Inhibiting a problematic protein helps immunotherapies, CAR T-cell therapy to fight off melanoma more effectively
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
Powered by WPeMatico
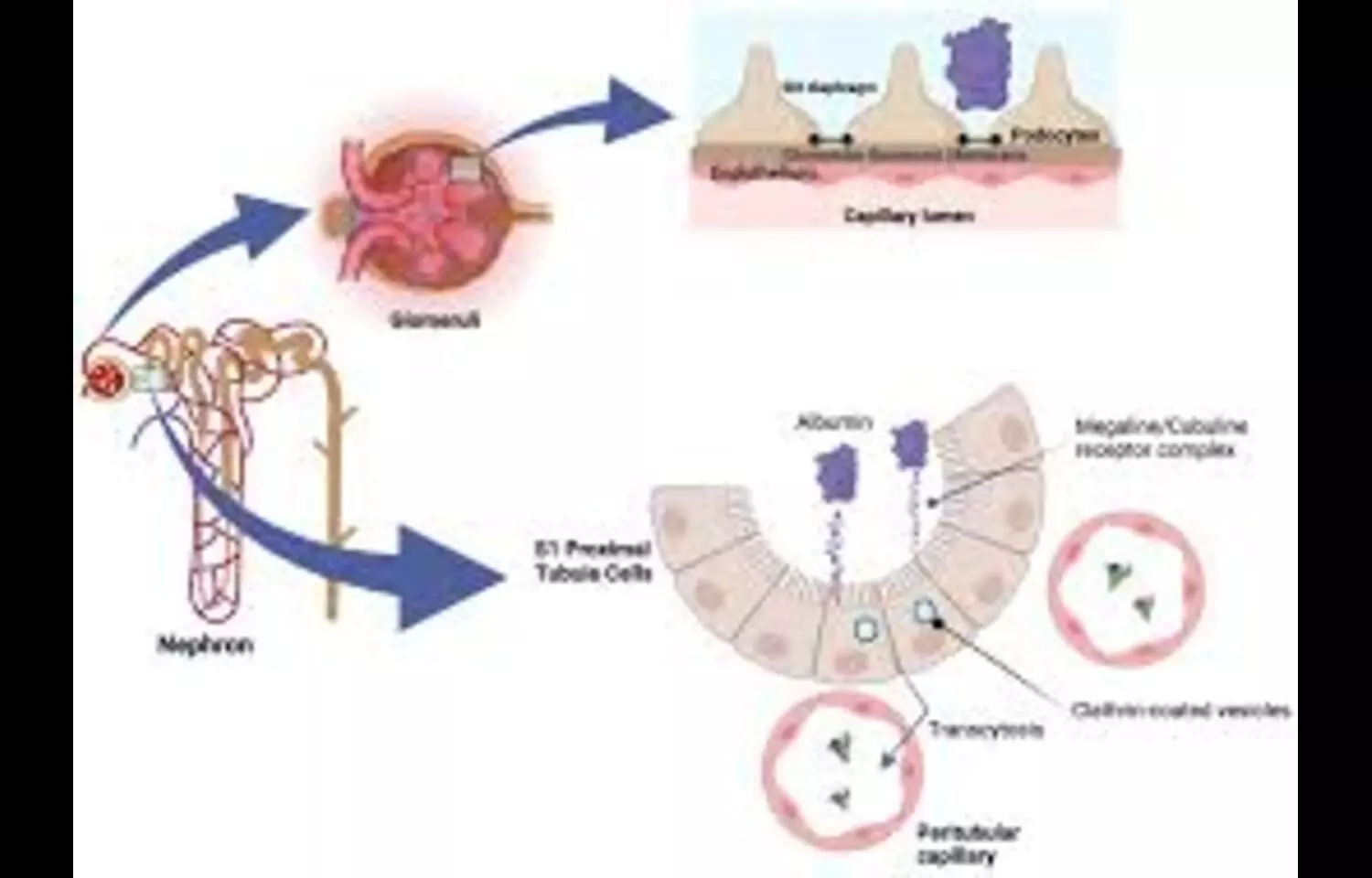
A recent analysis published in BMJ Open Diabetes Research & Care revealed that reducing albuminuria plays a crucial role in improving long-term outcomes for patients living with chronic kidney disease and type 2 diabetes mellitus. The study demonstrated that patients who achieved a sustained decrease of more than thirty percent in the urine albumin-to-creatinine ratio over a period of six to twenty-four months experienced significantly lower risks of death, cardiovascular events, and kidney disease progression. These results highlight that albuminuria is not only a marker of kidney damage but also a modifiable treatment target capable of influencing overall survival.
Powered by WPeMatico

People with both cavities and gum disease may face a higher risk of ischemic stroke, according to a study published on October 22, 2025, in Neurology® Open Access, an official journal of the American Academy of Neurology. The study does not prove that poor oral health causes strokes; it only shows an association.
Ischemic strokes are the most common type of stroke and occur when a clot or blockage reduces blood flow to the brain, depriving it of oxygen and nutrients.
Cavities are holes in the tooth enamel caused by sugary or starchy foods or factors such as poor oral hygiene or genetics. Gum disease, usually caused by poor oral hygiene, is an inflammation or infection of the gums and jawbone. It can lead to tooth loss.
“We found that people with both cavities and gum disease had almost twice the risk of stroke when compared to people with good oral health, even after controlling for cardiovascular risk factors,” said study author Souvik Sen, MD, MS, MPH, of the University of South Carolina in Columbia. “These findings suggest that improving oral health may be an important part of stroke prevention efforts.”
Researchers analyzed data from 5,986 adults with an average age of 63 who had no prior history of stroke at the start of the study. All participants completed dental exams that assessed whether participants had gum disease, cavities or both. Participants were then placed in three groups: having a healthy mouth, gum disease only or gum disease with cavities.
Researchers followed them for two decades, using phone visits and medical records to determine which people had a stroke.
Of 1,640 people with healthy mouths, 4% had a stroke, of 3,151 people with gum disease only, 7% had a stroke and of 1,195 people with gum disease and cavities, 10% had a stroke.
After adjusting for factors such as age, body mass index and smoking status, researchers found when compared to people with healthy mouths, those with both gum disease and cavities had an 86% higher risk of stroke. Those with gum disease alone had a 44% increased risk.
The study also looked more broadly and found that people with both gum disease and cavities had a 36% higher risk of experiencing a major cardiovascular event, such as a heart attack, fatal heart disease or stroke when compared to people with healthy mouths.
Participants who reported visiting the dentist regularly had 81% lower odds of having both gum disease and cavities and 29% lower odds of having gum disease alone.
“This study reinforces the idea that taking care of your teeth and gums isn’t just about your smile; it could help protect your brain,” said Sen. “People with signs of gum disease or cavities should seek treatment not just to preserve their teeth, but potentially to reduce stroke risk.”
A limitation of the study is that participants’ oral health was assessed only once at the start of the study, so changes in dental health over time weren’t captured. It’s also possible that other unmeasured health factors contributed to the findings.
Reference:
Wood, S., et al. (2025). Combined Influence of Dental Caries and Periodontal Disease on Ischemic Stroke Risk. Neurology® Open Access. doi.org/10.1212/wn9.0000000000000036
Powered by WPeMatico
Having lower cholesterol levels may help protect against dementia, according to a large-scale international study led by the University of Bristol. The research, involving data from more than one million participants, found that people with genetic traits that naturally reduce cholesterol are less likely to develop dementia.
The work was led by Dr. Liv Tybjærg Nordestgaard during her time at the University of Bristol and at the Department of Clinical Biochemistry at Copenhagen University Hospital — Herlev and Gentofte. The findings were published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
Some individuals are born with genetic variants that affect the same proteins targeted by cholesterol-lowering medications such as statins and ezetimibe. To explore whether these drugs might influence dementia risk, the team used a technique called Mendelian Randomization. This method allows scientists to study how specific genetic variants mimic the effects of a treatment while minimizing the influence of outside factors like weight, diet, or lifestyle.
By comparing people with and without these cholesterol-lowering genetic variants, the researchers observed a clear difference in dementia risk. A small decrease in cholesterol levels (about one millimole per liter) was associated with up to an 80% reduction in dementia risk for certain drug-related genetic targets.
“What our study indicates is that if you have these variants that lower your cholesterol, it looks like you have a significantly lower risk of developing dementia,” said Dr. Nordestgaard, who now works in the Department of Clinical Biochemistry at Copenhagen University Hospital — Bispebjerg and Frederiksberg hospital.
The results suggest that keeping cholesterol levels low — whether through genetics or medical treatment — may protect against dementia. However, the research does not yet confirm that cholesterol-lowering drugs themselves directly prevent the disease.
Because dementia often develops late in life, studying its causes requires tracking participants for decades. This makes it difficult to establish cause and effect in traditional clinical trials.
It also remains unclear why high cholesterol raises dementia risk. One explanation, according to Dr. Nordestgaard, is that high cholesterol contributes to atherosclerosis — the buildup of fatty deposits in blood vessels.
“Atherosclerosis is a result of the accumulation of cholesterol in your blood vessels,” Dr. Nordestgaard said. “It can be in both the body and the brain and increases the risk of forming small blood clots — one of the causes of dementia.
“It would be a really good next step to carry out randomised clinical trials over 10 or 30 years, for example, where you give the participants cholesterol-lowering medication and then look at the risk of developing dementia,” Dr. Nordestgaard added.
Reference:
Liv Tybjærg Nordestgaard, Aimee Hanson, Eleanor Sanderson, Emma Anderson, Venexia Walker, Anne Tybjærg‐Hansen, George Davey Smith, Børge G. Nordestgaard. Cholesterol‐lowering drug targets reduce risk of dementia: Mendelian randomization and meta‐analyses of 1 million individuals. Alzheimer’s, 2025; 21 (10) DOI: 10.1002/alz.70638
Powered by WPeMatico
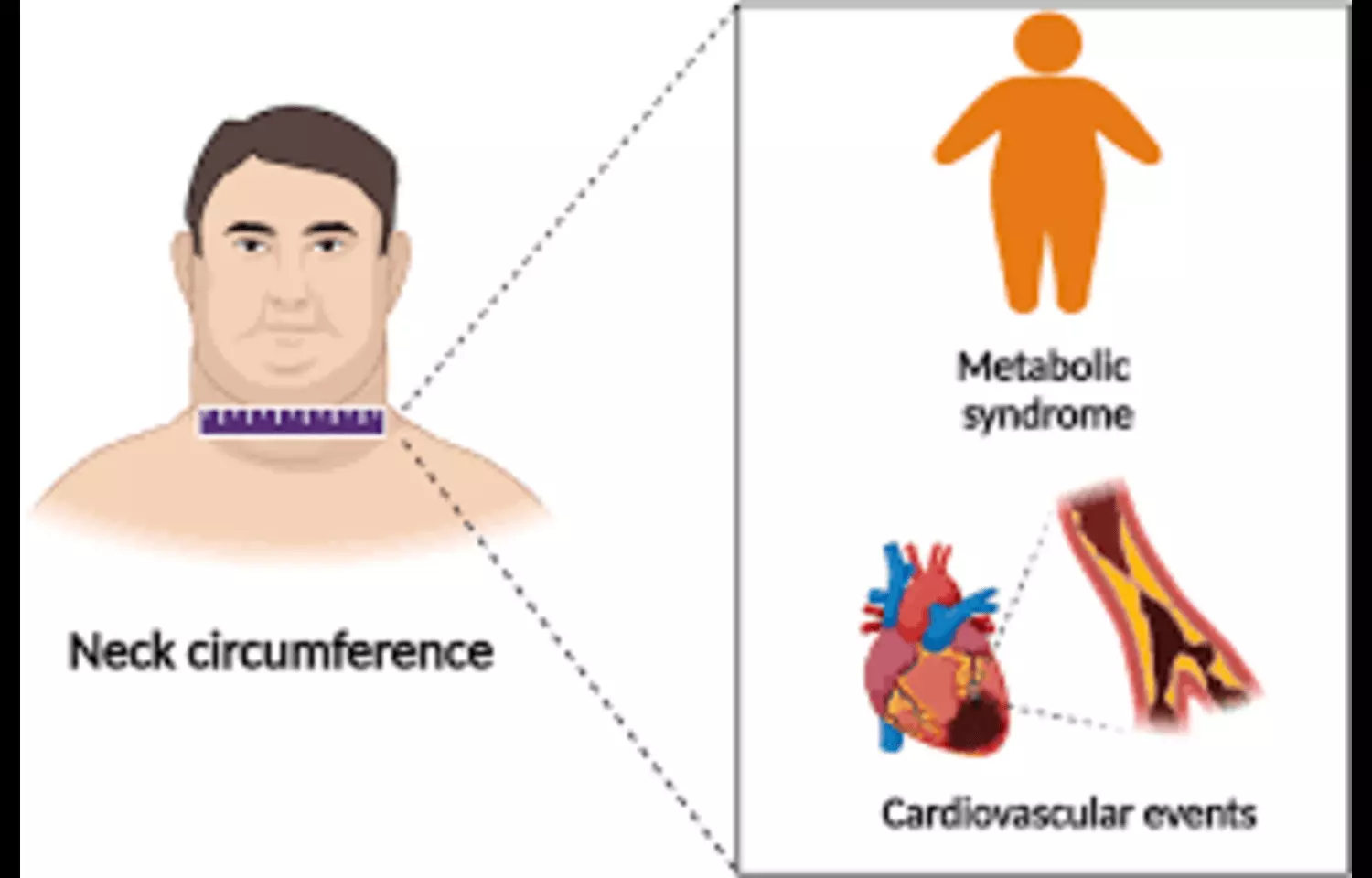
Researchers have found in a new study that neck circumference is significantly associated with components of metabolic syndrome and offers a simple, low-cost, and effective method for screening metabolic risk, particularly useful in resource-limited settings. The study, published in Cureus, evaluated the relationship between neck circumference and various metabolic risk factors, including waist circumference, blood pressure, glucose levels, and lipid profiles. Findings indicated that larger neck circumference correlated strongly with higher prevalence of metabolic syndrome traits, suggesting that this measurement could serve as a practical anthropometric marker for identifying individuals at elevated cardiometabolic risk.
Powered by WPeMatico
