the surgery, initially priced at Rs. 80,000 but settled for Rs. 40,000, with an immediate payment of Rs. 10,000.
The surgery, conducted by Dr Premlatha on November 21, 2020, revealed complications, and additional expenses of Rs. 1,00,000 were demanded. The complainant paid another Rs. 10,000. Subsequently, the services of the 4th opposite party, Dr Kumar were sought. It was at this point that it was realized by the complainant the surgery had been performed negligently without pre-operative tests. Due to the severity of the situation, the patient was shifted to Government Rajaji Hospital, Madurai. The 1st opposite party did not provide medical records but issued a referral letter.
Upon reaching the 5th opposite party, Rajaji Government Hospital on November 22, 2020, they initially refused admission due to the patient’s condition after the incomplete surgery. Later, she was admitted as an inpatient, and the complainant paid Rs. 606 for scan and blood tests. The patient, who had undergone a half-baked colostomy operation, struggled with treatment and ultimately passed away on November 28, 2020. Medical records from the Rajaji Government Hospital revealed that the antecedent cause of death was injury with colostomy.
Aggrieved, the complainant moved the Commission alleging negligence and deficiency in service by the opposite parties, asserting that proper pre-operative investigations could have saved his wife’s life. The complaint sought compensation among other reliefs.
The complainant alleged that the Andal Hospital performed the surgery negligently, puncturing the intestine and causing severe adhesion in the bowel. He claims that proper pre-operative investigation, such as an MRI scan, could have saved his wife’s life. The complainant issued a lawyer’s notice and lodged the complaint, accusing the opposite parties of negligence and deficiency in service.
In response to the consumer complaint, the Rajaji Government Hospital, argued that the complaint is not maintainable as they provide free services, and the complainant did not pay any consideration for the treatment. The hospital contended that they offered proper treatment and there was no negligence on their part.
Deliberating the case, the Commission raised points for consideration that included, whether the consumer complaint against the Rajaji Government Hospital is maintainable; whether the opposite parties have committed any deficiency in service; If so, to what relief the complainant is entitled.
The Commission, after reviewing the written version of the Rajaji Government Hospital, addressed the first point. They concluded that the complaint against the Government Hospital is not maintainable as the hospital provides free services, and the complainant did not pay any consideration for the treatment. The Commission referred to a Supreme Court judgment supporting this stance. Therefore, Point 1 was answered against the complainant, and the complaint against the Rajaji Government Hospital was deemed dismissed.
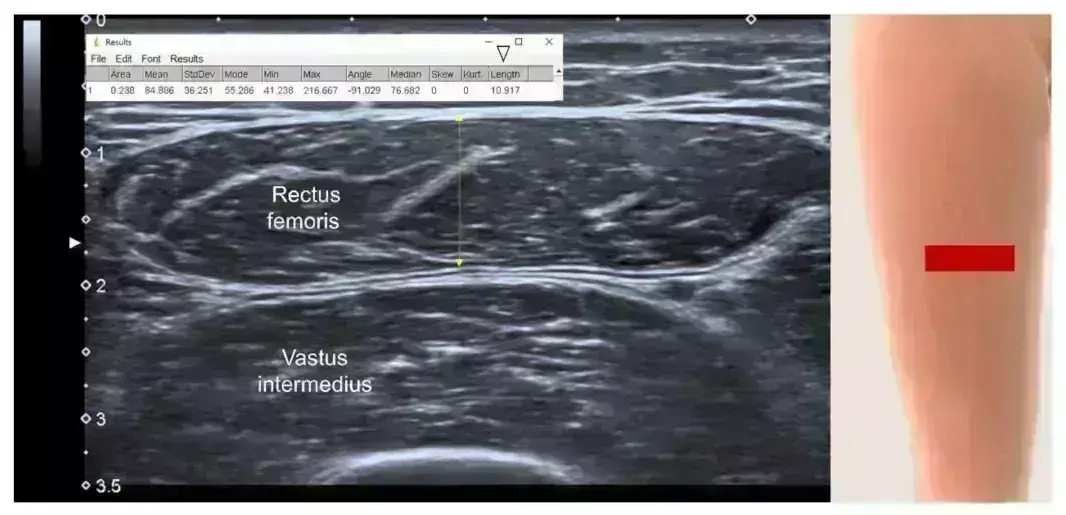
Upon examining the records, the Commission observed that it was evident that the doctors conducted proper pre-operative investigations before the surgery. The Commission emphasized the importance of pre-operative assessment to ensure the patient’s fitness for surgery, identify potential issues, and guarantee patient safety. However, the Commission agreed with the complainant’s argument that the doctors failed to conduct an MRI scan to assess the patient’s condition before the surgery. The Commission deemed the failure to perform pre-operative investigations, including an MRI scan for assessing abdominal adhesions, as gross negligence and a deficiency in service on the part of the physcians. It noted;
“We are of the view that pre-operative assessment is necessary prior to surgical procedures, in order to ensure that the patient is fit to undergo surgery, to highlight issues that the surgical or anaesthetic team need to be aware of during the peri-operative period, and to ensure patients’ safety during their journey of care. In addition, unnecessary complications due to inappropriate surgery may be avoided. In the above circumstances we find force in the contention of the complainant that the opposite parties 1 to 4 have failed to take MRI scan to assess the condition of the patient prior to performing the surgery. We are of the considered view that non-carrying out of pre-operative investigations including MRI Scan for assessing abdominal adhesions in the case in hand amount to gross negligence coupled with deficiency in service on the part of the 2nd and 3rd opposite party.”
The complainant asserted that the Shri andal Hospital failed to provide medical records while referring his wife to the Government Hospital, Madurai, presenting only a referral letter. Referring to a judgment by the HON’BLE NATIONAL COMMISSION, the Commission agreed that non-provision of case sheets is a negligent act. It observed;
“We are of the view that the 1st opposite party act of not providing the case sheet to the complainant at the time of discharging the patient with referral to Government Hospital is an negligent act.”
The complainant argued the case as res ipsa loquitor, citing medical records obtained from the 5th Rajaji Government Hospital. The HON’BLE MADRAS HIGH COURT supports this argument, emphasizing the onus on the medical professionals to prove non-negligence.
The Commission concluded that the Shri Andal Hospital, the physicians and the surgeon failed to discharge their burden, and the complainant was entitled to compensation for careless and negligent treatment. It noted;
“The opposite parties 1 to 4 have failed to discharge their burden on the facts and circumstances of the present case and therefore the complainants are entitled compensation for the damages for the careless and negligent treatment. In auxiliary in the case in hand the complainant had proved and established his case by filing proof affidavit and marking requisite documents and in the absence of any evidence in contra being produced and placed before us by the opposite parties 1 to 4 are inclined to accept the case of the complaint that the opposite parties 1 to 4 are guilty of gross negligence and deficiency in service. Accordingly we answer Point 2 in favour of the complainant.”
The complainant contended that the negligent and nonchalant actions of the Shri Andal Hospital and physicians, lacking professional ethics, resulted in the death of his wife, causing immense mental agony to the family. The Consumer Commission acknowledged that compensation is warranted upon proof of loss or injury due to negligence. It noted;
“In the case in hand negligent act and utter lack of devotion to duty and nonchalant attitude of the opposite parties 1 to 3 in observing even minimum professional ethics and principles had resulted in death of the complainant’s wife which would have definitely resulted in caused acute mental agony, pain and anguish to the complainant and his family members posing a great question mark of the entire family’s future.”
It emphasized the need for a fair, reasonable, and commensurate compensation, considering all relevant factors and following established legal principles. The Commission asserted its duty to assess compensation based on the individual circumstances of each case and the proven loss suffered by the consumer.
In light of established medical negligence leading to the complainant’s loss of his wife, aged around 39 years, the Consumer Commission deemed a compensation of Rs. 10,00,000/- just and fair. The hospital (1st opposite party) was held vicariously liable for the acts of negligence by the treating doctors (opposite parties 2 to 4). Therefore, the 1st opposite party was directed to pay Rs. 10,00,000/- as compensation and Rs. 10,000/- as the cost of the complaint. The complaint against the 5th opposite party was dismissed. The Commission held;
“It is well established that a hospital is vicariously liable for the acts of negligence committed by the doctors engaged or empanelled to provide medical care. It is common experience that when a patient goes to a hospital, he/she goes there on account of the reputation of the hospital, and with the hope that due and proper care will be taken by the hospital authorities. If the hospital fails to discharge their duties through their doctors, being employed on job basis or employed on contract basis, it is the hospital which has to justify the acts of commission or omission on behalf of their doctors. Accordingly, we hold the 1st opposite party to be vicariously liable for the acts of omission and commission committed by the opposite parties 2 to 4 and therefore the 1st opposite party is liable to pay compensation the compensation of Rs. 10,00,000/- to the complainant.”
The hearing took place on November 8, 2023, with legal representation on both sides, while the order was pronounced on November 14, 2023, by the Commission President M. Piraviperumal and Member-I P. Shanmugapriya.
To view the original order, click on the link below: